Abstract
Purpose of Review
In this review, we examine the intersection of the HIV and COVID-19 epidemics with focus on COVID-19-related health outcomes and risk factors for SARS-CoV-2 among people living with HIV (PLWH).
Recent Findings
Evidence to date do not suggest a higher incidence of SARS-CoV-2 infection among PLWH compared to the general population, although—once exposed—PLWH are at greater risk of severe COVID-19 outcomes. Key risk factors for severe COVID-19 include non-HIV comorbidities known to be associated with severe disease, as well as HIV-specific risk factors such as low CD4 + T-cell count, unsuppressed viral load, and tuberculosis co-infection. The disproportionate impact of the SARS-CoV-2 pandemic among Black, Latinx, and Native American/Alaskan Native PLWH could worsen pre-existing disparities in health outcomes among PLWH. Data on SARS-CoV-2 vaccine protection among PLWH needs additional study, although some studies suggest decreased humoral responses among those with low CD4 + T-cell counts, while there is a signal of increased vaccine breakthrough rates among PLWH in two large observational cohorts. Data on post-acute sequelae of SARS-CoV-2 (PASC) among PLWH is also limited.
Summary
PLWH do not have a higher susceptibility to SARS-CoV-2, but once exposed, they are at higher risk of severe COVID-19 outcomes. Additional resources will need to be dedicated to the development of interventions to improve health outcomes and address disparities among PLWH impacted by the COVID-19 pandemic.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The SARS-CoV-2 pandemic is the first global pandemic to overlap with the last great pandemic of our era, HIV. Closures for in-person care of medical clinics as part of shelter-in-place ordinances, stock-outs of antiretroviral therapy, and the profound public health impacts of the SARS-CoV-2 pandemic have challenged systems of care for people living with HIV (PLWH) [1, 2]. Adding to fears about setbacks in global HIV epidemic control were concerns about the susceptibility of PLWH to SARS-CoV-2 infection and severe COVID-19 infection, given susceptibility to other pulmonary infections such as pneumococcus even among people with well-controlled HIV [3]. Understanding whether susceptibility to SARS-CoV-2 infection or propensity to develop severe disease is increased among PLWH were crucial questions for both these individuals and their providers. PLWH have generally not been found to have increased incidence rates of respiratory viral infections such as influenza when compared to the general population. However, SARS-CoV-2 transmission is much more widespread than influenza and infection is generally determined by social determinants of health, such as unstable housing [4] and racial/ethnic disparities. [5••] Moreover, comorbidities and behaviors among PLWH—such as higher rates of underlying pulmonary disease [6, 7], inhalational drug use [8], increased tobacco use [9], and hazardous alcohol use [10, 11]—could lead to increased susceptibility to SARS-CoV-2 infection [12]. Finally, PLWH have increased rates of comorbidities which can raise the risk of severe COVID-19 disease if exposed to SARS-CoV-2, including cardiovascular disease [13], pulmonary disease [6, 7], cancer [14], and obesity and diabetes [15].
Given concerns about increased risk of severe SARS-CoV-2 outcomes among PLWH, the extent of protection afforded by COVID-19 vaccines is critical to understand for PLWH and their providers. PLWH have been shown to have reduced humoral responses to natural SARS-CoV-2 infection [16] and might experience less durability of the CoV-2-specific neutralizing antibody (NAb) to a SARS-CoV-2 vaccine [17,18,19,20,21]. As an example in other infections, PLWH experience more rapidly waning NAb titers in response to yellow fever vaccination than those without HIV [18], respond less well to hepatitis B vaccination [22,23,24], and—depending on CD4 count—mount attenuated immune responses to other vaccines [25], including influenza. HIV-specific factors such as CD4 + T-cell count have also been associated with disease outcomes in influenza [12, 26]. Finally, risk factors for post-acute sequelae of SARS-CoV-2 infection (PASC) have been of profound interest among the general population, with emerging data suggesting that vaccination reduces but does not eliminate the risk of PASC or “long COVID” [27]. Given concerns for higher severity COVID-19 [28], higher frequency of autoimmunity and immune dysregulation [29, 30], more medical comorbidities, and a potential for decreased vaccination responses among PLWH, data on longer-term COVID-19 outcomes among PLWH is needed.
We have reached a point in the SARS-CoV-2 pandemic at which large, methodologically rigorous studies are now available to elucidate many of these concerns. In this review, we explore evidence on the susceptibility of PLWH to SARS-CoV-2 infection and the severity of clinical outcomes following infection, as well as emerging evidence on the impact of HIV status on SARS-CoV-2 vaccine responses and risk of PASC.
Susceptibility to SARS-CoV-2 Infection Among PLWH in Population-Level Analyses
Throughout the pandemic, large, population-based studies have mostly demonstrated lower or similar incidence of SARS-CoV-2 infection among PLWH when compared to those without HIV in the general population [28, 31••, 32, 33••, 34,35,36,37,38]. The first reported population-based studies from the early months of the pandemic (through April 2020) generally demonstrated lower SARS-CoV-2 incidence among PLWH. A prospective cohort study among HIV clinics in 60 hospitals that serve 77,590 PLWH in Madrid observed lower age- and sex-standardized risk of infection among PLWH on ART compared to the general population (30 per 10,000 among PLWH vs. 41.7 per 10,000 among the general population), although the risk in the general population attenuated when health care workers were excluded to 33 per 10,000 [31••]. A population-based cohort in Wuhan, China, similarly found lower incidence among PLWH compared to the general population early in the pandemic (0.38%, 95% confidence interval (CI): 0.24–0.53% vs. 0.45%, 95% CI: 0.45–0.46%) [32]. The findings from these early studies may have resulted from greater social distancing among PLWH soon after the pandemic was declared [39].
As the pandemic matured, later population-based studies have generally demonstrated similar SARS-CoV-2 incidence among PLWH and the general population. A population-based study within New York State through June 15, 2020, which included 2988 PLWH who were diagnosed with SARS-CoV-2, demonstrated a similar incidence of infection to the general population after standardization (adjusted rate ratio (ARR) 0.94 (95% CI, 0.91–0.97)) [33••]. US National COVID Cohort Collaborative data, which included 54 sites and 13,170 PLWH, demonstrated lower rates of mild-moderate infection among PLWH compared to those without HIV (adjusted odds ratio (AOR) 0.53 (95% CI: 0.51–0.55)) [34]. In a population-based study from the Western Cape Province, South Africa, which included 540,552 PLWH, the cumulative incidence of SARS-CoV-2 infection through June 9, 2020, was similar by HIV status (0.74% vs. 0.63%) [35]. Cohorts from large health systems have instead been more mixed, with higher incidence of COVID-19 with the University of California, San Diego health system [40], and Kaiser Permanente Southern California [41], but similar incidence within the U.S. Veteran Administration Veterans Aging Cohort [38] and the San Francisco Department of Public Health Clinics [36]. In conclusion, large population-based studies support a generally similar incidence of SARS-CoV-2 among PLWH compared to the general population.
However, PLWH can be disproportionately impacted by social determinants of health that may increase the risk of SARS-CoV-2 infection. Such determinants include greater housing instability than the general population [42, 43], which may decrease the ability to socially distance or effectively quarantine [44, 45]. PLWH are also more likely to be from Black, Latinx, or American Indian/Alaskan Native communities, populations who have had a disproportionate incidence of SARS-CoV-2 compared to White individuals throughout the pandemic [8, 10, 11]. Indeed, communities of color in the USA are subject to systemic racism, which can directly impact their health and health outcomes, including the risk for both COVID-19 and HIV.
Risk of Severe COVID-19 Among PLWH and its Risk Factors
Initial data from earlier in the pandemic did not suggest high rates of severe COVID-19 among PLWH [46,47,48,49,50,51]. However, these data were predominantly from single center studies, hospitalized cohorts, or case series and were susceptible to biases such as the potential for precautionary hospitalization of PLWH independent of clinical status. The largest published population-based cohort to date from the Western Cape Providence, South Africa, included 3978 cases of COVID-19 among 540,552 PLWH out of a cohort of 3,460,932 patients served by the public sector health care system. PLWH had an increased hazard rate for COVID-19 death after adjustment for age and sex when compared to those without HIV (ARR 2.14; 95% CI: 1.70–2.70) [35]. Some aspects of this population were notable, including a low rate of confirmed virologic suppression within the prior 15 months (45%) and high rates of co-occurring tuberculosis and uncontrolled diabetes. However, elevated mortality was similarly demonstrated in the OpenSAFELY platform from the UK primary care clinic system, which included 27,480 PLWH within a population of 17,282,905 individuals. After adjusting for age and sex, PLWH had a higher risk of COVID-19 death (AHR 2.59 (95% CI 1.74–3.84)) [52] than those without HIV. In the US National COVID Cohort Collaborative, which included 13,170 cases of COVID-19 among PLWH, there were an increased adjusted odds of mortality (AOR 1.29 (95% CI 1.16–1.44)) [34] among PLWH. Similarly—among 2988 PLWH diagnosed with COVID-19 in New York State—the mortality rate was higher compared to those without HIV (standardized RR, 1.23 (95% CI, 1.07–1.40)) [33••]. Within the WHO Global Clinical Platform, which included hospitalization data on 15,522 PLWH from 24 countries—although most data came from South Africa—the adjusted rate of severe or fatal COVID-19 was 1.30-fold higher among PLWH (95% CI: 1.24–1.36) [53••] than those without HIV.
Several HIV-specific risk factors among PLWH have been identified for severe COVID-19, in addition to traditional risk factors such as older age, diabetes, obesity, and cardiovascular disease [17, 35, 53••]. PLWH with CD4 + T-cell counts < 200 cells/mm3 had elevated mortality risk in the US National COVID Cohort Collaborative (AOR 2.73; 95% CI 1.80–4.14 vs. > 500) [34], within the US TriNetX database [54], as well as in the Western Cape Province, South Africa (AHR 2.36; 95% CI: 1.47–3.78) [17] analysis. A similar risk profile for PLWH with lower CD4 counts was seen inn a multi-center registry of PLWH in the USA which included 286 hospitalized PLWH [55], in the University of Colorado Health System among 206 PLWH with COVID-19 [56], and in a health system cohort in San Francisco among 136 PLWH with COVID-19 [36]. Having a CD4 + T-cell count nadir < 200 cells/mm3 was additionally associated with hospitalization in a multi-center cohort of PLWH in the USA which included 649 cases of COVID-19 (ARR 1.67; 95% CI 1.18–2.36) [57••]. In this cohort, a current CD4 + count < 350 cells/mm3 was also associated with hospitalization (ARR 2.68; 95% CI 1.93–3.71). The data on virologic suppression are more limited and mixed, with the US National COVID Cohort Collaborative demonstrating an increased risk of hospitalization, but not death [34] in those without virologic suppression, although viremia was significantly associated with disease severity within the multi-center cohort of PLWH in the USA [57••]. Tuberculosis co-infection was additionally associated with mortality in the Western Cape Province Cohort (AHR 2.70; 95% CI, 1.81–4.04).
In addition to medical comorbidities already discussed, it is important to note the SARS-CoV-2 pandemic has disproportionately impacted Black and Latinx communities, as well as Alaska Natives/American Indians, and those living in higher poverty neighborhoods, communities that have already been affected significantly by the HIV epidemic. Among the 2410 PLWH who were diagnosed with COVID-19 in the New York City registry, those who were Black or Latinx, and/or came from high poverty neighborhoods had greater rates of severe COVID-19 [5••]. These findings were echoed among analyses completed in Philadelphia and Boston, with a higher concentration of poor COVID-19 outcomes among Black PLWH and those living in neighborhoods with higher poverty [8, 10]. Similar findings were noted in the UK, where there was evidence of disproportionate risk of severe COVID-19 among Black PLWH compared to non-Black PLWH (AHR 4.31 [95% CI 2.42–7.65]) vs non-Black people without HIV (HR 1.84 [95% CI 1.03–3.26] p-interaction = 0.044) [52]. In Paris, similar disparities were noted by Black vs. White race [58] among PLWH. There is the worrying potential for the COVID-19 pandemic to worsen health inequities among PLWH via multiple mechanisms, including COVID-19 disease outcomes, impacts on HIV disease control, and the psychosocial and economic impacts of the pandemic [5••, 28].
Protection from SARS-CoV-2 Vaccination
Data on the impact of SARS-CoV-2 vaccination on COVID-19 outcomes among PLWH is limited. When the subgroup of PLWH (n = 240) was excluded from the analysis of the Novavax phase 2b trial in South Africa, the investigators reported that efficacy rose from 49.4 to 60%. This has raised concern that the efficacy of this particular vaccine was lower in PLWH [59]. Trials for the mRNA vaccines did include small numbers of PLWH (196 and 176) although HIV specific data was not reported in the outcome papers [60]. The Janssen/Johnson and Johnson vaccine study involved the largest number of PLWH so far (1218), and, per news reports, 2 PLWH who received the vaccine experienced COVID-19 versus 4 PLWH in the placebo group [60]. However, given these small numbers, definitive inferences cannot be drawn. A recent study of ART-suppressed PLWH who received the BNT162b2 vaccine showed lower neutralizing responses compared to healthcare workers, but the cohort did not represent the full spectrum of HIV disease, follow-up was limited to 18 days, and no T cell assays or mechanistic studies were performed [61]. Although a cohort of PLWH receiving the ChAdOx1 vaccine did not find differences in humoral and ELISPOT and T-cell responses compared to healthy controls over 6 months of follow-up, the cohort was relatively young and healthy, and excluded individuals with CD4 + T-cell counts < 350 cells/µL or virologic non-suppression [62, 63]. A cohort of 100 PLWH matched on age, sex, which mRNA vaccine they received, and time since vaccination demonstrated greater surrogate virus neutralization test non-response among PLWH, with greater non-response among those with CD4 + T-cell count < 200 cells/µL and unsuppressed viral loads [64]. Within a cohort of 166 PLWH who received an mRNA-based vaccine, those with CD4 + T-cell counts < 200 cells/µL had reduced humoral and T-cell immunity compared to those with CD4 + T-cell counts > 500 cells/µL [65]. PLWH who received the Novavax vaccine had attenuated humoral immune responses [66] as did those who received CoronaVac [67]. A cohort 136 PLWH who received mRNA vaccination demonstrated comparable humoral and cellular responses, although those with CD4 + T-cell counts < 300 cells/µL had lower binding antibodies [68]. The question of whether additional booster vaccination attenuates potential differences in immune responses among PLWH with lower CD4 + counts and unsuppressed viral loads merits further study.
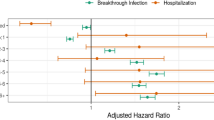
Given evidence of reduced humoral responses to vaccination among PLWH in some studies, particularly in those with low CD4 + counts or virologic non-suppression, clinical data on outcomes following vaccination and boosting among PLWH is needed. In a cohort of adults who had one or two doses of COVID-19 vaccination in the UK, PLWH had an increased adjusted hazard ratio for death following vaccination (AHR 3.29; 95% CI: 1.05–10.29) [69]. Among 31,840 PLWH in the USA and 77,759 people without HIV who had completed SARS-CoV-2 vaccination prior to booster immunization, the rate of breakthrough infection was higher among PLWH (44 vs. 31 per 1000 person-years; AHR = 1.41 95% CI: 1.28, 1.56) [70]. The third shot or booster is definitively indicated for PLWH and data on additional booster doses is needed.
Data on responses to other preventative and treatment strategies such as monoclonal antibodies and antivirals among PLWH remains even more limited. Case reports among immunocompromised hosts, including among PLWH, have discussed long durations of persistence of viral antigen and culturable virus in the context of persistent or recurrent symptoms, with antiviral treatment courses repeated [71,72,73]. Additional research will need to explore the relationship between immunocompromise and antiviral resistance [73], need for antiviral retreatment [71], and potential for drug interactions with other essential therapies [74].
Risk of PASC Among PLWH
The limited data available to date suggest that medical comorbidities, severity of prior COVID-19 infection, and being unvaccinated against SARS-CoV-2 are the major risk factors for PASC [27, 75,76,77,78]. PASC may also be driven, at least in part, by residual inflammation following prior SARS-CoV-2 infection [79]. HIV infection, including in the setting of effective antiretroviral therapy, is characterized by chronic immune activation and tissue inflammation [80, 81]. PLWH could therefore be at elevated risk of PASC due to greater risk of severe COVID-19 [53••], potential for diminished SARS-CoV-2 vaccine responses [64], greater comorbidity burden [6, 7, 13], or greater baseline systemic inflammation and immune dysregulation [29, 30]. To date, the data available on risk factors for PASC among PLWH are limited, with the pathogenesis and potential treatments poorly understood.
However, a few studies investigating the impact of HIV status on risk for PASC have been published to date [82,83,84]. A retrospective survey study of people who presented to the emergency department with SARS-CoV-2 through May 15, 2020, found that PLWH, when adjusting for demographics, comorbidities, and severity of illness, had 1.75-fold higher odds of PASC symptoms at least nine months out from diagnosis (95% CI: 1.14–2.69) [82]. A case–control study which included 39 PLWH enrolled after prior SARS-CoV-2 infection in the pre-vaccine era found 4.01-fold higher odds of PASC among PLWH when adjusting for age, time since infection, and disease severity (95% CI: 1.45–11.1) [84]. PLWH had lower levels of anti-SARS-CoV-2 CD8 + T-cells and greater anti-SARS-CoV-2 CD4 + T-cell exhaustion. There was a trend towards increased CD4 + T-cell immune exhaustion with PASC irrespective of HIV status. Finally, a cohort of 94 PLWH with well-controlled HIV on ART in Western India found that 43.6% of the cohort met criteria for PASC, with individuals with lower CD4 + T-cell counts having higher rates of PASC.
Additional research is urgently needed, as PLWH may be more likely to exhibit risk factors for PASC (including greater baseline inflammation, comorbidities, and susceptibility to severe COVID-19). Given the strong association between COVID-19 disease severity and risk of PASC, alongside the higher risk of severe COVID-19 among PLWH, PLWH should continue to be prioritized for COVID-19 prevention and treatment including vaccination and antivirals.
Conclusions
This review summarizes available data on the relationship between HIV status and susceptibility to SARS-CoV-2 infection, risk of severe COVID-19, response to vaccination, and rates of PASC. Large population-based studies have generally demonstrated similar incidence of SARS-CoV-2 infection among PLWH, but greater risk of severe COVID-19 once exposed to the virus. Key risk factors among PLWH include low CD4 + T-cell count, unsuppressed viral load, and tuberculosis co-infection, as well as traditional COVID-19 risk factors such as cardiopulmonary disease, diabetes, and obesity. The disproportionate impact of the COVID-19 pandemic on Black, Latinx, and Alaskan Native/American Indian PLWH has the potential to worsen pre-existing disparities in health outcomes and should be urgently addressed through public health and financial investment directed towards reducing inequities engendered by structural racism [85]. Data on vaccine responses among PLWH remains limited, with some studies demonstrating evidence of decreased humoral responses among those with lower CD4 + T-cell counts, and a potential for increased vaccine breakthrough following initial series vaccination. Further data on vaccine responses following additional doses of the vaccine among PLWH with lower CD4 + T-cell counts are needed. Data on antiviral treatment response and risk of PASC among PLWH is extremely limited, and high-quality studies will be needed given the importance of these topics to PLWH and their providers. The ongoing collision of the HIV epidemic and the SARS-CoV-2 pandemic will require additional study, as well as development of interventions to attenuate impacts of the SARS-CoV-2/HIV syndemic on the health of PLWH globally.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Lamontagne E. COVID-19 pandemic increases socioeconomic vulnerability of LGBTI+ communities and their susceptibility to HIV. AIDS 2020 San Francisco/Oakland 2020. July 14. abstract LBPEE53.
Centers for Disease Control and Prevention. HIV Surveillance Report, 2020; vol. 33. https://www.cdc.gov/hiv/library/reports/hiv-surveillance.html. Published May 2022. Accessed June 2 2022.
Garcia Garrido HM, Mak AMR, Wit F, et al. Incidence and risk factors for invasive pneumococcal disease and community-acquired pneumonia in human immunodeficiency virus-infected individuals in a high-income setting. Clin Infect Dis. 2020;71(1):41–50.
Sachdev D, Mara E, Hsu L, et al. COVID-19 Susceptibility and outcomes among people living with HIV in San Francisco. J Acquir Immune Defic Syndr. 2020;86(1):19–21.
•• Braunstein SL, Lazar R, Wahnich A, Daskalakis DC, Blackstock OJ. Coronavirus disease 2019 (COVID-19) infection among people with human immunodeficiency virus in New York City: a population-level analysis of linked surveillance data. Clin Infect Dis. 2020;72(12):e1021–9. Braunstein and colleagues present a methodolocially rigorous examination of the impact of HIV status on COVID-19 outcomes among PLWH in New York City. This study also demonstrated the impact of racial/ethnic and socioeconomic disparities on COVID-19 outcomes.
Fitzpatrick ME, Kunisaki KM, Morris A. Pulmonary disease in HIV-infected adults in the era of antiretroviral therapy. AIDS. 2018;32(3):277–92.
Crothers K. Chronic obstructive pulmonary disease in patients who have HIV infection. Clin Chest Med. 2007;28(3):575–87, vi.
Meyerowitz EA, Kim AY, Ard KL, et al. Disproportionate burden of coronavirus disease 2019 among racial minorities and those in congregate settings among a large cohort of people with HIV. AIDS 2020; 34(12).
Mdodo R, Frazier EL, Dube SR, et al. Cigarette smoking prevalence among adults with HIV compared with the general adult population in the United States: cross-sectional surveys. Ann Intern Med. 2015;162(5):335–44.
Goldstein ND, Webster JL, Robinson LF, Welles SL. Disparities of COVID-19 and HIV occurrence based on neighborhood infection incidence in Philadelphia, Pennsylvania. Am J Public Health. 2022;112(3):408–16.
Zlot AI, Capizzi J, Bush L, Menza TW. Impact of COVID-19 Among immigrant and communities of color living with HIV in Oregon, 2020: two pandemics rooted in racism. J Immigr Minor Health. 2021;23(6):1348–53.
Sheth AN, Althoff KN, Brooks JT. Influenza susceptibility, severity, and shedding in HIV-infected adults: a review of the literature. Clin Infect Dis. 2011;52(2):219–27.
Triant VA. Cardiovascular disease and HIV infection. Curr HIV/AIDS Rep. 2013;10(3):199–206.
Silverberg MJ, Leyden W, Hernández-Ramírez RU, et al. Timing of antiretroviral therapy initiation and risk of cancer among persons living with human immunodeficiency virus. Clin Infect Dis. 2021;72(11):1900–9.
Hernandez-Romieu AC, Garg S, Rosenberg ES, Thompson-Paul AM, Skarbinski J. Is diabetes prevalence higher among HIV-infected individuals compared with the general population? Evidence from MMP and NHANES 2009–2010. BMJ Open Diabetes Res Care. 2017;5(1):e000304.
Spinelli MA, Lynch KL, Yun C, et al. SARS-CoV-2 seroprevalence, and IgG concentration and pseudovirus neutralising antibody titres after infection, compared by HIV status: a matched case-control observational study. The Lancet HIV. 2021;8(6):e334–41.
Buechler MB, Newman LP, Chohan BH, Njoroge A, Wamalwa D, Farquhar C. T cell anergy and activation are associated with suboptimal humoral responses to measles revaccination in HIV-infected children on anti-retroviral therapy in Nairobi. Kenya Clin Exp Immunol. 2015;181(3):451–6.
Avelino-Silva VI, Miyaji KT, Hunt PW, et al. CD4/CD8 ratio and KT ratio predict yellow fever vaccine immunogenicity in HIV-infected patients. PLoS Negl Trop Dis. 2016;10(12):e0005219.
Colin de Verdiere N, Durier C, Samri A, et al. Immunogenicity and safety of yellow fever vaccine in HIV-1-infected patients. AIDS. 2018;32(16):2291–9.
Parmigiani A, Alcaide ML, Freguja R, et al. Impaired antibody response to influenza vaccine in HIV-infected and uninfected aging women is associated with immune activation and inflammation. PLoS One. 2013;8(11):e79816.
Spinelli MA. SARS-CoV-2 vaccination in people with HIV. The Lancet HIV 2021. Epub ahead of print https://doi.org/10.1016/S2352-3018(21)00128-4.
van den Berg R, van Hoogstraten I, van Agtmael M. Non-responsiveness to hepatitis B vaccination in HIV seropositive patients; possible causes and solutions. AIDS Rev. 2009;11(3):157–64.
Collier AC, Corey L, Murphy VL, Handsfield HH. Antibody to human immunodeficiency virus (HIV) and suboptimal response to hepatitis B vaccination. Ann Intern Med. 1988;109(2):101–5.
Pasricha N, Datta U, Chawla Y, et al. Immune responses in patients with HIV infection after vaccination with recombinant Hepatitis B virus vaccine. BMC Infect Dis. 2006;6:65.
Kroon FP, van Dissel JT, Labadie J, van Loon AM, van Furth R. Antibody response to diphtheria, tetanus, and poliomyelitis vaccines in relation to the number of CD4+ T lymphocytes in adults infected with human immunodeficiency virus. Clin Infect Dis. 1995;21(5):1197–203.
von Mollendorf C, Hellferscee O, Valley-Omar Z, et al. Influenza viral shedding in a prospective cohort of HIV-infected and uninfected children and adults in 2 provinces of South Africa, 2012–2014. J Infect Dis. 2018;218(8):1228–37.
Antonelli M, Penfold RS, Merino J, et al. Risk factors and disease profile of post-vaccination SARS-CoV-2 infection in UK users of the COVID Symptom Study app: a prospective, community-based, nested, case-control study. Lancet Infect Dis. 2022;22(1):43–55.
Brown LB, Spinelli MA, Gandhi M. The interplay between HIV and COVID-19: summary of the data and responses to date. Curr Opin HIV AIDS. 2021;16(1):63–73.
Rutishauser RL, Hartogensis W, Deguit CD, et al. Early and delayed antiretroviral therapy results in comparable reductions in CD8(+) T cell exhaustion marker expression. AIDS Res Hum Retroviruses. 2017;33(7):658–67.
Fromentin R, Bakeman W, Lawani MB, et al. CD4+ T cells expressing PD-1, TIGIT and LAG-3 contribute to HIV persistence during ART. PLoS Pathog. 2016;12(7):e1005761.
•• Del Amo J, Polo R, Moreno S, et al. Incidence and severity of COVID-19 in HIV-positive persons receiving antiretroviral therapy: a cohort study. Ann Intern Med 2022. This prospective cohort study among HIV clinics in 60 hospitals that serve over 75,000 PLWH in Madrid observed lower risk of SARS-CoV-2 infection among PLWH on ART compared to the general population, although the risk was similar between PLWH and the general population once health care workers were excluded.
Huang J, Xie N, Hu X, et al. Epidemiological, virological and serological features of COVID-19 cases in people living with HIV in Wuhan City: a population-based cohort study. Clin Infect Dis. 2020;73(7):e2086–e2094.
•• Tesoriero JM, Swain CE, Pierce JL, et al. COVID-19 outcomes among persons living with or without diagnosed hiv infection in New York state. JAMA Netw Open. 2021;4(2):e2037069. This study by Tesoriero and colleagues demonstrates the impact of living with HIV on COVID-19 outcomes in a large population-based sample among PLWH in New York State.
Yang X, Sun J, Patel RC, et al. Associations between HIV infection and clinical spectrum of COVID-19: a population level analysis based on US National COVID Cohort Collaborative (N3C) data. Lancet HIV. 2021;8(11):e690–700.
Boulle A, Davies MA, Hussey H, et al. Risk factors for COVID-19 death in a population cohort study from the Western Cape Province, South Africa. Clin Infect Dis. 2021;73(7):e2005–e2015.
Spinelli MA, Brown LB, Glidden DV, et al. SARS-CoV-2 incidence, testing rates, and severe COVID-19 outcomes among people with and without HIV. AIDS. 2021;35(15):2545–7.
Charre C, Icard V, Pradat P, et al. Coronavirus disease 2019 attack rate in HIV-infected patients and in preexposure prophylaxis users. AIDS. 2020;34(12):1765–70.
Park LR, CT Rentsch, Sigel K, Rodriguez-Barradas M, Brown ST, Goetz MB, Williams EC, Althoff K, Brau N, Aoun-Barakat L, Tseng A, Justice AC, Tate JP. COVID-19 in the largest US HIV cohort. In: AIDS 2020: 23rd International AIDS Conference Virtual, 2020.
Santiago-Rodriguez EI, Maiorana A, Peluso MJ, et al. Characterizing the COVID-19 illness experience to inform the study of post-acute sequelae and recovery. Int J Behav Med 2021: 1–14.
Tang ME, Gaufin T, Anson R, Zhu W, Mathews William C, Cachay ER. People with HIV have a higher risk of COVID-19 diagnosis but similar outcomes to the general population. HIV Medicine.
Chang JJ, Bruxvoort K, Chen LH, Akhavan B, Rodriguez J, Hechter RC. Brief report: COVID-19 testing, characteristics, and outcomes among people living with HIV in an integrated health system. JAIDS Journal of Acquired Immune Deficiency Syndromes 2021; 88(1).
Fazel S, Geddes JR, Kushel M. The health of homeless people in high-income countries: descriptive epidemiology, health consequences, and clinical and policy recommendations. Lancet. 2014;384(9953):1529–40.
Aidala AA, Lee G, Abramson DM, Messeri P, Siegler A. Housing need, housing assistance, and connection to HIV medical care. AIDS Behav. 2007;11(6 Suppl):101–15.
Mosites E, Parker EM, Clarke KEN, et al. Assessment of SARS-CoV-2 infection prevalence in homeless shelters - four U.S. Cities, March 27-April 15, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(17):521–2.
Imbert E, Kinley PM, Scarborough A, et al. Coronavirus disease 2019 (COVID-19) outbreak in a San Francisco homeless shelter. Clin Infect Dis 2020.
Blanco JL, Ambrosioni J, Garcia F, et al. COVID-19 in patients with HIV: clinical case series. Lancet HIV. 2020;7(5):e314–6.
Vizcarra P, Pérez-Elías MJ, Quereda C, et al. Description of COVID-19 in HIV-infected individuals: a single-centre, prospective cohort. Lancet HIV. 2020;7(8):e554–64.
Karmen-Tuohy S, Carlucci PM, Zervou FN, et al. Outcomes among HIV-positive patients hospitalized with COVID-19. J Acquir Immune Defic Syndr. 2020;85(1):6–10.
Childs K, Post FA, Norcross C, et al. Hospitalized patients with COVID-19 and HIV: a case series. Clin Infect Dis. 2020;71(8):2021–2.
Collins LF, Moran CA, Oliver NT, et al. Clinical characteristics, comorbidities and outcomes among persons with HIV hospitalized with coronavirus disease 2019 in Atlanta, GA. Aids. 2020;34(12):1789–94.
Meyerowitz EA, Kim AY, Ard KL, et al. Disproportionate burden of COVID-19 among racial minorities and those in congregate settings among a large cohort of people with HIV. Aids. 2020;34(12):1781–7.
Bhaskaran K, Rentsch CT, MacKenna B, et al. HIV infection and COVID-19 death: a population-based cohort analysis of UK primary care data and linked national death registrations within the OpenSAFELY platform. Lancet HIV. 2021;8(1):e24–32.
•• Bertagnolio S, Thwin SS, Silva R, et al. Clinical characteristics and prognostic factors in people living with HIV hospitalized with COVID-19: findings from the WHO Global Clinical Platform. IAS 2021; July 19, 2021. Abstract 2498. The WHO Global Clinical Platform presents data on the impact of HIV status on COVID-19 outcomes in a large, multi-country sample based on hospitalization data.
Yendewa GA, Perez JA, Schlick K, Tribout H, McComsey GA. Clinical features and outcomes of coronavirus disease 2019 among people with human immunodeficiency virus in the United States: a multicenter study from a large global health research network (TriNetX). Open Forum Infect Dis. 2021;8(7):ofab272.
Dandachi D, Geiger G, Montgomery MW, et al. Characteristics, comorbidities, and outcomes in a multicenter registry of patients with HIV and coronavirus disease-19. Clin Infect Dis. 2020;73(7):e1964–72
Kamis KF, Barbera L, Abdo M, et al. Risk Factors for hospitalization in people with HIV and COVID-19. JAIDS J Acquire Immune Defic Syndr. 2021;88(3):e22.
•• Shapiro AE, Bender Ignacio RA, Whitney BM, et al. Factors associated with severity of COVID-19 disease in a multicenter cohort of people with HIV in the United States, March-December 2020. J Acquir Immune Defic Syndr. 2022;90(4):369–76. This multi-site U.S. cohort identified novel risk factors for severe COVID-19 including CD4+ T-cell count nadir, which has important implications for prioritization of therapeutics.
Etienne N, Karmochkine M, Slama L, et al. HIV infection and COVID-19: risk factors for severe disease. AIDS. 2020;34(12):1771–4.
Callaway E, Mallapty S. Novavax offers first evidence that COVID vaccines protect people against variants. 2021 Nature News. Available at https://www.nature.com/articles/d41586-021-00268-9. Accessed 2/1/21.
Peabody R. Have COVID-19 vaccines been tested in people with HIV? NAM AIDSMAP 2021. Accessed Februrary 25. Available at: https://www.aidsmap.com/about-hiv/have-covid-19-vaccines-been-tested-people-hiv.
Levy I, Wieder – Finesod A, Litchevsky V, et al. Immunogenicity and safety of the BNT162b2 mRNA COVID-19 vaccine in people living with HIV-1. Clini Microbiol Infect. 2021;27(12):1851–5.
Frater J, Ewer KJ, Ogbe A, et al. Safety and immunogenicity of the ChAdOx1 nCoV-19 (AZD1222) vaccine against SARS-CoV-2 in HIV infection: a single-arm substudy of a phase 2/3 clinical trial. Lancet HIV. 2021;8(8):e474–85.
Ogbe A, Pace M, Bittaye M, et al. Durability of ChAdOx1 nCoV-19 vaccination in people living with HIV. JCI Insight. 2022;7(7):e157031.
Spinelli MA, Peluso MJ, Lynch KL, et al. Differences in post-mRNA vaccination SARS-CoV-2 IgG concentrations and surrogate virus neutralization test response by HIV status and type of vaccine: a matched case-control observational study. Clin Infect Dis. 2021. pp. ciab1009.
Antinori A, Cicalini S, Meschi S, et al. Humoral and cellular immune response elicited by mRNA vaccination against SARS-CoV-2 in people living with HIV (PLWH) receiving antiretroviral therapy (ART) according with current CD4 T-lymphocyte count. Clin Infect Dis. 2022. pp. ciac238.
Madhi SA, Moodley D, Hanley S, et al. Immunogenicity and safety of a SARS-CoV-2 recombinant spike protein nanoparticle vaccine in people living with and without HIV-1 infection: a randomised, controlled, phase 2A/2B trial. Lancet HIV. 2022;9(5):e309–22.
Netto LC, Ibrahim KY, Picone CM, et al. Safety and immunogenicity of CoronaVac in people living with HIV: a prospective cohort study. Lancet HIV. 2022;9(5):e323–31.
Tau L, Turner D, Adler A, et al. SARS-CoV-2 Humoral and cellular immune responses of patients with HIV After vaccination with BNT162b2 mRNA COVID-19 vaccine in the Tel-Aviv Medical Center. Open Forum Infect Dis. 2022;9(4):ofac089.
Hippisley-Cox J, Coupland CA, Mehta N, et al. Risk prediction of covid-19 related death and hospital admission in adults after COVID-19 vaccination: national prospective cohort study. BMJ. 2021;374:n2244.
Coburn SB, Humes E, Lang R, et al. COVID-19 infections post-vaccination by HIV status in the United States. medRxiv 2021: 2021.12.02.21267182.
Sepulcri C, Dentone C, Mikulska M, et al. The longest persistence of viable SARS-CoV-2 with recurrence of viremia and relapsing symptomatic COVID-19 in an immunocompromised patient-a case study. Open Forum Infect Dis. 2021;8(11):ofab217.
Hensley MK, Bain WG, Jacobs J, et al. Intractable coronavirus disease 2019 (COVID-19) and prolonged severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) replication in a chimeric antigen receptor-modified T-cell therapy recipient: a case study. Clin Infect Dis. 2021;73(3):e815–21.
Cele S, Karim F, Lustig G, et al. SARS-CoV-2 prolonged infection during advanced HIV disease evolves extensive immune escape. Cell Host Microbe. 2022;30(2):154-62.e5.
Rose DT, Gandhi SM, Bedard RA, et al. Supratherapeutic tacrolimus concentrations with nirmatrelvir/ritonavir in solid organ transplant recipients requiring hospitalization: a case series using rifampin for reversal. Open Forum Infect Dis. 2022;9(7):ofac238.
Bergwerk M, Gonen T, Lustig Y, et al. Covid-19 Breakthrough infections in vaccinated health care workers. N Engl J Med. 2021;385(16):1474–84.
Kuodi P, Gorelik Y, Zayyad H, et al. Association between vaccination status and reported incidence of post-acute COVID-19 symptoms in Israel: a cross-sectional study of patients tested between March 2020 and November 2021. medRxiv 2022: 2022.01.05.22268800.
Taquet M, Dercon Q, Harrison PJ. Six-month sequelae of post-vaccination SARS-CoV-2 infection: a retrospective cohort study of 10,024 breakthrough infections. Brain Behav Immun. 2022;103:154–62.
Al-Aly Z, Bowe B, Xie Y. Long COVID after breakthrough SARS-CoV-2 infection. Nat Med. 2022;28(7):1461–7.
Phetsouphanh C, Darley DR, Wilson DB, et al. Immunological dysfunction persists for 8 months following initial mild-to-moderate SARS-CoV-2 infection. Nat Immunol. 2022;23(2):210–6.
Serrano-Villar S, Sainz T, Lee SA, et al. HIV-infected individuals with low CD4/CD8 ratio despite effective antiretroviral therapy exhibit altered T cell subsets, heightened CD8+ T cell activation, and increased risk of non-AIDS morbidity and mortality. PLoS Pathog. 2014;10(5):e1004078.
Khoury G, Fromentin R, Solomon A, et al. Human immunodeficiency virus persistence and T-cell activation in blood, rectal, and lymph node tissue in human immunodeficiency virus-infected individuals receiving suppressive antiretroviral therapy. J Infect Dis. 2017;215(6):911–9.
Kingery JR, Safford MM, Martin P, et al. Health status, persistent symptoms, and effort intolerance one year after acute COVID-19 infection. J Gen Intern Med. 2022;37(5):1218–25.
Pujari S, Gaikwad S, Chitalikar A, Dabhade D, Joshi K, Bele V. Long-coronavirus disease among people living with HIV in western India: an observational study. Immun Inflamm Dis. 2021;9(3):1037–43.
Peluso MJ, Spinelli MA, Deveau T-M, et al. Post-acute sequelae and adaptive immune responses in people living with HIV recovering from SARS-CoV-2 infection. medRxiv 2022: 2022.02.10.22270471.
Millett GA. New pathogen, same disparities: why COVID-19 and HIV remain prevalent in U.S. communities of colour and implications for ending the HIV epidemic. J Int AIDS Soc. 2020;23(11):e25639.
Funding
This work was funded by National Institutes of Health/National Institute of Allergy and Infectious Diseases R01AI158013 and R21AI138771 (MPI Spinelli and Gandhi).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Human and Animal Rights and Informed Consent
All reported studies/experiments with human or animal subjects performed by the authors have been previously published and complied with all applicable ethical standards (including the Helsinki Declaration and its amendments, institutional/national research committee standards, and international/national/institutional guidelines).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Complications of HIV and Antiretroviral Therapy.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Spinelli, M.A., Jones, B.L.H. & Gandhi, M. COVID-19 Outcomes and Risk Factors Among People Living with HIV. Curr HIV/AIDS Rep 19, 425–432 (2022). https://doi.org/10.1007/s11904-022-00618-w
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11904-022-00618-w