Abstract
Purpose of Review
Heart failure with preserved ejection fraction mainly affects the elderly. The obesity phenotype of heart failure with preserved ejection fraction reflects the coexistence of two highly prevalent conditions in the elderly. Obesity may also lead to heart failure with preserved ejection fraction in middle-aged persons, especially in African American women.
Recent Findings
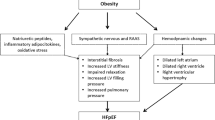
Obesity is twice as common in middle-aged than in elderly persons with heart failure with preserved ejection fraction. Obese middle-aged persons with heart failure with preserved ejection fraction are less likely to be Caucasian and to have atrial fibrillation or chronic kidney disease as comorbidities than elderly patients with heart failure with preserved ejection fraction. Obesity-associated low-grade systemic inflammation may induce/heighten inflammatory activation of the coronary microvascular endothelium, leading to cardiomyocyte hypertrophy/ stiffness, myocardial fibrosis, and left ventricular diastolic dysfunction.
Summary
Both substantial weight reduction with bariatric surgery and lesser levels of weight reduction with caloric restriction are promising therapeutic approaches to obesity-induced heart failure with preserved ejection fraction.

Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: •• Of major importance
Flegal KM, Kruszon-Moran D, Carroll MD, Fryar CD, Ogden CL. Trends in obesity among adults in the United States, 2005 to 2014. JAMA. 2016;315(21):2284–91. https://doi.org/10.1001/jama.2016.6458.
Jackson SE, Llewellyn CH, Smith L. The obesity epidemic - nature via nurture: a narrative review of high-income countries. SAGE Open Med. 2020;8:2050312120918265. https://doi.org/10.1177/2050312120918265.
Turer AT, Hill JA, Elmquist JK, Scherer PE. Adipose tissue biology and cardiomyopathy: translational implications. Circ Res. 2012;111(12):1565–77. https://doi.org/10.1161/CIRCRESAHA.111.262493.
Aurigemma GP, de Simone G, Fitzgibbons TP. Cardiac remodeling in obesity. Circ Cardiovasc Imaging. 2013;6(1):142–52. https://doi.org/10.1161/CIRCIMAGING.111.964627.
Szczepaniak LS, Victor RG, Orci L, Unger RH. Forgotten but not gone: the rediscovery of fatty heart, the most common unrecognized disease in America. Circ Res. 2007;101(8):759–67. https://doi.org/10.1161/CIRCRESAHA.107.160457.
Turkbey EB, McClelland RL, Kronmal RA, Burke GL, Bild DE, Tracy RP, et al. The impact of obesity on the left ventricle: the multi-ethnic study of atherosclerosis (MESA). JACC Cardiovasc Imaging. 2010;3(3):266–74. https://doi.org/10.1016/j.jcmg.2009.10.012.
Tsao CW, Lyass A, Enserro D, Larson MG, Ho JE, Kizer JR, et al. Temporal trends in the incidence of and mortality associated with heart failure with preserved and reduced ejection fraction. JACC Heart Fail. 2018;6(8):678–85. https://doi.org/10.1016/j.jchf.2018.03.006.
•• Savji N, Meijers WC, Bartz TM, Bhambhani V, Cushman M, Nayor M, et al. The association of obesity and cardiometabolic traits with incident HFpEF and HFrEF. JACC Heart Fail. 2018;6(8):701–9. https://doi.org/10.1016/j.jchf.2018.05.018The data from 4 community-based cohorts clearly establishthat obesity is a risk for HFpEF especially in women.
Gupta DK, Shah AM, Castagno D, Takeuchi M, Loehr LR, Fox ER, et al. Heart failure with preserved ejection fraction in African Americans: the ARIC (atherosclerosis risk in communities) study. JACC Heart Fail. 2013;1(2):156–63. https://doi.org/10.1016/j.jchf.2013.01.003.
Aune D, Sen A, Norat T, Janszky I, Romundstad P, Tonstad S, et al. Body mass index, abdominal fatness, and heart failure incidence and mortality: a systematic review and dose-response meta-analysis of prospective studies. Circulation. 2016;133(7):639–49. https://doi.org/10.1161/CIRCULATIONAHA.115.016801.
Yan Y, Li S, Guo Y, Fernandez C, Bazzano L, He J, et al. Life-course cumulative burden of body mass index and blood pressure on progression of left ventricular mass and geometry in midlife: the Bogalusa heart study. Circ Res. 2020;126(5):633–43. https://doi.org/10.1161/CIRCRESAHA.119.316045.
Peterson LR, Waggoner AD, Schechtman KB, Meyer T, Gropler RJ, Barzilai B, et al. Alterations in left ventricular structure and function in young healthy obese women: assessment by echocardiography and tissue Doppler imaging. J Am Coll Cardiol. 2004;43(8):1399–404. https://doi.org/10.1016/j.jacc.2003.10.062.
De Simone G, Devereux RB, Chinali M, Roman MJ, Barac A, Panza JA, et al. Sex differences in obesity-related changes in left ventricular morphology: the strong heart study. J Hypertens. 2011;29(7):1431–8. https://doi.org/10.1097/HJH.0b013e328347a093.
Powell BD, Redfield MM, Bybee KA, Freeman WK, Rihal CS. Association of obesity with left ventricular remodeling and diastolic dysfunction in patients without coronary artery disease. Am J Cardiol. 2006;98(1):116–20. https://doi.org/10.1016/j.amjcard.2006.01.063.
Rozenbaum Z, Topilsky Y, Khoury S, Pereg D, Laufer-Perl M. Association of body mass index and diastolic function in metabolically healthy obese with preserved ejection fraction. Int J Cardiol. 2019;277:147–52. https://doi.org/10.1016/j.ijcard.2018.08.008.
Campbell DJ, Gong FF, Jelinek MV, Castro JM, Coller JM, McGrady M, et al. Threshold body mass index and sex-specific waist circumference for increased risk of heart failure with preserved ejection fraction. Eur J Prev Cardiol. 2019;26(15):1594–602. https://doi.org/10.1177/2047487319851298.
Russo C, Jin Z, Homma S, Rundek T, Elkind MS, Sacco RL, et al. Effect of obesity and overweight on left ventricular diastolic function: a community-based study in an elderly cohort. J Am Coll Cardiol. 2011;57(12):1368–74. https://doi.org/10.1016/j.jacc.2010.10.042.
Steinberg BA, Zhao X, Heidenreich PA, Peterson ED, Bhatt DL, Cannon CP, et al. Trends in patients hospitalized with heart failure and preserved left ventricular ejection fraction: prevalence, therapies, and outcomes. Circulation. 2012;126(1):65–75. https://doi.org/10.1161/CIRCULATIONAHA.111.080770.
•• Stolfo D, Uijl A, Vedin O, Strömberg A, Faxén UL, Rosano GMC, et al. Sex-Based Differences in Heart Failure Across the Ejection Fraction Spectrum: Phenotyping, and Prognostic and Therapeutic Implications. JACC Heart Fail. 2019;7(6):505–15. https://doi.org/10.1016/j.jchf.2019.03.011Recent data from the Swedish Heart Failure Registry confirm that in contrast to HFrEF HFpEF affect predominantly women.
Salton CJ, Chuang ML, O'Donnell CJ, Kupka MJ, Larson MG, Kissinger KV, et al. Gender differences and normal left ventricular anatomy in an adult population free of hypertension. A cardiovascular magnetic resonance study of the Framingham Heart Study Offspring cohort. J Am Coll Cardiol. 2002;39(6):1055–60. https://doi.org/10.1016/s0735-1097(02)01712-6.
Gori M, Lam CS, Gupta DK, Santos AB, Cheng S, Shah AM, et al. Sex-specific cardiovascular structure and function in heart failure with preserved ejection fraction. Eur J Heart Fail. 2014;16(5):535–42. https://doi.org/10.1002/ejhf.67.
Pandey A, Omar W, Ayers C, LaMonte M, Klein L, Allen NB, et al. Sex and race differences in lifetime risk of heart failure with preserved ejection fraction and heart failure with reduced ejection fraction. Circulation. 2018;137(17):1814–23. https://doi.org/10.1161/CIRCULATIONAHA.117.031622.
Dunlay SM, Roger VL, Redfield MM. Epidemiology of heart failure with preserved ejection fraction. Nat Rev Cardiol. 2017;14(10):591–602. https://doi.org/10.1038/nrcardio.2017.65.
Ho JE, Enserro D, Brouwers FP, Kizer JR, Shah SJ, Psaty BM, et al. Predicting heart failure with preserved and reduced ejection fraction: The International Collaboration on Heart Failure Subtypes. Circ Heart Fail. 2016;9(6). https://doi.org/10.1161/CIRCHEARTFAILURE.115.003116.
Tadic M, Cuspidi C, Plein S, Belyavskiy E, Heinzel F, Galderisi M. Sex and heart failure with preserved ejection fraction: from pathophysiology to clinical studies. J Clin Med. 2019;8(6). https://doi.org/10.3390/jcm8060792.
Benjamin EJ, Virani SS, Callaway CW, Chamberlain AM, Chang AR, Cheng S, et al. Heart disease and stroke Statistics-2018 update: a report from the American Heart Association. Circulation. 2018;137(12):e67–e492. https://doi.org/10.1161/CIR.0000000000000558.
Drazner MH, Dries DL, Peshock RM, Cooper RS, Klassen C, Kazi F, et al. Left ventricular hypertrophy is more prevalent in blacks than whites in the general population: the Dallas Heart Study. Hypertension. 2005;46(1):124–9. https://doi.org/10.1161/01.HYP.0000169972.96201.8e.
Morris AA, Patel RS, Binongo JN, Poole J, Al Mheid I, Ahmed Y, et al. Racial differences in arterial stiffness and microcirculatory function between Black and White Americans. J Am Heart Assoc. 2013;2(2):e002154. https://doi.org/10.1161/JAHA.112.002154.
Krishnamoorthy A, Greiner MA, Bertoni AG, Eapen ZJ, O'Brien EC, Curtis LH, et al. The obesity and heart failure epidemics among African Americans: insights from the Jackson Heart Study. J Card Fail. 2016;22(8):589–97. https://doi.org/10.1016/j.cardfail.2016.03.004.
Buffington CK, Marema RT. Ethnic differences in obesity and surgical weight loss between African-American and Caucasian females. Obes Surg. 2006;16(2):159–65. https://doi.org/10.1381/096089206775565258.
Eaton CB, Pettinger M, Rossouw J, Martin LW, Foraker R, Quddus A, et al. Risk factors for incident hospitalized heart failure with preserved versus reduced ejection fraction in a multiracial cohort of postmenopausal women. Circ Heart Fail. 2016;9(10). https://doi.org/10.1161/CIRCHEARTFAILURE.115.002883.
East MA, Peterson ED, Shaw LK, Gattis WA, O'Connor CM. Racial differences in the outcomes of patients with diastolic heart failure. Am Heart J. 2004;148(1):151–6. https://doi.org/10.1016/j.ahj.2004.01.017.
Lekavich CL, Barksdale DJ. A critical evaluation of the representation of black patients with heart failure and preserved ejection fraction in clinical trials: a literature review. J Cardiovasc Nurs. 2016;31(3):202–8. https://doi.org/10.1097/JCN.0000000000000237.
Goyal P, Paul T, Almarzooq ZI, Peterson JC, Krishnan U, Swaminathan RV, et al. Sex- and race-related differences in characteristics and outcomes of hospitalizations for heart failure with preserved ejection fraction. J Am Heart Assoc. 2017;6(4). https://doi.org/10.1161/JAHA.116.003330.
Vivo RP, Krim SR, Liang L, Neely M, Hernandez AF, Eapen ZJ, et al. Short- and long-term rehospitalization and mortality for heart failure in 4 racial/ethnic populations. J Am Heart Assoc. 2014;3(5):e001134. https://doi.org/10.1161/JAHA.114.001134.
Paulus WJ, Tschöpe C. A novel paradigm for heart failure with preserved ejection fraction: comorbidities drive myocardial dysfunction and remodeling through coronary microvascular endothelial inflammation. J Am Coll Cardiol. 2013;62(4):263–71. https://doi.org/10.1016/j.jacc.2013.02.092.
•• Franssen C, Chen S, Unger A, Korkmaz HI, De Keulenaer GW, Tschöpe C, et al. Myocardial Microvascular Inflammatory Endothelial Activation in Heart Failure With Preserved Ejection Fraction. JACC Heart Fail. 2016;4(4):312–24. https://doi.org/10.1016/j.jchf.2015.10.007Human and experimental data that link HFpEF to coronary microvascular endothelial activation and oxidative stress.
Després JP. Body fat distribution and risk of cardiovascular disease: an update. Circulation. 2012;126(10):1301–13. https://doi.org/10.1161/CIRCULATIONAHA.111.067264.
Rubin R. Postmenopausal women with a “normal” BMI might be overweight or even obese. JAMA. 2018;319(12):1185–7. https://doi.org/10.1001/jama.2018.0423.
Neeland IJ, Gupta S, Ayers CR, Turer AT, Rame JE, Das SR, et al. Relation of regional fat distribution to left ventricular structure and function. Circ Cardiovasc Imaging. 2013;6(5):800–7. https://doi.org/10.1161/CIRCIMAGING.113.000532.
Abbasi SA, Hundley WG, Bluemke DA, Jerosch-Herold M, Blankstein R, Petersen SE, et al. Visceral adiposity and left ventricular remodeling: the multi-ethnic study of atherosclerosis. Nutr Metab Cardiovasc Dis. 2015;25(7):667–76. https://doi.org/10.1016/j.numecd.2015.03.016.
de Simone G, Izzo R, De Luca N, Gerdts E. Left ventricular geometry in obesity: is it what we expect? Nutr Metab Cardiovasc Dis. 2013;23(10):905–12. https://doi.org/10.1016/j.numecd.2013.06.012.
Rao VN, Zhao D, Allison MA, Guallar E, Sharma K, Criqui MH, et al. Adiposity and incident heart failure and its subtypes: MESA (multi-ethnic study of atherosclerosis). JACC Heart Fail. 2018;6(12):999–1007. https://doi.org/10.1016/j.jchf.2018.07.009.
•• Tsujimoto T, Kajio H. Abdominal obesity is associated with an increased risk of all-cause mortality in patients with HFpEF. J Am Coll Cardiol. 2017;70(22):2739–49. https://doi.org/10.1016/j.jacc.2017.09.1111Analysis of TOPCAT indicates that the amount of abdominal obesity; i.e., visceral adipose tiissue plays an essential role in the clinical outcome of HFpEF.
Després JP, Lemieux I. Abdominal obesity and metabolic syndrome. Nature. 2006;444(7121):881–7. https://doi.org/10.1038/nature05488.
Blackburn P, Després JP, Lamarche B, Tremblay A, Bergeron J, Lemieux I, et al. Postprandial variations of plasma inflammatory markers in abdominally obese men. Obesity (Silver Spring). 2006;14(10):1747–54. https://doi.org/10.1038/oby.2006.201.
Visser M, Bouter LM, McQuillan GM, Wener MH, Harris TB. Elevated C-reactive protein levels in overweight and obese adults. JAMA. 1999;282(22):2131–5. https://doi.org/10.1001/jama.282.22.2131.
Pou KM, Massaro JM, Hoffmann U, Vasan RS, Maurovich-Horvat P, Larson MG, et al. Visceral and subcutaneous adipose tissue volumes are cross-sectionally related to markers of inflammation and oxidative stress: the Framingham Heart Study. Circulation. 2007;116(11):1234–41. https://doi.org/10.1161/CIRCULATIONAHA.107.710509.
Wernstedt Asterholm I, Tao C, Morley TS, Wang QA, Delgado-Lopez F, Wang ZV, et al. Adipocyte inflammation is essential for healthy adipose tissue expansion and remodeling. Cell Metab. 2014;20(1):103–18. https://doi.org/10.1016/j.cmet.2014.05.005.
Lumeng CN, Bodzin JL, Saltiel AR. Obesity induces a phenotypic switch in adipose tissue macrophage polarization. J Clin Invest. 2007;117(1):175–84. https://doi.org/10.1172/JCI29881.
Reilly SM, Saltiel AR. Adapting to obesity with adipose tissue inflammation. Nat Rev Endocrinol. 2017;13(11):633–43. https://doi.org/10.1038/nrendo.2017.90.
Lee YS, Wollam J, Olefsky JM. An integrated view of Immunometabolism. Cell. 2018;172(1–2):22–40. https://doi.org/10.1016/j.cell.2017.12.025.
Amano SU, Cohen JL, Vangala P, Tencerova M, Nicoloro SM, Yawe JC, et al. Local proliferation of macrophages contributes to obesity-associated adipose tissue inflammation. Cell Metab. 2014;19(1):162–71. https://doi.org/10.1016/j.cmet.2013.11.017.
Schlecht I, Fischer B, Behrens G, Leitzmann MF. Relations of visceral and abdominal subcutaneous adipose tissue, body mass index, and waist circumference to serum concentrations of parameters of chronic inflammation. Obes Facts. 2016;9(3):144–57. https://doi.org/10.1159/000443691.
Khera A, Vega GL, Das SR, Ayers C, McGuire DK, Grundy SM, et al. Sex differences in the relationship between C-reactive protein and body fat. J Clin Endocrinol Metab. 2009;94(9):3251–8. https://doi.org/10.1210/jc.2008-2406.
Denis GV, Sebastiani P, Bertrand KA, Strissel KJ, Tran AH, Slama J, et al. Inflammatory signatures distinguish metabolic health in African American women with obesity. PLoS One. 2018;13(5):e0196755. https://doi.org/10.1371/journal.pone.0196755.
DeBerge M, Shah SJ, Wilsbacher L, Thorp EB. Macrophages in heart failure with reduced versus preserved ejection fraction. Trends Mol Med. 2019;25(4):328–40. https://doi.org/10.1016/j.molmed.2019.01.002.
Paulus WJ. Unfolding discoveries in heart failure. N Engl J Med. 2020;382(7):679–82. https://doi.org/10.1056/NEJMcibr1913825.
Mohammed SF, Hussain I, AbouEzzeddine OF, Abou Ezzeddine OF, Takahama H, Kwon SH, et al. Right ventricular function in heart failure with preserved ejection fraction: a community-based study. Circulation. 2014;130(25):2310–20. https://doi.org/10.1161/CIRCULATIONAHA.113.008461.
Zeng H, Chen JX. Microvascular rarefaction and heart failure with preserved ejection fraction. Front Cardiovasc Med. 2019;6:15. https://doi.org/10.3389/fcvm.2019.00015.
Bajaj NS, Osborne MT, Gupta A, Tavakkoli A, Bravo PE, Vita T, et al. Coronary microvascular dysfunction and cardiovascular risk in obese patients. J Am Coll Cardiol. 2018;72(7):707–17. https://doi.org/10.1016/j.jacc.2018.05.049.
Zylke JW, Bauchner H. The unrelenting challenge of obesity. JAMA. 2016;315(21):2277–8. https://doi.org/10.1001/jama.2016.6190.
•• Maslov PZ, Kim JK, Argulian E, Ahmadi A, Narula N, Singh M, et al. Is Cardiac Diastolic Dysfunction a Part of Post-Menopausal Syndrome? JACC Heart Fail. 2019;7(3):192–203. https://doi.org/10.1016/j.jchf.2018.12.018Post-menopausal women gain a lot of weight that, in addition to estrogen deficiency, leads to the development and progression of HFpEF.
Haass M, Kitzman DW, Anand IS, Miller A, Zile MR, Massie BM, et al. Body mass index and adverse cardiovascular outcomes in heart failure patients with preserved ejection fraction: results from the Irbesartan in Heart Failure with Preserved Ejection Fraction (I-PRESERVE) trial. Circ Heart Fail. 2011;4(3):324–31. https://doi.org/10.1161/CIRCHEARTFAILURE.110.959890.
Foppa M, Arora G, Gona P, Ashrafi A, Salton CJ, Yeon SB, et al. Right ventricular volumes and systolic function by cardiac magnetic resonance and the impact of sex, age, and obesity in a longitudinally followed cohort free of pulmonary and cardiovascular disease: the Framingham Heart Study. Circ Cardiovasc Imaging. 2016;9(3):e003810. https://doi.org/10.1161/CIRCIMAGING.115.003810.
McQuillan BM, Picard MH, Leavitt M, Weyman AE. Clinical correlates and reference intervals for pulmonary artery systolic pressure among echocardiographically normal subjects. Circulation. 2001;104(23):2797–802. https://doi.org/10.1161/hc4801.100076.
Reddy YNV, Lewis GD, Shah SJ, Obokata M, Abou-Ezzedine OF, Fudim M, et al. Characterization of the obese phenotype of heart failure with preserved ejection fraction: a RELAX trial ancillary study. Mayo Clin Proc. 2019;94(7):1199–209. https://doi.org/10.1016/j.mayocp.2018.11.037.
Obokata M, Reddy YNV, Pislaru SV, Melenovsky V, Borlaug BA. Evidence supporting the existence of a distinct obese phenotype of heart failure with preserved ejection fraction. Circulation. 2017;136(1):6–19. https://doi.org/10.1161/CIRCULATIONAHA.116.026807.
•• Tromp J, MacDonald MR, Tay WT, Teng TK, Hung CL, Narasimhan C, et al. Heart failure with preserved ejection fraction in the young. Circulation. 2018;138(24):2763–73. https://doi.org/10.1161/CIRCULATIONAHA.118.034720The distinctive features of HFpEF in middle-aged patients are outlined for the first time. Middle-aged patients were twice more likely to be obese than elderly patients with HFpEF in the Asian sudden death in heart failure (ASIAN-HF) registry.
•• Tromp J, Shen L, Jhund PS, Anand IS, Carson PE, Desai AS, et al. Age-related characteristics and outcomes of patients with heart failure with preserved ejection fraction. J Am Coll Cardiol. 2019;74(5):601–12. https://doi.org/10.1016/j.jacc.2019.05.052Younger patients with HFpEF were also more likely to be obese than elderly patients in the I-PRESERVE (Irbesartan in heart failure with preserved systolic function and CHARM (Candesartan cilexetil in heart failure assessment of reduction of mortality and morbidity) trials.
Powell-Wiley TM, Ngwa J, Kebede S, Lu D, Schulte PJ, Bhatt DL, et al. Impact of body mass index on heart failure by race/ethnicity from the get with the guidelines-heart failure (GWTG-HF) registry. JACC Heart Fail. 2018;6(3):233–42. https://doi.org/10.1016/j.jchf.2017.11.011.
Klapholz M, Maurer M, Lowe AM, Messineo F, Meisner JS, Mitchell J, et al. Hospitalization for heart failure in the presence of a normal left ventricular ejection fraction: results of the New York heart failure registry. J Am Coll Cardiol. 2004;43(8):1432–8. https://doi.org/10.1016/j.jacc.2003.11.040.
Melenovsky V, Borlaug BA, Rosen B, Hay I, Ferruci L, Morell CH, et al. Cardiovascular features of heart failure with preserved ejection fraction versus nonfailing hypertensive left ventricular hypertrophy in the urban Baltimore community: the role of atrial remodeling/dysfunction. J Am Coll Cardiol. 2007;49(2):198–207. https://doi.org/10.1016/j.jacc.2006.08.050.
Samson R, Jaiswal A, Ennezat PV, Cassidy M, Le Jemtel TH. Clinical phenotypes in heart failure with preserved ejection fraction. J Am Heart Assoc. 2016;5(1). doi:https://doi.org/10.1161/JAHA.115.002477.
Susmallian S, Raziel A, Barnea R, Paran H. Bariatric surgery in older adults: should there be an age limit? Medicine (Baltimore). 2019;98(3):e13824. https://doi.org/10.1097/MD.0000000000013824.
Persson CE, Björck L, Lagergren J, Lappas G, Giang KW, Rosengren A. Risk of heart failure in obese patients with and without bariatric surgery in Sweden-a registry-based study. J Card Fail. 2017;23(7):530–7. https://doi.org/10.1016/j.cardfail.2017.05.005.
Sundström J, Bruze G, Ottosson J, Marcus C, Näslund I, Neovius M. Weight loss and heart failure: a nationwide study of gastric bypass surgery versus intensive lifestyle treatment. Circulation. 2017;135(17):1577–85. https://doi.org/10.1161/CIRCULATIONAHA.116.025629.
Benotti PN, Wood GC, Carey DJ, Mehra VC, Mirshahi T, Lent MR, et al. Gastric bypass surgery produces a durable reduction in cardiovascular disease risk factors and reduces the long-term risks of congestive heart failure. J Am Heart Assoc. 2017;6(5). https://doi.org/10.1161/JAHA.116.005126.
Kindel TL, Strande JL. Bariatric surgery as a treatment for heart failure: review of the literature and potential mechanisms. Surg Obes Relat Dis. 2018;14(1):117–22. https://doi.org/10.1016/j.soard.2017.09.534.
Vest AR. Has the time come to be more aggressive with bariatric surgery in obese patients with chronic systolic heart failure? Curr Heart Fail Rep. 2018;15(3):171–80. https://doi.org/10.1007/s11897-018-0390-z.
de las Fuentes L, Waggoner AD, Mohammed BS, Stein RI, Miller BV, Foster GD, et al. Effect of moderate diet-induced weight loss and weight regain on cardiovascular structure and function. J Am Coll Cardiol. 2009;54(25):2376–81. https://doi.org/10.1016/j.jacc.2009.07.054.
Rider OJ, Francis JM, Ali MK, Petersen SE, Robinson M, Robson MD, et al. Beneficial cardiovascular effects of bariatric surgical and dietary weight loss in obesity. J Am Coll Cardiol. 2009;54(8):718–26. https://doi.org/10.1016/j.jacc.2009.02.086.
Le Jemtel TH, Samson R, Jaiswal A, Lewine EB, Oparil S. Regression of left ventricular mass after bariatric surgery. Curr Hypertens Rep. 2017;19(9):68. https://doi.org/10.1007/s11906-017-0767-5.
Grapsa J, Tan TC, Paschou SA, Kalogeropoulos AS, Shimony A, Kaier T, et al. The effect of bariatric surgery on echocardiographic indices: a review of the literature. Eur J Clin Investig. 2013;43(11):1224–30. https://doi.org/10.1111/eci.12162.
Alpert MA, Omran J, Mehra A, Ardhanari S. Impact of obesity and weight loss on cardiac performance and morphology in adults. Prog Cardiovasc Dis. 2014;56(4):391–400. https://doi.org/10.1016/j.pcad.2013.09.003.
Ashrafian H, le Roux CW, Darzi A, Athanasiou T. Effects of bariatric surgery on cardiovascular function. Circulation. 2008;118(20):2091–102. https://doi.org/10.1161/CIRCULATIONAHA.107.721027.
Kurnicka K, Domienik-Karłowicz J, Lichodziejewska B, Bielecki M, Kozłowska M, Goliszek S, et al. Improvement of left ventricular diastolic function and left heart morphology in young women with morbid obesity six months after bariatric surgery. Cardiol J. 2018;25(1):97–105. https://doi.org/10.5603/CJ.a2017.0059.
Leung M, Xie M, Durmush E, Leung DY, Wong VW. Weight loss with sleeve gastrectomy in obese type 2 diabetes mellitus: impact on cardiac function. Obes Surg. 2016;26(2):321–6. https://doi.org/10.1007/s11695-015-1748-x.
Owan T, Avelar E, Morley K, Jiji R, Hall N, Krezowski J, et al. Favorable changes in cardiac geometry and function following gastric bypass surgery: 2-year follow-up in the Utah obesity study. J Am Coll Cardiol. 2011;57(6):732–9. https://doi.org/10.1016/j.jacc.2010.10.017.
Aggarwal R, Harling L, Efthimiou E, Darzi A, Athanasiou T, Ashrafian H. The effects of bariatric surgery on cardiac structure and function: a systematic review of cardiac imaging outcomes. Obes Surg. 2016;26(5):1030–40. https://doi.org/10.1007/s11695-015-1866-5.
Cuspidi C, Rescaldani M, Tadic M, Sala C, Grassi G. Effects of bariatric surgery on cardiac structure and function: a systematic review and meta-analysis. Am J Hypertens. 2014;27(2):146–56. https://doi.org/10.1093/ajh/hpt215.
Garza CA, Pellikka PA, Somers VK, Sarr MG, Collazo-Clavell ML, Korenfeld Y, et al. Structural and functional changes in left and right ventricles after major weight loss following bariatric surgery for morbid obesity. Am J Cardiol. 2010;105(4):550–6. https://doi.org/10.1016/j.amjcard.2009.09.057.
Algahim MF, Lux TR, Leichman JG, Boyer AF, Miller CC, Laing ST, et al. Progressive regression of left ventricular hypertrophy two years after bariatric surgery. Am J Med. 2010;123(6):549–55. https://doi.org/10.1016/j.amjmed.2009.11.020.
Mikhalkova D, Holman SR, Jiang H, Saghir M, Novak E, Coggan AR, et al. Bariatric surgery-induced cardiac and lipidomic changes in obesity-related heart failure with preserved ejection fraction. Obesity (Silver Spring). 2018;26(2):284–90. https://doi.org/10.1002/oby.22038.
Gaborit B, Jacquier A, Kober F, Abdesselam I, Cuisset T, Boullu-Ciocca S, et al. Effects of bariatric surgery on cardiac ectopic fat: lesser decrease in epicardial fat compared to visceral fat loss and no change in myocardial triglyceride content. J Am Coll Cardiol. 2012;60(15):1381–9. https://doi.org/10.1016/j.jacc.2012.06.016.
Lehmann S, Linder N, Retschlag U, Schaudinn A, Stange R, Garnov N, et al. MRI assessment of changes in adipose tissue parameters after bariatric surgery. PLoS One. 2018;13(11):e0206735. https://doi.org/10.1371/journal.pone.0206735.
Otto M, Färber J, Haneder S, Michaely H, Kienle P, Hasenberg T. Postoperative changes in body composition--comparison of bioelectrical impedance analysis and magnetic resonance imaging in bariatric patients. Obes Surg. 2015;25(2):302–9. https://doi.org/10.1007/s11695-014-1382-z.
Meyer-Gerspach AC, Peterli R, Moor M, Madörin P, Schötzau A, Nabers D, et al. Quantification of liver, subcutaneous, and visceral adipose tissues by MRI before and after bariatric surgery. Obes Surg. 2019;29(9):2795–805. https://doi.org/10.1007/s11695-019-03897-2.
Toro-Ramos T, Goodpaster BH, Janumala I, Lin S, Strain GW, Thornton JC, et al. Continued loss in visceral and intermuscular adipose tissue in weight-stable women following bariatric surgery. Obesity (Silver Spring). 2015;23(1):62–9. https://doi.org/10.1002/oby.20932.
Korner J, Punyanitya M, Taveras C, McMahon DJ, Kim HJ, Inabnet W, et al. Sex differences in visceral adipose tissue post-bariatric surgery compared to matched non-surgical controls. Int J Body Compos Res. 2008;6(3):93–9.
Illán-Gómez F, Gonzálvez-Ortega M, Orea-Soler I, Alcaraz-Tafalla MS, Aragón-Alonso A, Pascual-Díaz M, et al. Obesity and inflammation: change in adiponectin, C-reactive protein, tumour necrosis factor-alpha and interleukin-6 after bariatric surgery. Obes Surg. 2012;22(6):950–5. https://doi.org/10.1007/s11695-012-0643-y.
Schmatz R, Bitencourt MR, Patias LD, Beck M, da C Alvarez G, Zanini D et al. Evaluation of the biochemical, inflammatory and oxidative profile of obese patients given clinical treatment and bariatric surgery. Clin Chim Acta 2017;465:72–79. doi:https://doi.org/10.1016/j.cca.2016.12.012.
Williams DB, Hagedorn JC, Lawson EH, Galanko JA, Safadi BY, Curet MJ, et al. Gastric bypass reduces biochemical cardiac risk factors. Surg Obes Relat Dis. 2007;3(1):8–13. https://doi.org/10.1016/j.soard.2006.10.003.
Viana EC, Araujo-Dasilio KL, Miguel GP, Bressan J, Lemos EM, Moyses MR, et al. Gastric bypass and sleeve gastrectomy: the same impact on IL-6 and TNF-α. prospective clinical trial. Obes Surg. 2013;23(8):1252–61. https://doi.org/10.1007/s11695-013-0894-2.
Freitas WR, Oliveira LVF, Perez EA, Ilias EJ, Lottenberg CP, Silva AS, et al. Systemic inflammation in severe obese patients undergoing surgery for obesity and weight-related diseases. Obes Surg. 2018;28(7):1931–42. https://doi.org/10.1007/s11695-017-3104-9.
Chiappetta S, Schaack HM, Wölnerhannsen B, Stier C, Squillante S, Weiner RA. The impact of obesity and metabolic surgery on chronic inflammation. Obes Surg. 2018;28(10):3028–40. https://doi.org/10.1007/s11695-018-3320-y.
Rao SR. Inflammatory markers and bariatric surgery: a meta-analysis. Inflamm Res. 2012;61(8):789–807. https://doi.org/10.1007/s00011-012-0473-3.
Askarpour M, Khani D, Sheikhi A, Ghaedi E, Alizadeh S. Effect of bariatric surgery on serum inflammatory factors of obese patients: a systematic review and meta-analysis. Obes Surg. 2019;29(8):2631–47. https://doi.org/10.1007/s11695-019-03926-0.
Heilbronn LK, de Jonge L, Frisard MI, DeLany JP, Larson-Meyer DE, Rood J, et al. Effect of 6-month calorie restriction on biomarkers of longevity, metabolic adaptation, and oxidative stress in overweight individuals: a randomized controlled trial. JAMA. 2006;295(13):1539–48. https://doi.org/10.1001/jama.295.13.1539.
•• Kraus WE, Bhapkar M, Huffman KM, Pieper CF, Krupa Das S, Redman LM, et al. 2 years of calorie restriction and cardiometabolic risk (CALERIE): exploratory outcomes of a multicentre, phase 2, randomised controlled trial. Lancet Diabetes Endocrinol. 2019;7(9):673–83. https://doi.org/10.1016/S2213-8587(19)30151-2First demonstration of the beneficial effect of caloric restriction for 2 years on cardiometabolic risk factors in healthy, non-obese, young and middle-aged persons.
Romashkan SV, Das SK, Villareal DT, Ravussin E, Redman LM, Rochon J, et al. Safety of two-year caloric restriction in non-obese healthy individuals. Oncotarget. 2016;7(15):19124–33. https://doi.org/10.18632/oncotarget.8093.
•• Redman LM, Smith SR, Burton JH, Martin CK, Il'yasova D, Ravussin E. Metabolic slowing and reduced oxidative damage with sustained caloric restriction support the rate of living and oxidative damage theories of aging. Cell Metab. 2018;27(4):805–15.e4. https://doi.org/10.1016/j.cmet.2018.02.019Sustained caloric restriction reduces oxidative damage and is thought to induce a slowing of energy metabolism that may delay aging and possibly increase life expectancy.
Most J, Gilmore LA, Smith SR, Han H, Ravussin E, Redman LM. Significant improvement in cardiometabolic health in healthy nonobese individuals during caloric restriction-induced weight loss and weight loss maintenance. Am J Physiol Endocrinol Metab. 2018;314(4):E396–405. https://doi.org/10.1152/ajpendo.00261.2017.
Ard JD, Gower B, Hunter G, Ritchie CS, Roth DL, Goss A, et al. Effects of calorie restriction in obese older adults: the CROSSROADS randomized controlled trial. J Gerontol A Biol Sci Med Sci. 2017;73(1):73–80. https://doi.org/10.1093/gerona/glw237.
Verheggen RJ, Maessen MF, Green DJ, Hermus AR, Hopman MT, Thijssen DH. A systematic review and meta-analysis on the effects of exercise training versus hypocaloric diet: distinct effects on body weight and visceral adipose tissue. Obes Rev. 2016;17(8):664–90. https://doi.org/10.1111/obr.12406.
Ruiz JR, Lavie CJ, Ortega FB. Exercise versus pharmacological interventions for reducing visceral adiposity and improving health outcomes. Mayo Clin Proc. 2019;94(2):182–5. https://doi.org/10.1016/j.mayocp.2018.12.018.
Meyer TE, Kovács SJ, Ehsani AA, Klein S, Holloszy JO, Fontana L. Long-term caloric restriction ameliorates the decline in diastolic function in humans. J Am Coll Cardiol. 2006;47(2):398–402. https://doi.org/10.1016/j.jacc.2005.08.069.
Kitzman DW, Brubaker P, Morgan T, Haykowsky M, Hundley G, Kraus WE, et al. Effect of caloric restriction or aerobic exercise training on peak oxygen consumption and quality of life in obese older patients with heart failure with preserved ejection fraction: a randomized clinical trial. JAMA. 2016;315(1):36–46. https://doi.org/10.1001/jama.2015.17346.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no conflicts of interest relevant to this manuscript.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Disclosures
The authors report no financial relationships or conflicts of interest regarding the content herein. No funding sources to declare.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Hypertension and Obesity
Rights and permissions
About this article
Cite this article
Ayinapudi, K., Samson, R., Le Jemtel, T.H. et al. Weight Reduction for Obesity-Induced Heart Failure with Preserved Ejection Fraction. Curr Hypertens Rep 22, 47 (2020). https://doi.org/10.1007/s11906-020-01074-w
Published:
DOI: https://doi.org/10.1007/s11906-020-01074-w