Abstract
Following elective craniotomy, patients routinely receive 24-h monitoring in an intensive care unit (ICU). However, the benefit of intensive care monitoring and treatment in these patients is discussed controversially. This study aimed to evaluate the complication profile of a “No ICU – Unless” strategy and to compare this strategy with the standardized management of post-craniotomy patients in the ICU. Two postoperative management strategies were compared in a matched-pair analysis: The first cohort included patients who were managed in the normal ward postoperatively (“No ICU – Unless” group). The second cohort contained patients routinely admitted to the ICU (control group). Outcome parameters contained detailed complication profile, length of hospital and ICU stay, duration to first postoperative mobilization, number of unplanned imaging before scheduled postoperative imaging, number and type of intensive care interventions, as well as pre- and postoperative modified Rankin scale (mRS). Patient characteristics and clinical course were analyzed using electronic medical records. The No ICU – Unless (NIU) group consisted of 96 patients, and the control group consisted of 75 patients. Complication rates were comparable in both cohorts (16% in the NIU group vs. 17% in the control group; p = 0.123). Groups did not differ significantly in any of the outcome parameters examined. The length of hospital stay was shorter in the NIU group but did not reach statistical significance (average 5.8 vs. 6.8 days; p = 0.481). There was no significant change in the distribution of preoperative (p = 0.960) and postoperative (p = 0.425) mRS scores in the NIU and control groups. Routine postoperative ICU management does not reduce postoperative complications and does not affect the surgical outcome of patients after elective craniotomies. Most postoperative complications are detected after a 24-h observation period. This approach may represent a potential strategy to prevent the overutilization of ICU capacities while maintaining sufficient postoperative care for neurosurgical patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Following elective craniotomy, neurosurgical patients are routinely admitted to the ICU for a 24-h observation period to rule out early postoperative complications. These are thought to most commonly occur on the first postoperative day and include hemorrhage, liquor circulation disorders, seizures, and acute ischemic strokes [6]. Postoperative care in the ICU allows rapid recognition of neurologic deterioration or accurate hemodynamic assessment. However, there is no scientific evidence for the benefit of intensive medical monitoring in patients after elective intracranial procedures [5,6,7]. More likely, only a small portion of neurosurgical patients require invasive monitoring and intensive care interventions [3, 6]. Especially during the coronavirus disease-19 (COVID-19) pandemic, ICU capacities have become a critical medical resource with increasing relevance for the routine postoperative ICU care of neurosurgical patients [1, 10, 11].
Consequently, this study aimed to compare the concept of routine ICU admission in patients undergoing elective craniotomy with the concept of providing intensive care only for selected cases with potentially complicated courses during restrictions to ICU capacities and personnel induced by the COVID-19 pandemic.
Methods
Patients
We retrospectively identified all patients aged 18 years and older undergoing elective craniotomy and transnasal/transsphenoidal resection in our institution between February and August 2021.
The control group consisted of adult patients (> 18 years old) undergoing elective craniotomies as well as transnasal/transsphenoidal approaches between February and May 2021. During this period, all patients undergoing elective craniotomies were referred to the ICU postoperatively for 24 h as standard procedure.
From May 2021, the standard procedure for postoperative monitoring in our institute was changed to the “No ICU – Unless” concept as published previously [7]. Patients in this “No ICU – Unless” group (NIU group) were automatically planned for postoperative observation in the neurosurgical normal ward following a short period (approximately 1–2 h) in the post-anesthesia care unit unless one or more of the following preoperative criteria were fulfilled (No ICU – Unless criteria). In this scenario, patients were planned for postoperative management in the ICU:
-
1)
Neurological and neurosurgical criteria: Tumors of the posterior fossa larger than 3 cm diameter; affection of lower cranial nerves with (potential for) dysphagia and aspiration; altered level of consciousness before surgery.
-
2)
Anesthesiologic criteria: Cardiopulmonary or hemodynamic risk factors determined by the managing anesthesiologist, such as an American Society of Anesthesiology (ASA) score of 4 or higher, coagulation disorders, or difficult airways.
In case of high intraoperative blood loss (more than two liters), the occurrence of intraoperative complications, prolonged surgical time (more than four hours) or other anesthesiologic concerns [6], patients were admitted to the ICU even if they were initially intended for the normal ward.
Patients under 18 years of age and those undergoing emergency treatment were excluded from our analysis. Also, patients undergoing tumor biopsies were not included in our analysis.
Data collection
Electronic medical records were used to collect patient demographics, anesthesiology documentation, intraoperative, and imaging data. In particular, we recorded surgical time, catecholamine doses, blood loss, intraoperative complications (surgical complications, seizures, intraoperative neuromonitoring break-offs, cardiac complications), total length of stay in the hospital, length of stay in the ICU, time to first postoperative mobilization, and numbers of unscheduled imaging prior to scheduled postoperative imaging. When applicable, we recorded ICU treatment received (blood pressure medication/circulation support, prolonged ventilation, observation/monitoring alone).
Finally, postoperative complications were recorded in detail. Clinically significant complications were determined as hemorrhage, acute ischemic stroke, seizure, edema, hydrocephalus, pulmonary embolism, cerebrospinal fluid (CSF) fistula, or other complications that required surgery, (re-) transfer to the ICU, or any medical intervention. Time of occurrence of complications was also noted during the period of hospital stay. Unexpected events that did not require treatment or had no practical consequences were not included in the analysis. Only in-hospital complications were analyzed.
Statistical analysis
Data analysis was performed with Excel (version 14.7.7; Microsoft) and SPSS (version 28.0; IBM Corp). Group comparisons were performed using the Mann–Whitney U test. Fisher’s exact test was used for the comparison of categorical variables. Results of p ≤ 0.05 were considered statistically significant.
Results
Patient characteristics
In total, 171 patients were evaluated between February and August 2021. A total of 96 patients were included in the NIU group, and 75 patients were referred to the control group.
The median age of the NIU and control groups was 55 years (range of NIU group: 19–81 years; range of control group: 24–81 years; p = 0.171). The NIU group included 57 male (59%) and 39 (41%) female patients, and the control group contained 32 (43%) male and 43 (57%) female patients (p = 0.083).
The NIU group contained more patients (9%) with an ASA score of 4 versus 3% in the control group, which was not statistically significant (p = 0.055). The most common diagnosis in both groups was an intracranial tumor (84% in the NIU group, 81% in the control group), most commonly with a supratentorial localization (88% in both groups), followed by vascular pathologies (12% in the NIU group, 9% in the control group). No statistically significant differences in the distribution of age, gender, ASA score, diagnosis, and localization of the lesion were detected between groups (Table 1).
Among patients in the NIU group, 42 (44%) were transferred to the normal ward and 54 (56%) patients were admitted to the ICU; 37 patients (39%) were initially scheduled for ICU, and 17 (18%) were unscheduled, but ultimately required, transfer to the ICU as decided within the course of surgery. In the control group, 14 patients (19%) were directly admitted to the normal neurosurgical ward after surgery (resection of pituitary tumors via a transnasal/transsphenoidal approach or open biopsies) and 61 patients (81%) were admitted to the ICU (Table 2).
Retrospective analysis of the control group showed that 39% of patients would have fulfilled the NIU criteria for observation in the ICU, with 61% having been transferred to the normal ward instead of ICU observation (Fig. 1).
Application of No ICU – Unless criteria in the control group. The figure represents the proportions of patients in the control group which would have met and not met the NIU criteria; 39% of patients would have met the NIU criteria for observation in the ICU versus 61% who could have been observed in the normal ward
Intraoperative parameters
Intraoperative parameters in the NIU and control groups were examined (Table 3). Median length of surgery in minutes (157; range 21–358 vs. 181; range 279–470; p = 0.369), blood loss in milliliters (300; range 10–1500 vs. 325; range 10–1000; p = 0.726), intraoperative catecholamines in µg/kg/min (0.06; range 0.00–0.20 vs. 0.08; range 0.00–0.25; p = 0.840), and number of intraoperative complications (8/96; 8% vs. 3/75; 4%; p = 0.73). Intraoperative complications occurring in the NIU group included cardiac arrhythmia in five cases (0,05%), vessel injury or aneurysm rupture in two cases (0,02%), and one intraoperative seizure (0,01%). Intraoperative complications within the control group included cardiac arrhythmia in two cases (0,03%) and loss of intraoperative neuromonitoring signals in one case (0,01%). All intraoperative parameters showed no statistically significant differences (Table 3).
Inpatient stay
Overall length of stay in hospital
Patients in the NIU group had an overall shorter stay in the hospital compared to the control group (average 5.8 ± 4.6 vs. 6.8 ± 3.7 days; p = 0.661; Table 4). Patients from the NIU group whose admission to the ICU was unscheduled had an overall hospital stay of 6.0 (± 4.7) days which was comparable to the subgroup of NIU patients that were scheduled for postoperative ICU admission (average 6.1 ± 4.7; p = 0.571; Table 4).
Length of stay in ICU
Overall, patients in the NIU group spent less time in the ICU following surgery than the control group (average 0.9 ± 1.8 vs. 1.4 ± 2.1 days; p = 0.414; Table 3). Patients from the NIU group who were scheduled for ICU admission following surgery spent the same time in the ICU as those with unscheduled admission (average 1 ± 1.9 days; p = 0.667; Table 4).
Time to first postoperative mobilization
There was no difference between groups in time to mobilization (average 0.9 ± 1.6 days in the NIU group vs. 1.1 ± 1.2 days in the control group; p = 0.402; Table 4).
Number of unscheduled imaging
11/96 patients (11%) received unscheduled imaging (computed tomography (CT) or magnetic resonance imaging (MRI)) within the NIU group prior to their otherwise scheduled postoperative imaging. One patient received two CTs prior to scheduled imaging; 9/75 patients (12%) received CT scans prior to scheduled MRI or CT scan within the control group. One of these patients received two unscheduled CT scans. Within the control group, ten unscheduled scans were conducted (13%); within the NIU group, eleven scans were initiated prior to scheduled imaging (11%). Overall, cohorts did not differ significantly in the number of unplanned CT/MRI scans (p = 0.67; Table 4).
ICU treatment
In the NIU group, 11/96 patients (11%) received treatment in the ICU and 43 were observed without intervention. In the control group, 15/75 patients (20%) received treatment in the ICU and 46/61 were observed without intervention.
No statistically significant differences were found between the type of interventions in ICU in the NIU group and control group: anti-hypertensive therapy in 4 (5%) patients in vs. 5 (6%) patients (p = 0.825); catecholamine therapy in 6 (8%) patients vs. in 3 (3%) patients (p = 0.591); ventilation in 5 (7%) patients vs. 3 (3%) patients (p = 0.552).
In both groups, intravenous blood pressure management was the most frequent type of treatment in post-craniotomy patients (Table 5).
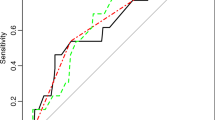
Early postoperative complications
Incidence of early postoperative complications during the postoperative inpatient hospital stay within the NIU and control groups showed no significant differences (15/96; 16% vs. 13/75; 17%; p = 0.786; Fig. 2). Further analysis of the time point at which complications occurred, either before or after the first 24 h following surgery, showed that most complications in both NIU and control groups occurred after the first 24 h postoperatively (67% in the NIU group and 54% in the control group).
Postoperative complications.Percentage of the total cohort of postoperative complications subdivided into early (< 24 h after surgery) and late (> 24 h after surgery). (a) NIU group: of the 16% overall complication rate, 33% occurred within the first 24 h following surgery with the remaining complications occurring after 24 h. (b) Control group: the overall complication rate was 17%; 46% of these complications occurred within the first 24 h following surgery and 54% occurred after 24 h postoperatively
In the NIU group, 7/15 (46%) of the complications occurred in the normal ward, with one patient suffering two early postoperative complications (hemorrhage and stroke). In the control group, 6/13 (46%) complications occurred in the normal ward.
One patient suffered two complications during the inpatient stay (seizure and stroke).
Surgical intervention was required in 9/15 (60%) of complications occurring in the NIU group (five evacuations of hemorrhage, two implantations of external ventricular drains, and one re-resection due to space-consuming residual hemorrhaging tumor mass).
Within the control group, 3/13 (23%) complications required surgical intervention (two evacuations of hemorrhage and one re-resection due to space-consuming residual tumor mass).
A detailed summary of all postoperative complications is found in Table 6 and Table 7.
Pre- and postoperative mRS
There was no significant change in the distribution of preoperative (p = 0.960) and postoperative (p = 0.425) mRS scores in the NIU group and the control group with the majority of patients in both groups having a pre- and postoperative mRS score of 1 (Fig. 3).
Discussion
Results of the current study demonstrate that postoperative management of elective cranial neurosurgical procedures is safe with a comparable complication and risk profile compared to standard postoperative ICU management. Most complications occurred later than 24 h following surgery, in which case patients are usually already on the regular ward. Outcome analysis at discharge from the hospital found that the “No ICU – Unless” concept resulted in comparable mRS distribution compared to the control group which underwent automatic postoperative ICU observation.
Postoperative care in patients undergoing elective craniotomy
The results of this study support previous findings in screening post-craniotomy patients for the need for ICU admission. Bui et al. [3] compared routine ICU admission to normal ward admission in 343 patients after elective craniotomy and identified long duration of surgery, anesthesiologic risks, and high intraoperative blood loss as predictors for required ICU admission. A further retrospective study including 400 patients identified advanced age and diabetes as independent predictors for necessary postoperative ICU monitoring [6]. Overall, no study could reveal routine ICU admission in all postoperative patients as significantly beneficial for in-hospital morbidity and mortality [2,3,4, 6, 7].
Despite the reduction of automatic postoperative transfers to the ICU within the NIU group, implementing the “No ICU – Unless” concept does not entirely exclude the a priori allocation of selected patients to the ICU following surgery. To date, evidence-based solid criteria that can effectively identify patients who would most profit from postoperative ICU observation do not exist. Our study identifies patients who will require ICU observation based on pragmatic criteria which can guide neurosurgeons and anesthesiologists in daily practice.
First, we initiate ICU observation in patients undergoing resection of large infratentorial lesions, as the previous series have shown that up to 43% of these patients required re-transfer to the ICU from the normal ward and approximately 4% required re-intubation [2]. Furthermore, lesions affecting lower cranial nerves may promote dysphagia and aspiration, so we routinely transfer patients with such lesions to the ICU [6]. Finally, patients with altered levels of consciousness prior to surgery were also routinely transferred to the ICU to observe and react to persisting or worsening neurological deficits.
In our study, the common reasons for unscheduled ICU admission within our “No ICU – Unless” group included intraoperative complications (8/96 patients) and unforeseeable prolonged surgical time (4/96 patients). Hanak et al. [6] identified intravenous blood pressure management as the most frequent type of ICU treatment modality, as it was also found in both of our cohorts. Most patients received observation and monitoring alone after being admitted to the ICU (45% of all patients within the NIU group).
Early postoperative complications
In our analysis, most complications occurred after the transfer of the patient to the normal ward after 24 h of observation (67%). More importantly, the incidence of complications did not increase after introducing the “No ICU – Unless” policy (16% in the NIU group vs. 17% in the control group; p = 0.786). These observations are in line with previously reported data on postoperative complications [8]. Importantly, no increase in complications has been described when patients were managed in the normal ward after surgery [7]. One study reported a statistically significant reduction of the complication rate from 0.98 to 0.53 per patient after changing the management of post-craniotomy patients to a normal ward setting [7].
The most common postoperative complication requiring surgical intervention in both the NIU and control groups was postoperative hematoma (9% in the NIU group and 7% in the control group; in both groups, 7% of all hematomas required surgical intervention).
Between both groups, three hemorrhages occurred within the first 24 h after surgery. The rate of postoperative hematoma following elective craniotomy has been reported to reach 1–4%; of these, only 2,1% required operative evacuation in the first 30 days after surgery [8]. Analysis of a series of 50 postoperative hematomas [12] revealed that 44 occurred within the first six hours after surgery. Six (12%) hemorrhages occurred later than 24 h. A further study found 16% of neurologic complications in 168 post-craniotomy patients, with 85% of complications occurring in the first two hours after surgery [9].
Taken together, 24-h observation and monitoring in the ICU to rule out early postoperative complications, most likely hemorrhage, may not be considered effective as only 1,7% of postoperative hemorrhages in our study occurred within 24 h. Observation up to a 6-h recovery room may also be sufficient [1,2,3, 5, 7, 8, 10, 11].
ICU capacity in times of COVID-19
According to the German Intensive Care Unit Register (DIVI), the capacity of available ICU beds in Germany decreased from approximately 12.000 at the beginning of the pandemic in March 2020 to approximately 2.200 during the fourth wave of the pandemic in November 2021 [4]. As this pandemic is ongoing, strategies for ICU capacity management are more critical than ever. The concept of “No ICU – Unless” may therefore not only serve as a clinically relevant postsurgical management strategy for neurosurgical patients but may also assist in relieving strain on the healthcare system.
Limitations of our study include the single-center, retrospective design, limiting the ability to generalize these initial results to other centers. Further studies should include a multicentric evaluation of the “No ICU – Unless” concept and include long-term follow-up in centers which have also been heavily impacted by pandemic-associated limitations in order to validate the results of our single-center analysis.
Conclusion
We found that routine postoperative ICU management does not reduce postoperative complications and has no effect on the surgical outcome of patients after elective craniotomies. Most postoperative complications were detected after a 24-h observation period. This approach may represent a potential strategy to prevent the overutilization of ICU capacities while maintaining sufficient postoperative care for neurosurgical patients. In our experience, the preoperative assessment of patients for postoperative ICU admission should be a team-based decision of experienced neurosurgeons and anesthesiologists in which comorbidities should be considered.
Data availability
Not applicable.
Change history
10 February 2023
A Correction to this paper has been published: https://doi.org/10.1007/s10143-023-01959-9
References
Anderson RM, Heesterbeek H, Klinkenberg D, Hollingsworth TD (2020) How will country-based mitigation measures influence the course of the COVID-19 epidemic? Lancet 395(10228):931–934. https://doi.org/10.1016/S0140-6736(20)30567-5
Badenes R, Prisco L, Maruenda A, Taccone FS (2017) Criteria for intensive care admission and monitoring after elective craniotomy. Curr Opin Anaesthesiol 30(5):540–545. https://doi.org/10.1097/ACO.0000000000000503
Bui JQH, Mendis RL, van Gelder JM, Sheridan MMP, Wright KM, Jaeger M (2011) Is postoperative intensive care unit admission a prerequisite for elective craniotomy? J Neurosurg 115(6):1236–1241. https://doi.org/10.3171/2011.8.JNS11105
DIVI. Deutsche interdisziplinäre Vereinigung für Intensiv- und Notfallmedizin. https://www.intensivregister.de/#/aktuellelage/zeitreihen. Accessed 29 Nov 2021
Florman JE, Cushing D, Keller LA, Rughani AI (2017) A protocol for postoperative admission of elective craniotomy patients to a non-ICU or step-down setting. J Neurosurg 127(6):1392–1397. https://doi.org/10.3171/2016.10.JNS16954
Hanak BW, Walcott BP, Nahed BV, Muzikansky A, Mian M, Kimberly W, Curry W (2014) Postoperative intensive care unit requirements after elective craniotomy. World Neurosurg 81(1):165–172. https://doi.org/10.1016/j.wneu.2012.11.068
Laan M, Roelofs S, Van Huet I, Adang EMM, Bartels RHMA (2020) Selective intensive care unit admission after adult supratentorial tumor craniotomy: complications, length of stay, and costs. Neurosurgery 86(1):E54–E59. https://doi.org/10.1093/neuros/nyz388
Lassen B, Helseth E, Rønning P, Scheie D, Johannesen T, Mæhlen J, Langmoen I et al (2011) Surgical mortality at 30 days and complications leading to recraniotomy in 2630 consecutive craniotomies for intracranial tumors. Neurosurgery 68(5):1259–1269. https://doi.org/10.1227/NEU.0b013e31820c0441
Lonjaret L, Guyonnet M, Berard E, Vironneau M, Peres F, Sacrista S, Ferrier A et al (2017) Postoperative complications after craniotomy for brain tumor surgery. Anaesth Crit Care Pain Med 36(4):213–218. https://doi.org/10.1016/j.accpm.2016.06.012
Schmidt F, Hauptmann C, Kohlenz W et al (2021) Tackling the waves of COVID-19: a planning model for intrahospital resource allocation. Front Health Serv 1:718668. https://doi.org/10.3389/frhs.2021.718668
Sharma R, Garg K, Katiyar V et al (2021) Analysis of neurosurgical cases before and during the coronavirus disease 2019 pandemic from a tertiary-care centre in India. World Neurosurg 152:e635–e644. https://doi.org/10.1016/j.wneu.2021.06.019
Taylor WAS, Wellings JA (1995) Timing of postoperative intracranial hematoma development and implications for the best use of neurosurgical intensive care. J Neurosurg 82:6
Funding
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Contributions
Conception and design: Czabanka, Lucia, Qasem, Al-Hilou. Acquisition of data: Qasem, Al-Hilou, Lucia. Analysis and interpretation of data: Lucia, Qasem, Al-Hilou. Drafting the article: Qasem, Al-Hilou, Lucia. Critically revising the article: all authors. Reviewed submitted version of manuscript: Qasem, Lucia. Approved the final version of the manuscript on behalf of all authors: Czabanka, Lucia. Statistical analysis: Lucia. Administrative/technical/material support: Czabanka, Lucia. Study supervision: Czabanka, Lucia.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Ethical approval was obtained from the Ethics Committee of the University Hospital Frankfurt am Main, Germany (Identification Number: 2021:550). Due to the retrospective design, informed consent of patients was not required.
Consent for publication
All authors critically reviewed the article and gave written consent for publication.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this article was revised:
The authors regret that in the original article Kristin Lucia and Marcus Czabanka were recognized as shared corresponding authors, however the status of co-senior author was not noted. As such, Kristin Lucia and Marcus Czabanka are both co-corresponding and co-senior authors.
The original article has been corrected.
Kristin Lucia and Marcus Czabanka share senior authorship.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Qasem, LE., Al-Hilou, A., Zacharowski, K. et al. Implementation of the “No ICU – Unless” approach in postoperative neurosurgical management in times of COVID-19. Neurosurg Rev 45, 3437–3446 (2022). https://doi.org/10.1007/s10143-022-01851-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10143-022-01851-y