Abstract
Purpose of Review
With recent advances in sequencing technologies and increasing research into the gut microbiome (GMB), studies have revealed associations between the GMB and urinary stone disease (USD). We sought to determine whether the evidence pointed towards a few specific gut bacteria or the broader GMB network is seemingly responsible for this relationship.
Recent Findings
Initially, Oxalobacter formigenes (OF) was pursued as the main link between GMB and USD given its ability to degrade oxalate in the gut. However, the latest studies consistently suggest that the entire GMB is much more likely to be involved in handling oxalate absorption and other risk factors for urinary stone formation, rather than just a few microbiota.
Summary
The GMB has complex networks that are likely involved in the pathophysiology of USD, although the causal mechanisms remain unclear. With increasing interest and research, potential modalities that act on the GMB may help to prevent incidence of USD.
Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Scales CD Jr, Smith AC, Hanley JM, Saigal CS. Urologic diseases in America P. Prevalence of kidney stones in the United States. Eur Urol. 2012;62(1):160–5. https://doi.org/10.1016/j.eururo.2012.03.052.
Sokolowska M, Frei R, Lunjani N, Akdis CA, O'Mahony L. Microbiome and asthma. Asthma Res Pract. 2018;4(1). https://doi.org/10.1186/s40733-017-0037-y.
Knoll RL, Forslund K, Kultima JR, Meyer CU, Kullmer U, Sunagawa S, et al. Gut microbiota differs between children with inflammatory bowel disease and healthy siblings in taxonomic and functional composition: a metagenomic analysis. Am J Physiol Gastrointest Liver Physiol. 2017;312(4):G327–G39. https://doi.org/10.1152/ajpgi.00293.2016.
Butto LF, Haller D. Dysbiosis in Crohn’s disease - joint action of stochastic injuries and focal inflammation in the gut. Gut Microbes. 2017;8(1):53–8. https://doi.org/10.1080/19490976.2016.1270810.
Wang Z, Klipfell E, Bennett BJ, Koeth R, Levison BS, Dugar B, et al. Gut flora metabolism of phosphatidylcholine promotes cardiovascular disease. Nature. 2011;472(7341):57–63. https://doi.org/10.1038/nature09922.
Turnbaugh PJ, Ley RE, Mahowald MA, Magrini V, Mardis ER, Gordon JI. An obesity-associated gut microbiome with increased capacity for energy harvest. Nature. 2006;444(7122):1027–31. https://doi.org/10.1038/nature05414.
Everard A, Cani PD. Diabetes, obesity and gut microbiota. Best Pract Res Clin Gastroenterol. 2013;27(1):73–83. https://doi.org/10.1016/j.bpg.2013.03.007.
Larsen N, Vogensen FK, van den Berg FW, Nielsen DS, Andreasen AS, Pedersen BK, et al. Gut microbiota in human adults with type 2 diabetes differs from non-diabetic adults. PLoS One. 2010;5(2):e9085. https://doi.org/10.1371/journal.pone.0009085.
Vrieze A, Van Nood E, Holleman F, Salojarvi J, Kootte RS, Bartelsman JF, et al. Transfer of intestinal microbiota from lean donors increases insulin sensitivity in individuals with metabolic syndrome. Gastroenterology. 2012;143(4):913–6 e7. https://doi.org/10.1053/j.gastro.2012.06.031.
Hess B. Metabolic syndrome, obesity and kidney stones. Arab J Urol. 2012;10(3):258–64. https://doi.org/10.1016/j.aju.2012.04.005.
Lee JA, Abramowitz MK, Kipperman N, Drzewiecki BA, Melamed ML, Stern JM. Exploring the association of asthma with urinary stone disease: results from the National Health and Nutrition Examination Survey 2007-2014. Eur Urol Focus. 2018. https://doi.org/10.1016/j.euf.2018.07.035.
Siener R, Bangen U, Sidhu H, Honow R, von Unruh G, Hesse A. The role of Oxalobacter formigenes colonization in calcium oxalate stone disease. Kidney Int. 2013;83(6):1144–9. https://doi.org/10.1038/ki.2013.104.
Holmes RP, Knight J, Assimos DG. Lowering urinary oxalate excretion to decrease calcium oxalate stone disease. Urolithiasis. 2016;44(1):27–32. https://doi.org/10.1007/s00240-015-0839-4.
Kartha GK, Li I, Comhair S, Erzurum SC, Monga M. Co-occurrence of asthma and nephrolithiasis in children. PLoS One. 2017;12(1):e0168813. https://doi.org/10.1371/journal.pone.0168813.
• Miller AW, Dale C, Dearing MD. Microbiota diversification and crash induced by dietary oxalate in the mammalian herbivore Neotoma albigula. mSphere. 2017;2(5). https://doi.org/10.1128/mSphere.00428-17 An experimental study of metabolism of dietary oxalate in an animal model. This study examined the stability of diverse microbiomes in relation to metabolism of dietary oxalate. Its findings suggested that more diverse networks of microbiota were resistant to destabilization.
Mehta M, Goldfarb DS, Nazzal L. The role of the microbiome in kidney stone formation. Int J Surg. 2016;36(Pt D):607–12. https://doi.org/10.1016/j.ijsu.2016.11.024.
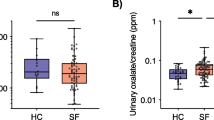
Stern JM, Moazami S, Qiu Y, Kurland I, Chen Z, Agalliu I, et al. Evidence for a distinct gut microbiome in kidney stone formers compared to non-stone formers. Urolithiasis. 2016;44(5):399–407. https://doi.org/10.1007/s00240-016-0882-9.
Tropini C, Earle KA, Huang KC, Sonnenburg JL. The gut microbiome: connecting spatial organization to function. Cell Host Microbe. 2017;21(4):433–42. https://doi.org/10.1016/j.chom.2017.03.010.
• Tang R, Jiang Y, Tan A, Ye J, Xian X, Xie Y, et al. 16S rRNA gene sequencing reveals altered composition of gut microbiota in individuals with kidney stones. Urolithiasis. 2018;46(6):503–14. https://doi.org/10.1007/s00240-018-1037-y This study looked at 13 stone formers with 13 healthy matched controls demonstrated decreased beta diversity amongst stone formers suggesting a unique profile for this cohort compared to controls.
• Ticinesi A, Milani C, Guerra A, Allegri F, Lauretani F, Nouvenne A, et al. Understanding the gut-kidney axis in nephrolithiasis: an analysis of the gut microbiota composition and functionality of stone formers. Gut. 2018;67:2097–106. https://doi.org/10.1136/gutjnl-2017-315734. This study of stool samples from 52 stone formers and 48 controls discovered that the abundance of five microbial taxa was associated with 24-h oxalate excretion, which further points towards a direct role for complex microbiota networks in the pathogenesis of stone formation.
Prien EL, Prien EL Jr. Composition and structure of urinary stone. Am J Med. 1968;45(5):654–72.
Szendroi A, Torde A, Vargha J, Banfi G, Horvath A, Horvath C, et al. Role of the diet in urinary stone formation and prevalence. Orv Hetil. 2017;158(22):851–5. https://doi.org/10.1556/650.2017.30747.
Knight J, Assimos DG, Callahan MF, Holmes RP. Metabolism of primed, constant infusions of [1,2-(1)(3)C(2)] glycine and [1-(1)(3)C(1)] phenylalanine to urinary oxalateMetabolism. 2011;60(7):950–6. https://doi.org/10.1016/j.metabol.2010.09.002.
Freel RW, Whittamore JM, Hatch M. Transcellular oxalate and Cl-absorption in mouse intestine is mediated by the DRA anion exchanger Slc26a3, and DRA deletion decreases urinary oxalate. Am J Physiol Gastrointest Liver Physiol. 2013;305(7):G520–7. https://doi.org/10.1152/ajpgi.00167.2013.
Knauf F, Ko N, Jiang Z, Robertson WG, Van Itallie CM, Anderson JM, et al. Net intestinal transport of oxalate reflects passive absorption and SLC26A6-mediated secretion. J Am Soc Nephrol. 2011;22(12):2247–55. https://doi.org/10.1681/asn.2011040433.
Jiang Z, Asplin JR, Evan AP, Rajendran VM, Velazquez H, Nottoli TP, et al. Calcium oxalate urolithiasis in mice lacking anion transporter Slc26a6. Nat Genet. 2006;38(4):474–8. https://doi.org/10.1038/ng1762.
Yao JJ, Bai S, Karnauskas AJ, Bushinsky DA, Favus MJ. Regulation of renal calcium receptor gene expression by 1,25-dihydroxyvitamin D3 in genetic hypercalciuric stone-forming rats. J Am Soc Nephrol. 2005;16(5):1300–8. https://doi.org/10.1681/asn.2004110991.
Hatch M, Cornelius J, Allison M, Sidhu H, Peck A, Freel RW. Oxalobacter sp. reduces urinary oxalate excretion by promoting enteric oxalate secretion. Kidney Int. 2006;69(4):691–8. https://doi.org/10.1038/sj.ki.5000162.
Arvans D, Jung YC, Antonopoulos D, Koval J, Granja I, Bashir M, et al. Oxalobacter formigenes-derived bioactive factors stimulate oxalate transport by intestinal epithelial cells. J Am Soc Nephrol. 2017;28(3):876–87. https://doi.org/10.1681/ASN.2016020132.
Hatch M, Gjymishka A, Salido EC, Allison MJ, Freel RW. Enteric oxalate elimination is induced and oxalate is normalized in a mouse model of primary hyperoxaluria following intestinal colonization with Oxalobacter. Am J Physiol Gastrointest Liver Physiol. 2011;300(3):G461–9. https://doi.org/10.1152/ajpgi.00434.2010.
Kaufman DW, Kelly JP, Curhan GC, Anderson TE, Dretler SP, Preminger GM, et al. Oxalobacter formigenes may reduce the risk of calcium oxalate kidney stones. J Am Soc Nephrol. 2008;19(6):1197–203. https://doi.org/10.1681/ASN.2007101058.
•• Milliner D, Hoppe B, Groothoff J. A randomised Phase II/III study to evaluate the efficacy and safety of orally administered Oxalobacter formigenes to treat primary hyperoxaluria. Urolithiasis. 2017. https://doi.org/10.1007/s00240-017-0998-6 A phase 3 clinical trial of 36 patients that demonstrated the use of oral Oxalobacter formigenes was not associated with changes in urinary oxalate excretion. This was the first large study to show that OF alone was not capable of inducing changes in urinary oxalate excretion in a meaningful way.
• Caudarella R, Vescini F. Urinary citrate and renal stone disease: the preventive role of alkali citrate treatment. Arch Ital Urol Androl. 2009;81(3):182–7 This study focused on the lack of efficacy of probiotics containing oxalate-degrading bacteria, rather suggesting a robust network of bacteria that work together in regulating oxalate degradation.
Batagello CA, Monga M, Miller AW. Calcium oxalate urolithiasis: a case of missing microbes? J Endourol. 2018;32:995–1005. https://doi.org/10.1089/end.2018.0294.
Liu M, Koh H, Kurtz ZD, Battaglia T, PeBenito A, Li H, et al. Oxalobacter formigenes-associated host features and microbial community structures examined using the American Gut Project. Microbiome. 2017;5(1):108. https://doi.org/10.1186/s40168-017-0316-0.
Soucie JM, Thun MJ, Coates RJ, McClellan W, Austin H. Demographic and geographic variability of kidney stones in the United States. Kidney Int. 1994;46(3):893–9.
Gupta S, Allen-Vercoe E, Petrof EO. Fecal microbiota transplantation: in perspective. Ther Adv Gastroenterol. 2016;9(2):229–39. https://doi.org/10.1177/1756283X15607414.
Marotz CA, Zarrinpar A. Treating obesity and metabolic syndrome with fecal microbiota transplantation. Yale J Biol Med. 2016;89(3):383–8.
Lopez J, Grinspan A. Fecal microbiota transplantation for inflammatory bowel disease. Gastroenterol Hepatol (N Y). 2016;12(6):374–9.
•• Stern J, Burk R, Schoenfeld D, Davies K, Asplin J, Suadicani S. Fecal transplant modifies urine chemistry risk factors for urinary stone disease. Phys Rep. 2019; This study demonstrated that the ability of fecal transplants of the whole gut microbiome could modulate urinary parameters related to stone formation in an animal model.
Miller AW, Oakeson KF, Dale C, Dearing MD. Microbial community transplant results in increased and long-term oxalate degradation. Microb Ecol. 2016;72(2):470–8. https://doi.org/10.1007/s00248-016-0800-2.
Lieske JC. Probiotics for prevention of urinary stones. Ann Transl Med. 2017;5(2):29. https://doi.org/10.21037/atm.2016.11.86.
Dethlefsen L, Relman DA. Incomplete recovery and individualized responses of the human distal gut microbiota to repeated antibiotic perturbation. Proc Natl Acad Sci U S A. 2011;108(Suppl 1):4554–61. https://doi.org/10.1073/pnas.1000087107.
Kharlamb V, Schelker J, Francois F, Jiang J, Holmes RP, Goldfarb DS. Oral antibiotic treatment of Helicobacter pylori leads to persistently reduced intestinal colonization rates with Oxalobacter formigenes. J Endourol. 2011;25(11):1781–5. https://doi.org/10.1089/end.2011.0243.
Tasian GE, Jemielita T, Goldfarb DS, Copelovitch L, Gerber JS, Wu Q, et al. Oral antibiotic exposure and kidney stone disease. J Am Soc Nephrol. 2018;29(6):1731–40. https://doi.org/10.1681/ASN.2017111213.
Dethlefsen L, Huse S, Sogin ML, Relman DA. The pervasive effects of an antibiotic on the human gut microbiota, as revealed by deep 16S rRNA sequencing. PLoS Biol. 2008;6(11):e280. https://doi.org/10.1371/journal.pbio.0060280.
Arora HC, Eng C, Shoskes DA. Gut microbiome and chronic prostatitis/chronic pelvic pain syndrome. Ann Transl Med. 2017;5(2):30. https://doi.org/10.21037/atm.2016.12.32.
Marinkovic SP, Moldwin R, Gillen LM, Stanton SL. The management of interstitial cystitis or painful bladder syndrome in women. BMJ. 2009;339:b2707. https://doi.org/10.1136/bmj.b2707.
Warren JW, Brown V, Jacobs S, Horne L, Langenberg P, Greenberg P. Urinary tract infection and inflammation at onset of interstitial cystitis/painful bladder syndrome. Urology. 2008;71(6):1085–90. https://doi.org/10.1016/j.urology.2007.12.091.
Burkhard FC, Blick N, Hochreiter WW, Studer UE. Urinary urgency and frequency, and chronic urethral and/or pelvic pain in females. Can doxycycline help? J Urol. 2004;172(1):232–5. https://doi.org/10.1097/01.ju.0000128698.93305.2e.
Siddiqui H, Lagesen K, Nederbragt AJ, Jeansson SL, Jakobsen KS. Alterations of microbiota in urine from women with interstitial cystitis. BMC Microbiol. 2012;12:205. https://doi.org/10.1186/1471-2180-12-205.
Shoskes DA, Wang H, Polackwich AS, Tucky B, Altemus J, Eng C. Analysis of gut microbiome reveals significant differences between men with chronic prostatitis/chronic pelvic pain syndrome and controls. J Urol. 2016;196(2):435–41. https://doi.org/10.1016/j.juro.2016.02.2959.
Fouts DE, Pieper R, Szpakowski S, Pohl H, Knoblach S, Suh MJ, et al. Integrated next-generation sequencing of 16S rDNA and metaproteomics differentiate the healthy urine microbiome from asymptomatic bacteriuria in neuropathic bladder associated with spinal cord injury. J Transl Med. 2012;10:174. https://doi.org/10.1186/1479-5876-10-174.
Pearce MM, Hilt EE, Rosenfeld AB, Zilliox MJ, Thomas-White K, Fok C, et al. The female urinary microbiome: a comparison of women with and without urgency urinary incontinence. MBio. 2014;5(4):e01283–14. https://doi.org/10.1128/mBio.01283-14.
Nelson DE, Van Der Pol B, Dong Q, Revanna KV, Fan B, Easwaran S, et al. Characteristic male urine microbiomes associate with asymptomatic sexually transmitted infection. PLoS One. 2010;5(11):e14116. https://doi.org/10.1371/journal.pone.0014116.
Barr-Beare E, Saxena V, Hilt EE, Thomas-White K, Schober M, Li B, et al. The interaction between Enterobacteriaceae and calcium oxalate deposits. PLoS One. 2015;10(10):e0139575. https://doi.org/10.1371/journal.pone.0139575.
Schwaderer AL, Wolfe AJ. The association between bacteria and urinary stones. Ann Transl Med. 2017;5(2):32. https://doi.org/10.21037/atm.2016.11.73.
De Ferrari ME, Macaluso M, Brunati C, Pozzoli R, Colussi G. Hypocitraturia and Ureaplasma urealyticum urinary tract infection in patients with idiopathic calcium nephrolithiasis. Nephrol Dial Transplant. 1996;11(6):1185.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Justin A. Lee and Joshua M. Stern each declare no potential conflicts of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Endourology
Rights and permissions
About this article
Cite this article
Lee, J.A., Stern, J.M. Understanding the Link Between Gut Microbiome and Urinary Stone Disease. Curr Urol Rep 20, 19 (2019). https://doi.org/10.1007/s11934-019-0882-8
Published:
DOI: https://doi.org/10.1007/s11934-019-0882-8