Abstract
Purpose of Review
To highlight recent basic, translational, and clinical works demonstrating exercise and diet regulation of marrow adipose tissue (MAT) and bone and how this informs current understanding of the relationship between marrow adiposity and musculoskeletal health.
Recent Findings
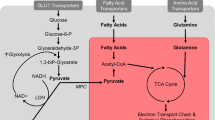
Marrow adipocytes accumulate in the bone in the setting of not only hypercaloric intake (calorie excess; e.g., diet-induced obesity) but also with hypocaloric intake (calorie restriction; e.g., anorexia), despite the fact that these states affect bone differently. With hypercaloric intake, bone quantity is largely unaffected, whereas with hypocaloric intake, bone quantity and quality are greatly diminished. Voluntary running exercise in rodents was found to lower MAT and promote bone in eucaloric and hypercaloric states, while degrading bone in hypocaloric states, suggesting differential modulation of MAT and bone, dependent upon whole-body energy status. Energy status alters bone metabolism and bioenergetics via substrate availability or excess, which plays a key role in the response of bone and MAT to mechanical stimuli.
Summary
Marrow adipose tissue (MAT) is a fat depot with a potential role in—as well as responsivity to—whole-body energy metabolism. Understanding the localized function of this depot in bone cell bioenergetics and substrate storage, principally in the exercised state, will aid to uncover putative therapeutic targets for skeletal fragility.


Similar content being viewed by others
Data Availability
Not applicable.
References
Papers of particular interest, published recently, have been highlighted as: •• Of major importance
Pagnotti GM, Styner M. Exercise regulation of marrow adipose tissue. Front Endocrinol (Lausanne). 2016;7:94. https://doi.org/10.3389/fendo.2016.00094.
Pagnotti GM, Styner M, Uzer G, Patel VS, Wright LE, Ness KK, et al. Combating osteoporosis and obesity with exercise: leveraging cell mechanosensitivity. Nat Rev Endocrinol. 2019;15(6):339–55. https://doi.org/10.1038/s41574-019-0170-1.
Paccou J, Hardouin P, Cotten A, Penel G, Cortet B. The role of bone marrow fat in skeletal health: usefulness and perspectives for clinicians. J Clin Endocrinol Metab. 2015;100(10):3613–21. https://doi.org/10.1210/jc.2015-2338.
Devlin MJ. Why does starvation make bones fat? Am J Hum Biol. 2011;23(5):577–85. https://doi.org/10.1002/ajhb.21202.
Naveiras O, Nardi V, Wenzel PL, Hauschka PV, Fahey F, Daley GQ. Bone-marrow adipocytes as negative regulators of the haematopoietic microenvironment. Nature. 2009;460(7252):259–63. https://doi.org/10.1038/nature08099.
Zhou BO, Yu H, Yue R, Zhao Z, Rios JJ, Naveiras O, et al. Bone marrow adipocytes promote the regeneration of stem cells and haematopoiesis by secreting SCF. Nat Cell Biol. 2017;19(8):891–903. https://doi.org/10.1038/ncb3570.
•• Zhang Z, Huang Z, Ong B, Sahu C, Zeng H, Ruan HB. Bone marrow adipose tissue-derived stem cell factor mediates metabolic regulation of hematopoiesis. Haematologica. 2019;104(9):1731–43. https://doi.org/10.3324/haematol.2018.205856Stem cell factor, a MAT-secreted hormone, acts as an integral mediator for metabolic regulation of hematopoietic stem cells and its absence significantly impairs hematopoiesis.
Oehlbeck LW, Robscheit-Robbins FS, Whipple GH. Marrow hyperplasia and hemoglobin reserve in experimental anemia due to bleeding. J Exp Med. 1932;56(3):425–48. https://doi.org/10.1084/jem.56.3.425.
Meunier P, Aaron J, Edouard C, Vignon G. Osteoporosis and the replacement of cell populations of the marrow by adipose tissue. A quantitative study of 84 iliac bone biopsies. Clin Orthop Relat Res. 1971;80:147–54. https://doi.org/10.1097/00003086-197110000-00021.
Lanotte M, Scott D, Dexter TM, Allen TD. Clonal preadipocyte cell lines with different phenotypes derived from murine marrow stroma: factors influencing growth and adipogenesis in vitro. J Cell Physiol. 1982;111(2):177–86. https://doi.org/10.1002/jcp.1041110209.
Kodama HA, Amagai Y, Koyama H, Kasai S. A new preadipose cell line derived from newborn mouse calvaria can promote the proliferation of pluripotent hemopoietic stem cells in vitro. J Cell Physiol. 1982;112(1):89–95. https://doi.org/10.1002/jcp.1041120114.
Rozman C, Feliu E, Berga L, Reverter JC, Climent C, Ferran MJ. Age-related variations of fat tissue fraction in normal human bone marrow depend both on size and number of adipocytes: a stereological study. Exp Hematol. 1989;17(1):34–7.
Rozman C, Reverter JC, Feliu E, Berga L, Rozman M, Climent C. Variations of fat tissue fraction in abnormal human bone marrow depend both on size and number of adipocytes: a stereologic study. Blood. 1990;76(5):892–5.
Hood RL, Allen CE. Cellularity of bovine adipose tissue. J Lipid Res. 1973;14(6):605–10.
Scheller EL, Troiano N, Vanhoutan JN, Bouxsein MA, Fretz JA, Xi Y, et al. Use of osmium tetroxide staining with microcomputerized tomography to visualize and quantify bone marrow adipose tissue in vivo. Methods Enzymol. 2014;537:123–39. https://doi.org/10.1016/B978-0-12-411619-1.00007-0.
Styner M, Thompson WR, Galior K, Uzer G, Wu X, Kadari S, et al. Bone marrow fat accumulation accelerated by high fat diet is suppressed by exercise. Bone. 2014;64:39–46. https://doi.org/10.1016/j.bone.2014.03.044.
Uzer G, Thompson WR, Sen B, Xie Z, Yen SS, Miller S, et al. Cell Mechanosensitivity to extremely low-magnitude signals is enabled by a LINCed nucleus. Stem Cells. 2015;33(6):2063–76. https://doi.org/10.1002/stem.2004.
•• McGrath C, Sankaran JS, Misaghian-Xanthos N, Sen B, Xie Z, Styner MA, et al. Exercise degrades bone in caloric restriction, despite suppression of marrow adipose tissue (MAT). J Bone Miner Res. 2020;35(1):106–15. https://doi.org/10.1002/jbmr.3872Moderate calorie restriction induced MAT accumulation and trabecular bone loss, while combined restriction and exercise modestly suppressed MAT and further degraded bone.
Styner M, Pagnotti GM, McGrath C, Wu X, Sen B, Uzer G, et al. Exercise decreases marrow adipose tissue through β-oxidation in obese running mice. J Bone Miner Res Off J Am Soc Bone Miner Res. 2017. https://doi.org/10.1002/jbmr.3159.
Wang MC, Bachrach LK, Van Loan M, Hudes M, Flegal KM, Crawford PB. The relative contributions of lean tissue mass and fat mass to bone density in young women. Bone. 2005;37(4):474–81. https://doi.org/10.1016/j.bone.2005.04.038.
De Laet C, Kanis JA, Odén A, Johanson H, Johnell O, Delmas P, et al. Body mass index as a predictor of fracture risk: a meta-analysis. Osteoporos Int. 2005;16(11):1330–8. https://doi.org/10.1007/s00198-005-1863-y.
Sankaran JS, Sen B, Dudakovic A, Paradise CR, Perdue T, Xie Z, et al. Knockdown of formin mDia2 alters lamin B1 levels and increases osteogenesis in stem cells. Stem Cells. 2020;38(1):102–17. https://doi.org/10.1002/stem.3098.
Robles H, Park S, Joens MS, Fitzpatrick JAJ, Craft CS, Scheller EL. Characterization of the bone marrow adipocyte niche with three-dimensional electron microscopy. Bone. 2019;118:89–98. https://doi.org/10.1016/j.bone.2018.01.020.
Scheller EL, Doucette CR, Learman BS, Cawthorn WP, Khandaker S, Schell B, et al. Region-specific variation in the properties of skeletal adipocytes reveals regulated and constitutive marrow adipose tissues. Nat Commun. 2015;6:7808. https://doi.org/10.1038/ncomms8808.
Cuminetti V, Arranz L. Bone marrow adipocytes: the enigmatic components of the hematopoietic stem cell niche. J Clin Med. 2019;8(5). doi:https://doi.org/10.3390/jcm8050707.
Yu EW, Greenblatt L, Eajazi A, Torriani M, Bredella MA. Marrow adipose tissue composition in adults with morbid obesity. Bone. 2017;97:38–42. https://doi.org/10.1016/j.bone.2016.12.018.
Turner RT, Martin SA, Iwaniec UT. Metabolic coupling between bone marrow adipose tissue and hematopoiesis. Curr Osteoporos Rep. 2018;16(2):95–104. https://doi.org/10.1007/s11914-018-0422-3.
Liu LF, Shen WJ, Ueno M, Patel S, Kraemer FB. Characterization of age-related gene expression profiling in bone marrow and epididymal adipocytes. BMC Genomics. 2011;12:212. https://doi.org/10.1186/1471-2164-12-212.
Suchacki KJ, Tavares AAS, Mattiucci D, Scheller EL, Papanastasiou G, Gray C, et al. Bone marrow adipose tissue is a unique adipose subtype with distinct roles in glucose homeostasis. Nat Commun. 2020;11(1):3097. https://doi.org/10.1038/s41467-020-16878-2.
Yeung DK, Griffith JF, Antonio GE, Lee FK, Woo J, Leung PC. Osteoporosis is associated with increased marrow fat content and decreased marrow fat unsaturation: a proton MR spectroscopy study. J Magn Reson Imaging. 2005;22(2):279–85.
Li R, Liang L, Dou Y, Huang Z, Mo H, Wang Y, et al. Mechanical stretch inhibits mesenchymal stem cell adipogenic differentiation through TGFbeta1/Smad2 signaling. J Biomech. 2015;48(13):3665–71. https://doi.org/10.1016/j.jbiomech.2015.08.013.
Krings A, Rahman S, Huang S, Lu Y, Czernik PJ, Lecka-Czernik B. Bone marrow fat has brown adipose tissue characteristics, which are attenuated with aging and diabetes. Bone. 2012;50(2):546–52. https://doi.org/10.1016/j.bone.2011.06.016.
Tavassoli M, Houchin DN, Jacobs P. Fatty acid composition of adipose cells in red and yellow marrow: a possible determinant of haematopoietic potential. Scand J Haematol. 1977;18(1):47–53. https://doi.org/10.1111/j.1600-0609.1977.tb01476.x.
Bohnert M. New friends for seipin - implications of seipin partner proteins in the life cycle of lipid droplets. Semin Cell Dev Biol. 2020. https://doi.org/10.1016/j.semcdb.2020.04.012.
Tarnopolsky MA, Rennie CD, Robertshaw HA, Fedak-Tarnopolsky SN, Devries MC, Hamadeh MJ. Influence of endurance exercise training and sex on intramyocellular lipid and mitochondrial ultrastructure, substrate use, and mitochondrial enzyme activity. Am J Physiol Regul Integr Comp Physiol. 2007;292(3):R1271–8. https://doi.org/10.1152/ajpregu.00472.2006.
Kozubik A, Sedlakova A, Pospisil M, Petrasek R. In vivo studies of the relationship between the activation of lipid metabolism, postirradiation bone marrow cell proliferation and radioresistance of mice. Gen Physiol Biophys. 1988;7(3):293–302.
Valentinitsch A, Patsch JM, Burghardt AJ, Link TM, Majumdar S, Fischer L, et al. Computational identification and quantification of trabecular microarchitecture classes by 3-D texture analysis-based clustering. Bone. 2013;54(1):133–40. https://doi.org/10.1016/j.bone.2012.12.047.
Griffith JF, Yeung DKW, Antonio GE, Wong SYS, Kwok TCY, Woo J, et al. Vertebral marrow fat content and diffusion and perfusion indexes in women with varying bone density: MR evaluation. Radiology. 2006;241(3):831–8. https://doi.org/10.1148/radiol.2413051858.
Patsch JM, Li X, Baum T, Yap SP, Karampinos DC, Schwartz AV, et al. Bone marrow fat composition as a novel imaging biomarker in postmenopausal women with prevalent fragility fractures. J Bone Miner Res. 2013. https://doi.org/10.1002/jbmr.1950.
Stout MB, Swindell WR, Zhi X, Rohde K, List EO, Berryman DE, et al. Transcriptome profiling reveals divergent expression shifts in brown and white adipose tissue from long-lived GHRKO mice. Oncotarget. 2015;6(29):26702–15. https://doi.org/10.18632/oncotarget.5760.
Palmer AK, Kirkland JL. Aging and adipose tissue: potential interventions for diabetes and regenerative medicine. Exp Gerontol. 2016;86:97–105. https://doi.org/10.1016/j.exger.2016.02.013.
Picard F, Guarente L. Molecular links between aging and adipose tissue. Int J Obes. 2005;29(Suppl 1):S36–9. https://doi.org/10.1038/sj.ijo.0802912.
Lecka-Czernik B, Stechschulte LA, Czernik PJ, Dowling AR. High bone mass in adult mice with diet-induced obesity results from a combination of initial increase in bone mass followed by attenuation in bone formation; implications for high bone mass and decreased bone quality in obesity. Mol Cell Endocrinol. 2015. https://doi.org/10.1016/j.mce.2015.01.001.
Rahman S, Lu Y, Czernik PJ, Rosen CJ, Enerback S, Lecka-Czernik B. Inducible brown adipose tissue, or beige fat is anabolic for the skeleton. Endocrinology. 2013. https://doi.org/10.1210/en.2012-2162.
Bonnet N, Bourgoin L, Biver E, Douni E, Ferrari S. RANKL inhibition improves muscle strength and insulin sensitivity and restores bone mass. J Clin Invest. 2019;129(8):3214–23. https://doi.org/10.1172/JCI125915.
Hanley DA, Adachi JD, Bell A, Brown V. Denosumab: mechanism of action and clinical outcomes. Int J Clin Pract. 2012;66(12):1139–46. https://doi.org/10.1111/ijcp.12022.
Zebaze RM, Libanati C, Austin M, Ghasem-Zadeh A, Hanley DA, Zanchetta JR, et al. Differing effects of denosumab and alendronate on cortical and trabecular bone. Bone. 2014;59:173–9. https://doi.org/10.1016/j.bone.2013.11.016.
Harris KB, Nealy KL, Jackson DJ, Thornton PL. The clinical use of denosumab for the management of low bone mineral density in postmenopausal women. J Pharm Pract. 2012;25(3):310–8. https://doi.org/10.1177/0897190012442061.
Thomas DM, Maher F, Rogers SD, Best JD. Expression and regulation by insulin of Glut 3 in UMR 106-01, a clonal rat osteosarcoma cell line. Biochem Biophys Res Commun. 1996;218(3):789–93. https://doi.org/10.1006/bbrc.1996.0140.
Wei J, Shimazu J, Makinistoglu MP, Maurizi A, Kajimura D, Zong H, et al. Glucose uptake and Runx2 synergize to orchestrate osteoblast differentiation and bone formation. Cell. 2015;161(7):1576–91. https://doi.org/10.1016/j.cell.2015.05.029.
Zoch ML, Abou DS, Clemens TL, Thorek DL, Riddle RC. In vivo radiometric analysis of glucose uptake and distribution in mouse bone. Bone Res. 2016;4(December 2015):16004. https://doi.org/10.1038/boneres.2016.4.
Esen E, Chen J, Karner CM, Okunade AL, Patterson BW, Long F. WNT-LRP5 signaling induces Warburg effect through mTORC2 activation during osteoblast differentiation. Cell Metab. 2013;17(5):745–55. https://doi.org/10.1016/j.cmet.2013.03.017.
Karner CM, Esen E, Okunade AL, Patterson BW, Long F. Increased glutamine catabolism mediates bone anabolism in response to WNT signaling. J Clin Invest. 2015;125(2):551–62. https://doi.org/10.1172/JCI78470.
Frey JL, Li Z, Ellis JM, Zhang Q, Farber CR, Aja S, et al. Wnt-Lrp5 signaling regulates fatty acid metabolism in the osteoblast. Mol Cell Biol. 2015;35(11):1979–91. https://doi.org/10.1128/MCB.01343-14.
Pritchard JJ. A cytological and histochemical study of bone and cartilage formation in the rat. J Anat. 1959;86:259–77.
Thompson WR, Uzer G, Brobst KE, Xie Z, Sen B, Yen SS, et al. Osteocyte specific responses to soluble and mechanical stimuli in a stem cell derived culture model. Sci Rep. 2015;5:11049. https://doi.org/10.1038/srep11049.
Lecka-Czernik B. Marrow fat metabolism is linked to the systemic energy metabolism. Bone. 2012;50(2):534–9. https://doi.org/10.1016/j.bone.2011.06.032.
Simsek T, Kocabas F, Zheng J, Deberardinis RJ, Mahmoud AI, Olson EN, et al. The distinct metabolic profile of hematopoietic stem cells reflects their location in a hypoxic niche. Cell Stem Cell. 2010;7(3):380–90. https://doi.org/10.1016/j.stem.2010.07.011.
Oburoglu L, Tardito S, Fritz V, de Barros SC, Merida P, Craveiro M, et al. Glucose and glutamine metabolism regulate human hematopoietic stem cell lineage specification. Cell Stem Cell. 2014;15:169–84. https://doi.org/10.1016/j.stem.2014.06.002.
Oburoglu L, Romano M, Taylor N, Kinet S. Metabolic regulation of hematopoietic stem cell commitment and erythroid differentiation. Curr Opin Hematol. 2016;23(3):198–205. https://doi.org/10.1097/MOH.0000000000000234.
Morten KJ, Badder L, Knowles HJ. Differential regulation of HIF-mediated pathways increases mitochondrial metabolism and ATP production in hypoxic osteoclasts. J Pathol. 2013;229:755–64. https://doi.org/10.1002/path.4159.
Karner CM, Long F. Glucose metabolism in bone. Bone. 2018;115:2–7. https://doi.org/10.1016/j.bone.2017.08.008.
Weivoda MM, Chew CK, Monroe DG, Farr JN, Atkinson EJ, Geske JR, et al. Identification of osteoclast-osteoblast coupling factors in humans reveals links between bone and energy metabolism. Nat Commun. 2020;11(1):87. https://doi.org/10.1038/s41467-019-14003-6.
Schmidt-Rohr K. Oxygen is the high-energy molecule powering complex multicellular life: fundamental corrections to traditional bioenergetics. ACS Omega. 2020;5(5):2221–33. https://doi.org/10.1021/acsomega.9b03352.
Brand K. Aerobic glycolysis by proliferating cells: protection against oxidative stress at the expense of energy yield. J Bioenerg Biomembr. 1997;29(4):355–64. https://doi.org/10.1023/a:1022498714522.
Shum LC, White NS, Mills BN, Bentley KL, Eliseev RA. Energy metabolism in mesenchymal stem cells during osteogenic differentiation. Stem Cells Dev. 2016;25(2):114–22. https://doi.org/10.1089/scd.2015.0193.
Mylotte LA, Duffy AM, Murphy M, O’Brien T, Samali A, Barry F, et al. Metabolic flexibility permits mesenchymal stem cell survival in an ischemic environment. Stem Cells. 2008;26(5):1325–36. https://doi.org/10.1634/stemcells.2007-1072.
Du W, Zhang L, Brett-Morris A, Aguila B, Kerner J, Hoppel CL, et al. HIF drives lipid deposition and cancer in ccRCC via repression of fatty acid metabolism. Nat Commun. 2017;8(1):1769. https://doi.org/10.1038/s41467-017-01965-8.
Papandreou I, Cairns RA, Fontana L, Lim AL, Denko NC. HIF-1 mediates adaptation to hypoxia by actively downregulating mitochondrial oxygen consumption. Cell Metab. 2006;3(3):187–97. https://doi.org/10.1016/j.cmet.2006.01.012.
Kushwaha P, Wolfgang MJ, Riddle RC. Fatty acid metabolism by the osteoblast. Bone. 2018;115(November):8–14. https://doi.org/10.1016/j.bone.2017.08.024.
Komarova SV, Ataullakhanov FI, Globus RK. Bioenergetics and mitochondrial transmembrane potential during differentiation of cultured osteoblasts. Am J Physiol Cell Physiol. 2000;279(4):C1220–9. https://doi.org/10.1152/ajpcell.2000.279.4.C1220.
Kim SP, Li Z, Zoch ML, Frey JL, Bowman CE, Kushwaha P, et al. Fatty acid oxidation by the osteoblast is required for normal bone acquisition in a sex- and diet-dependent manner. JCI Insight. 2017;2(16):1–16. https://doi.org/10.1172/jci.insight.92704.
Shockley KR, Lazarenko OP, Czernik PJ, Rosen CJ, Churchill GA, Lecka-Czernik B. PPARgamma2 nuclear receptor controls multiple regulatory pathways of osteoblast differentiation from marrow mesenchymal stem cells. J Cell Biochem. 2009;106(2):232–46. https://doi.org/10.1002/jcb.21994.
Li Z, Macdougald OA. Stem cell factor: the bridge between bone marrow adipocytes and hematopoietic cells. Haematologica. 2019;104(9):1689–91. https://doi.org/10.3324/haematol.2019.224188.
Rimmelé P, Liang R, Bigarella CL, Kocabas F, Xie J, Serasinghe MN, et al. Mitochondrial metabolism in hematopoietic stem cells requires functional FOXO 3. EMBO Rep. 2015;16(9):1164–76. https://doi.org/10.15252/embr.201439704.
Kim JM, Jeong D, Kang HK, Jung SY, Kang SS, Min BM. Osteoclast precursors display dynamic metabolic shifts toward accelerated glucose metabolism at an early stage of RANKL-stimulated osteoclast differentiation. Cell Physiol Biochem. 2007;20:935–46. https://doi.org/10.1159/000110454.
Lemma S, Sboarina M, Porporato PE, Zini N, Sonveaux P, Di Pompo G, et al. Energy metabolism in osteoclast formation and activity. Int J Biochem Cell Biol. 2016;79(August):168–80. https://doi.org/10.1016/j.biocel.2016.08.034.
Indo Y, Takeshita S, Ishii KA, Hoshii T, Aburatani H, Hirao A, et al. Metabolic regulation of osteoclast differentiation and function. J Bone Miner Res. 2013;28(11):2392–9. https://doi.org/10.1002/jbmr.1976.
Bredella MA, Torriani M, Ghomi RH, Thomas BJ, Brick DJ, Gerweck AV, et al. Vertebral bone marrow fat is positively associated with visceral fat and inversely associated with IGF-1 in obese women. Obesity (Silver Spring). 2011;19(1):49–53. https://doi.org/10.1038/oby.2010.106.
McCabe LR, Irwin R, Tekalur A, Evans C, Schepper JD. Exercise prevents high fat diet-induced bone loss , marrow adiposity and dysbiosis in male mice. Bone. 2019;118:20–31. https://doi.org/10.1016/j.bone.2018.03.024.
Devlin MJ, Cloutier AM, Thomas NA, Panus DA, Lotinun S, Pinz I, et al. Caloric restriction leads to high marrow adiposity and low bone mass in growing mice. J Bone Miner Res. 2010;25(9):2078–88. https://doi.org/10.1002/jbmr.82.
Bredella MA. Perspective: the bone-fat connection. Skelet Radiol. 2010;39(8):729–31. https://doi.org/10.1007/s00256-010-0936-y.
Amrein K, Amrein S, Drexler C, Dimai HP, Dobnig H, Pfeifer K, et al. Sclerostin and its association with physical activity, age, gender, body composition, and bone mineral content in healthy adults. J Clin Endocrinol Metab. 2012;97(1):148–54. https://doi.org/10.1210/jc.2011-2152.
Lavet C, Martin A, Linossier MT, Bossche AV, Laroche N, Thomas M, et al. Fat and sucrose intake induces obesity-related bone metabolism disturbances: kinetic and reversibility studies in growing and adult rats. J Bone Miner Res. 2016;31(1):98–115. https://doi.org/10.1002/jbmr.2596.
Heinonen S, Saarinen L, Naukkarinen J, Rodriguez A, Fruhbeck G, Hakkarainen A, et al. Adipocyte morphology and implications for metabolic derangements in acquired obesity. Int J Obes. 2014;38(11):1423–31. https://doi.org/10.1038/ijo.2014.31.
Spalding KL, Arner E, Westermark PO, Bernard S, Buchholz BA, Bergmann O, et al. Dynamics of fat cell turnover in humans. Nature. 2008;453(7196):783–7. https://doi.org/10.1038/nature06902.
Nishino N, Tamori Y, Tateya S, Kawaguchi T, Shibakusa T, Mizunoya W, et al. FSP27 contributes to efficient energy storage in murine white adipocytes by promoting the formation of unilocular lipid droplets. J Clin Investig. 2008;118(8):2808–21. https://doi.org/10.1172/JCI34090.
Fazeli PK, Bredella MA, Freedman L, Thomas BJ, Breggia A, Meenaghan E, et al. Marrow fat and preadipocyte factor-1 levels decrease with recovery in women with anorexia nervosa. J Bone Miner Res. 2012;27(9):1864–71. https://doi.org/10.1002/jbmr.1640.
Pontzer H. Constrained total energy expenditure and the evolutionary biology of energy balance. Exerc Sport Sci Rev. 2015;43(3):110–6. https://doi.org/10.1249/JES.0000000000000048.
Pontzer H. Energy constraint as a novel mechanism linking exercise and health. Physiology. 2018;33(6):384–93. https://doi.org/10.1152/physiol.00027.2018.
Cordes C, Dieckmeyer M, Ott B, Shen J, Ruschke S, Settles M, et al. MR-detected changes in liver fat, abdominal fat, and vertebral bone marrow fat after a four-week calorie restriction in obese women. J Magn Reson Imaging. 2015;42(5):1272–80. https://doi.org/10.1002/jmri.24908.
Bredella MA, Fazeli PK, Miller KK, Misra M, Torriani M, Thomas BJ, et al. Increased bone marrow fat in anorexia nervosa. J Clin Endocrinol Metab. 2009;94(6):2129–36. https://doi.org/10.1210/jc.2008-2532.
Cao JJ. Caloric restriction combined with exercise is effective in reducing adiposity and mitigating bone structural deterioration in obese rats. Ann N Y Acad Sci. 2018;1433(1):41–52. https://doi.org/10.1111/nyas.13936.
Styner M, Pagnotti GM, Galior K, Wu X, Thompson WR, Uzer G, et al. Exercise regulation of marrow fat in the setting of PPARgamma agonist treatment in female C57BL/6 mice. Endocrinology. 2015;156(8):2753–61. https://doi.org/10.1210/en.2015-1213.
Ko FC, Martins JS, Reddy P, Bragdon B, Hussein AI, Gerstenfeld LC, et al. Acute phosphate restriction impairs bone formation and increases marrow adipose tissue in growing mice. J Bone Miner Res. 2016;31(12):2204–14. https://doi.org/10.1002/jbmr.2891.
Lips P, Van Schoor NM. The effect of vitamin D on bone and osteoporosis. Best Pract Res Clin Endocrinol Metab. 2011;25(4):585–91. https://doi.org/10.1016/j.beem.2011.05.002.
Zofkova I, Davis M, Blahos J. Trace elements have beneficial, as well as detrimental effects on bone homeostasis. Physiol Res. 2017;66(3):391–402. https://doi.org/10.33549/physiolres.933454.
Price CT, Langford JR, Liporace FA. Essential nutrients for bone health and a review of their availability in the average North American diet. Open Orthop J. 2012;6(1):143–9. https://doi.org/10.2174/1874325001206010143.
Ozcivici E, Luu YK, Adler B, Qin YX, Rubin J, Judex S, et al. Mechanical signals as anabolic agents in bone. Nat Rev Rheumatol. 2010;6(1):50–9. https://doi.org/10.1038/nrrheum.2009.239.Mechanical.
Rubin C, Lanyon L. Regulation of bone formation by applied dynamic loads. J Bone Joint Surg. 1984;66A:397–402.
Rubin C, Turner AS, Bain S, Mallinckrodt C, McLeod K. Low mechanical signals strengthen long bones. Nature. 2001;412(6847):603–4. https://doi.org/10.1038/35088119.
Rubin J. Regulation of skeletal remodeling by biomechanical input. Osteoporos Int. 2003;14(Suppl 5):S43–S5. https://doi.org/10.1007/s00198-003-1472-6.
Thompson WR, Rubin CT, Rubin J. Mechanical regulation of signaling pathways in bone. Gene. 2012;503(2):179–93. https://doi.org/10.1038/jid.2014.371.
Phu S, Bani Hassan E, Vogrin S, Kirk B, Duque G. Effect of denosumab on falls, muscle strength, and function in community-dwelling older adults. J Am Geriatr Soc. 2019;67(12):2660–1. https://doi.org/10.1111/jgs.16165.
Gross TS, Rubin CT. Uniformity of resorptive bone loss induced by disuse. J Orthop Res. 1995;13(5):708–14. https://doi.org/10.1002/jor.1100130510.
Judex S, Garman R, Squire M, Busa B, Donahue LR, Rubin C. Genetically linked site-specificity of disuse osteoporosis. J Bone Miner Res. 2004;19(4):607–13. https://doi.org/10.1359/JBMR.040110.
Jee S, Wronski E, Morey J, Kimmel D. Effects of spaceflight on trabecular bone in rats. Am J Phys. 1983;244:4310–4.
Hino K, Nifuji A, Morinobu M, Tsuji K, Ezura Y, Nakashima K, et al. Unloading-induced bone loss was suppressed in gold-thioglucose treated mice. J Cell Biochem. 2006;99(3):845–52. https://doi.org/10.1002/jcb.20935.
Keune JA, Wong CP, Br AJ, Iwaniec UT, Turner RT. Bone marrow adipose tissue deficiency increases disuse-induced bone loss in male mice. Sci Rep. 2017;7(46325). doi:https://doi.org/10.1038/srep46325.
Tatsumi S, Ishii K, Amizuka N, Li M, Kobayashi T, Kohno K, et al. Targeted ablation of osteocytes induces osteoporosis with defective mechanotransduction. Cell Metab. 2007;5(6):464–75. https://doi.org/10.1016/j.cmet.2007.05.001.
Aguirre JI, Plotkin LI, Stewart SA, Weinstein RS, Parfitt AM, Manolagas SC, et al. Osteocyte apoptosis is induced by weightlessness in mice and precedes osteoclast recruitment and bone loss. J Bone Miner Res. 2006;21(4):605–15. https://doi.org/10.1359/jbmr.060107.
Iwaniec UT, Philbrick KA, Wong CP, Gordon JL, Kahler-Quesada AM, Olson DA, et al. Room temperature housing results in premature cancellous bone loss in growing female mice: implications for the mouse as a preclinical model for age-related bone loss. Osteoporos Int. 2016;27(10):3091–101. https://doi.org/10.1007/s00198-016-3634-3.
LeBlanc A, Schneider V, Shackelford L, West S, Oganov V, Bakulin A, et al. Bone mineral and lean tissue loss after long duration space flight. J Musculoskelet Neuronal Interact. 2000;1(2):157–60.
Lang T, Leblanc A, Evans H, Lu Y, Genant H, Yu A. Cortical and trabecular bone mineral loss from the spine and hip in long-duration spaceflight. J Bone Miner Res. 2004;19(6). doi:https://doi.org/10.1359/JBMR.040307.
Trudel G, Payne M, Madler B, Ramachandran N, Lecompte M, Wade C, et al. Bone marrow fat accumulation after 60 days of bed rest persisted 1 year after activities were resumed along with hemopoietic stimulation: the Women International Space Simulation for Exploration study. J Appl Physiol. 2009;107(2):540–8. https://doi.org/10.1152/japplphysiol.91530.2008.
Trudel G, Coletta E, Cameron I, Belavy DL, Lecompte M, Armbrecht G, et al. Resistive exercises, with or without whole body vibration, prevent vertebral marrow fat accumulation during 60 days of head-down tilt bed rest in men. J Appl Physiol. 2012;112(11):1824–31. https://doi.org/10.1152/japplphysiol.00029.2012.
Ambrosi TH, Scialdone A, Graja A, Saraiva LR, Schulz TJ. Adipocyte accumulation in the bone marrow during obesity and aging impairs stem cell-based hematopoietic and bone regeneration. Cell Stem Cell. 2017;20:771–84. https://doi.org/10.1016/j.stem.2017.02.009.
Hinton PS, Nigh P, Thyfault J. Effectiveness of resistance training or jumping-exercise to increase bone mineral density in men with low bone mass: a 12-month randomized, clinical trial. Bone. 2015;79:203–12. https://doi.org/10.1016/j.bone.2015.06.008.
Hinton PS, Shankar K, Eaton LM, Rector RS. Obesity-related changes in bone structural and material properties in hyperphagic OLETF rats and protection by voluntary wheel running. Metab Clin Exp. 2015;64(8):905–16. https://doi.org/10.1016/j.metabol.2015.04.004.
Newhall KM, Rodnick KJ, van der Meulen MC, Carter DR, Marcus R. Effects of voluntary exercise on bone mineral content in rats. J Bone Miner Res. 1991;6(3):289–96.
Hamann N, Kohler T, Müller R, Brüggemann GP, Niehoff A. The effect of level and downhill running on cortical and trabecular bone in growing rats. Calcif Tissue Int. 2012;90(5):429–37. https://doi.org/10.1007/s00223-012-9593-6.
Tamakoshi K, Nishii Y, Minematsu A. Upward running is more beneficial than level surface or downslope running in reverting tibia bone degeneration in ovariectomized rats. J Musculoskelet Neuronal Interact. 2018;18(4):493–500.
Gregor RJ, Smith DW, Prilutsky BI. Mechanics of slope walking in the cat: quantification of muscle load, length change, and ankle extensor EMG patterns. J Neurophysiol. 2006;95(3):1397–409. https://doi.org/10.1152/jn.01300.2004.
Wallace IJ, Pagnotti GM, Rubin-Sigler J, Naeher M, Copes LE, Judex S, et al. Focal enhancement of the skeleton to exercise correlates with responsivity of bone marrow mesenchymal stem cells rather than peak external forces. J Exp Biol. 2015;218(19):3002–9. https://doi.org/10.1242/jeb.118729.
Huang TH, Su IH, Lewis JL, Chang MS, Hsu AT, Perrone CE, et al. Effects of methionine restriction and endurance exercise on bones of ovariectomized rats: a study of histomorphometry, densitometry, and biomechanical properties. J Appl Physiol. 2015;119(5):517–26. https://doi.org/10.1152/japplphysiol.00395.2015.
Baker JM, De Lisio M, Parise G. Endurance exercise training promotes medullary hematopoiesis. FASEB J. 2011;25(12):4348–57. https://doi.org/10.1096/fj.11-189043.
Yuasa Y, Miyakoshi N, Kasukawa Y, Nagahata I, Akagawa M, Ono Y, et al. Effects of bazedoxifene and low-intensity aerobic exercise on bone and fat parameters in ovariectomized rats. J Bone Miner Metab. 2020;38(2):179–87. https://doi.org/10.1007/s00774-019-01045-5.
Bertheau RC, Lorbeer R, Nattenmuller J, Wintermeyer E, Machann J, Linkohr B, et al. Bone marrow fat fraction assessment in regard to physical activity: KORA FF4-3-T MR imaging in a population-based cohort. Eur Radiol. 2020;30(6):3417–28. https://doi.org/10.1007/s00330-019-06612-y.
Belavy DL, Quittner MJ, Ridgers ND, Shiekh A, Rantalainen T, Trudel G. Specific modulation of vertebral marrow adipose tissue by physical activity. J Bone Miner Res. 2018;33(4):651–7. https://doi.org/10.1002/jbmr.3357.
Mori T, Okimoto N, Sakai A, Okazaki Y, Nakura N, Notomi T, et al. Climbing exercise increases bone mass and trabecular bone turnover through transient regulation of marrow osteogenic and osteoclastogenic potentials in mice. J Bone Miner Res. 2003;18(11):2002–9. https://doi.org/10.1359/jbmr.2003.18.11.2002.
Gomes RM, Junior MDF, Francisco FA, Moreira VM, de Almeida DL, Saavedra LPJ, et al. Strength training reverses ovariectomy-induced bone loss and improve metabolic parameters in female Wistar rats. Life Sci. 2018;213(October):134–41. https://doi.org/10.1016/j.lfs.2018.10.032.
Singulani MP, Stringhetta-Garcia CT, Santos LF, Morais SR, Louzada MJ, Oliveira SH, et al. Effects of strength training on osteogenic differentiation and bone strength in aging female Wistar rats. Sci Rep. 2017;7(February):42878. https://doi.org/10.1038/srep42878.
Swift JM, Gasier HG, Swift SN, Wiggs MP, Hogan HA, Fluckey JD, et al. Increased training loads do not magnify cancellous bone gains with rodent jump resistance exercise. J Appl Physiol. 2010;109(6):1600–7. https://doi.org/10.1152/japplphysiol.00596.2010.
Marín-Cascales E, Alcaraz PE, Ramos-Campo DJ, Rubio-Arias JA. Effects of multicomponent training on lean and bone mass in postmenopausal and older women: a systematic review. Menopause. 2018;25(3):346–56. https://doi.org/10.1097/GME.0000000000000975.
Sañudo B, De Hoyo M, Del Pozo-Cruz J, Carrasco L, Del Pozo-Cruz B, Tejero S, et al. A systematic review of the exercise effect on bone health: the importance of assessing mechanical loading in perimenopausal and postmenopausal women. Menopause. 2017;24(10):1208–16. https://doi.org/10.1097/GME.0000000000000872.
Lambert C, Beck BR, Harding AT, Watson SL, Weeks BK. Regional changes in indices of bone strength of upper and lower limbs in response to high-intensity impact loading or high-intensity resistance training. Bone. 2020;132(July 2019):115192. https://doi.org/10.1016/j.bone.2019.115192.
•• Harding AT, Weeks BK, Lambert C, Watson SL, Weis LJ, Beck BR. A comparison of bone-targeted exercise strategies to reduce fracture risk in middle-aged and older men with osteopenia and osteoporosis: LIFTMOR-M Semi-Randomized Controlled Trial. J Bone Miner Res. 2020;35(8):1404–14. https://doi.org/10.1002/jbmr.4008Older men with low bone mass participating in an 8-month high-intensity resistance and impact training program significantly improved lumbar spine and femoral neck BMD, as well as cortical thickness at the femoral neck, proving the safety and efficacy of strength training for osteoporosis prevention.
Watson SL, Weeks BK, Weis LJ, Harding AT, Horan SA, Beck BR. High-intensity resistance and impact training improves bone mineral density and physical function in postmenopausal women with osteopenia and osteoporosis: the LIFTMOR randomized controlled trial. J Bone Miner Res. 2018;33(2):211–20. https://doi.org/10.1002/jbmr.3284.
Krishnamoorthy D, Frechette DM, Adler BJ, Green DE, Chan ME, Rubin CT. Marrow adipogenesis and bone loss that parallels estrogen deficiency is slowed by low-intensity mechanical signals. Osteoporos Int. 2016;27(2):747–56. https://doi.org/10.1007/s00198-015-3289-5.
Ma R, Zhu D, Gong H, Gu G, Huang X, Gao JZ, et al. High-frequency and low-magnitude whole body vibration with rest days is more effective in improving skeletal micro-morphology and biomechanical properties in ovariectomised rodents. Hip Int. 2012;22(2):218–26. https://doi.org/10.5301/HIP.2012.9033.
Rubin CT, Capilla E, Luu YK, Busa B, Crawford H, Nolan DJ, et al. Adipogenesis is inhibited by brief, daily exposure to high-frequency, extremely low-magnitude mechanical signals. Proc Natl Acad Sci U S A. 2007;104(45):17879–84. https://doi.org/10.1073/pnas.0708467104.
Styner M, Sen B, Xie Z, Case N, Rubin J. Indomethacin promotes adipogenesis of mesenchymal stem cells through a cyclooxygenase independent mechanism. J Cell Biochem. 2010;111(4):1042–50. https://doi.org/10.1002/jcb.22793.
Gong H, Zhang R, Gao J, Zhang M, Liu B, Zhang M, et al. Whole body vibration with rest days could improve bone quality of distal femoral metaphysis by regulating trabecular arrangement. Sci China Life Sci. 2019;62(1):95–103. https://doi.org/10.1007/s11427-017-9253-x.
Zhang T, Gao J, Fang J, Gong H. Multiscale investigation on the effects of additional weight bearing in combination with low-magnitude high-frequency vibration on bone quality of growing female rats. J Bone Miner Metab. 2018;36(2):157–69. https://doi.org/10.1007/s00774-017-0827-6.
Judex S, Lei X, Han D, Rubin C. Low-magnitude mechanical signals that stimulate bone formation in the ovariectomized rat are dependent on the applied frequency but not on the strain magnitude. J Biomech. 2007;40(6):1333–9. https://doi.org/10.1016/j.jbiomech.2006.05.014.
Luo X, Zhang J, Zhang C, He C, Wang P. The effect of whole-body vibration therapy on bone metabolism, motor function, and anthropometric parameters in women with postmenopausal osteoporosis. Disabil Rehabil. 2017;39(22):2315–23. https://doi.org/10.1080/09638288.2016.1226417.
Rubin C, Recker R, Cullen D, Ryaby J, McCabe J, McLeod K. Prevention of postmenopausal bone loss by a low-magnitude, high-frequency mechanical stimuli: a clinical trial assessing compliance, efficacy, and safety. J Bone Miner Res. 2004;19(3):343–51. https://doi.org/10.1359/JBMR.0301251.
Kiel DP, Hannan MT, Barton BA, Bouxsein ML, Sisson E, Lang T, et al. Low-magnitude mechanical stimulation to improve bone density in persons of advanced age: a randomized, placebo-controlled trial. J Bone Miner Res. 2015;30(7):1319–28. https://doi.org/10.1002/jbmr.2448.
Slatkovska L, Alibhai SMH, Beyene J, Hu H, Demaras A, Cheung AM. Effect of 12 months of whole-body vibration therapy on bone density and structure in postmenopausal women: a randomized trial. Ann Intern Med. 2011;155(10):668–79. https://doi.org/10.7326/0003-4819-155-10-201111150-00005.
Gilsanz V, Wren TA, Sanchez M, Dorey F, Judex S, Rubin C. Low-level, high-frequency mechanical signals enhance musculoskeletal development of young women with low BMD. J Bone Miner Res. 2006;21(9):1464–74. https://doi.org/10.1359/jbmr.060612.
Ward K, Alsop C, Caulton J, Rubin C, Adams J, Mughal Z. Low magnitude mechanical loading is osteogenic in children with disabling conditions. J Bone Miner Res. 2004;19(3):360–9. https://doi.org/10.1359/JBMR.040129.
Mogil RJ, Kaste SC, Ferry RJ, Hudson MM, Mulrooney DA, Howell CR, et al. Effect of low-magnitude, high-frequency mechanical stimulation on BMD among young childhood cancer survivors a randomized clinical trial. JAMA Oncol. 2016;2(7):908–14. https://doi.org/10.1001/jamaoncol.2015.6557.
Sen B, Xie Z, Case N, Styner M, Rubin CT, Rubin J. Mechanical signal influence on mesenchymal stem cell fate is enhanced by incorporation of refractory periods into the loading regimen. J Biomech. 2011;44(4):593–9. https://doi.org/10.1038/jid.2014.371.
Styner M, Meyer MB, Galior K, Case N, Xie Z, Sen B, et al. Mechanical strain downregulates C/EBPbeta in MSC and decreases endoplasmic reticulum stress. PLoS One. 2012;7(12):e51613. https://doi.org/10.1371/journal.pone.0051613.
David V, Martin A, Lafage-Proust MH, Malaval L, Peyroche S, Jones DB, et al. Mechanical loading down-regulates peroxisome proliferator-activated receptor γ in bone marrow stromal cells and favors osteoblastogenesis at the expense of adipogenesis. Endocrinology. 2007;148(5):2553–62. https://doi.org/10.1210/en.2006-1704.
Sen B, Xie Z, Case N, Ma M, Rubin C, Rubin J. Mechanical strain inhibits adipogenesis in mesenchymal stem cells by stimulating a durable β-catenin signal. Endocrinology. 2008;149(12):6065–75. https://doi.org/10.1210/en.2008-0687.
Sen B, Paradise CR, Xie Z, Sankaran J, Uzer G, Styner M, et al. β-Catenin preserves the stem state of murine bone marrow stromal cells through activation of EZH2. J Bone Miner Res Off J Am Soc Bone Miner Res. 2020. https://doi.org/10.1002/jbmr.3975.
Nedergaard A, Henriksen K, Karsdal MA, Christiansen C. Musculoskeletal ageing and primary prevention. Best Pract Res Clin Obstet Gynaecol. 2013;27(5):673–88. https://doi.org/10.1016/j.bpobgyn.2013.06.001.
Brown M. Skeletal muscle and bone: effect of sex steroids and aging. Am J Physiol Adv Physiol Educ. 2008;32(2):120–6. https://doi.org/10.1152/advan.90111.2008.
Syed FA, Oursler MJ, Hefferanm TE, Peterson JM, Riggs BL, Khosla S. Effects of estrogen therapy on bone marrow adipocytes in postmenopausal osteoporotic women. Osteoporos Int. 2008;19(9):1323–30. https://doi.org/10.1007/s00198-008-0574-6.
Khosla S, Oursler MJ, Monroe DG. Estrogen and the skeleton. Trends Endocrinol Metab. 2012;23(11):576–81. https://doi.org/10.1016/j.japh.2018.02.005.
Clarke BL, Khosla S. Androgens and bone. Steroids. 2009;74(3):296–305. https://doi.org/10.1385/1-59259-388-7:221.
Mistry SD, Woods GN, Sigurdsson S, Ewing SK, Hue TF, Eiriksdottir G, et al. Sex hormones are negatively associated with vertebral bone marrow fat. Bone. 2018;108(1):20–4. https://doi.org/10.1016/j.bone.2017.12.009.
Gavin KM, Sullivan TM, Kohrt WM, Majka SM, Klemm DJ. Ovarian hormones regulate the production of adipocytes from bone marrow-derived cells. Front Endocrinol (Lausanne). 2018;9(MAY):276. https://doi.org/10.3389/fendo.2018.00276.
Wright LE, Harhash AA, Kozlow WM, Waning DL, Regan JN, She Y, et al. Aromatase inhibitor-induced bone loss increases the progression of estrogen receptor-negative breast cancer in bone and exacerbates muscle weakness in vivo. Oncotarget. 2017;8(5):8406–19. https://doi.org/10.18632/oncotarget.14139.
Cawthorn WP, Scheller EL, Parlee SD, Pham HA, Learman BS, Redshaw CM, et al. Expansion of bone marrow adipose tissue during caloric restriction is associated with increased circulating glucocorticoids and not with hypoleptinemia. Endocrinology. 2016;157(2):508–21. https://doi.org/10.1210/en.2015-1477.
Khosla S. Leptin-central or peripheral to the regulation of bone metabolism? Endocrinology. 2002;143(11):4161–4. https://doi.org/10.1210/en.2002-220843.
Devlin MJ, Brooks DJ, Conlon C, Vliet M, Louis L, Rosen CJ, et al. Daily leptin blunts marrow fat but does not impact bone mass in calorie-restricted mice. J Endocrinol. 2016;229(3):295–306. https://doi.org/10.1530/JOE-15-0473.
Ackert-Bicknell CL, Shockley KR, Horton LG, Lecka-Czernik B, Churchill GA, Rosen CJ. Strain-specific effects of rosiglitazone on bone mass, body composition, and serum insulin-like growth factor-I. Endocrinology. 2009;150(3):1330–40. https://doi.org/10.1210/en.2008-0936.
Clemmons DR. Role of IGF-binding proteins in regulating IGF responses to changes in metabolism. J Mol Endocrinol. 2018;61(1):T139–T69. https://doi.org/10.1530/JME-18-0016.
Tian F, Wang Y, Bikle DD. IGF-1 signaling mediated cell-specific skeletal mechano-transduction. J Orthop Res. 2018;36(2):576–83. https://doi.org/10.1002/jor.23767.
Xi G, Shen X, Rosen CJ, Clemmons DR. IRS-1 functions as a molecular scaffold to coordinate IGF-I/IGFBP-2 signaling during osteoblast differentiation. J Bone Miner Res Off J Am Soc Bone Miner Res. 2016;31(6):1300–14. https://doi.org/10.1002/jbmr.2791.
Diedrich JD, Rajagurubandara E, Herroon MK, Mahapatra G, Hüttemann M, Podgorski I. Bone marrow adipocytes promote the warburg phenotype in metastatic prostate tumors via HIF-1α activation. Oncotarget. 2016;7(40):64854–77. https://doi.org/10.18632/oncotarget.11712.
Morris EV, Edwards CM. Bone marrow adipose tissue: a new player in cancer metastasis to bone. Front Endocrinol (Lausanne). 2016;7(JUL):90. https://doi.org/10.3389/fendo.2016.00090.
Luo G, He Y, Yu X. Bone marrow adipocyte: an intimate partner with tumor cells in bone metastasis. Front Endocrinol (Lausanne). 2018;9(JUL):339. https://doi.org/10.3389/fendo.2018.00339.
Diedrich JD, Herroon MK, Rajagurubandara E, Podgorski I. The lipid side of bone marrow adipocytes: how tumor cells adapt and survive in bone. Curr Osteoporos Rep. 2018;16(4):443–57. https://doi.org/10.1007/s11914-018-0453-9.
Reagan MR. Critical assessment of in vitro and in vivo models to study marrow adipose tissue. Curr Osteoporos Rep. 2020;18(2):85–94. https://doi.org/10.1007/s11914-020-00569-4.
Funding
This review was supported by funds from the NIH/NIAMS R01AR073264 and NIH/NCATS KL2TR002490.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors have no conflicts of interest to report.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Ethics Approval
Not applicable.
Consent to Participate
Not applicable.
Consent for Publication
Not applicable.
Code Availability
Not applicable.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of Topical Collection on Bone Marrow and Adipose Tissue
Rights and permissions
About this article
Cite this article
Little-Letsinger, S.E., Pagnotti, G.M., McGrath, C. et al. Exercise and Diet: Uncovering Prospective Mediators of Skeletal Fragility in Bone and Marrow Adipose Tissue. Curr Osteoporos Rep 18, 774–789 (2020). https://doi.org/10.1007/s11914-020-00634-y
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11914-020-00634-y