Abstract
Purpose of Review
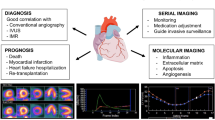
Cardiac allograft vasculopathy (CAV) is a late-occurring complication of heart transplantation significantly limiting overall graft survival. In the last few years, evidence has been growing about the use of positron emission tomography (PET) myocardial perfusion imaging with integrated myocardial blood flow (MBF) quantification in heart transplant recipients.
Recent Findings
Multiple studies have demonstrated that PET MBF assessment can be utilized to establish the diagnosis of CAV noninvasively and can be employed for prognostication. PET MBF quantification has also helped to define the link between transplant rejection and CAV. In addition, limited data suggests that PET MBF quantification can be used in heart transplant patients for serial monitoring of CAV.
Summary
PET myocardial perfusion imaging integrating MBF quantification shows great promise for the evaluation of CAV with good diagnostic and prognostic performance.



Similar content being viewed by others
Abbreviations
- CAV:
-
Cardiac allograft vasculopathy
- IVUS:
-
Intravascular ultrasound
- PET:
-
Positron emission tomography
- MBF:
-
Myocardial blood flow
- ISHLT:
-
International Society of Heart and Lung Transplantation
- MFR:
-
Myocardial flow reserve
- MACE:
-
Major adverse cardiovascular events
- IMR:
-
Index of microcirculatory resistance
- CTAC:
-
Computed tomography attenuation correction
- MPI:
-
Myocardial perfusion imaging
References
Papers of particular interest, published recently, have been highlighted as: •• Of major importance
Lund LH, Edwards LB, Kucheryavaya AY, et al. The Registry of the International Society for Heart and Lung Transplantation: thirty-second official adult heart transplantation report–2015; focus theme: early graft failure. J Heart Lung Transplant. 2015;34(10):1244–54.
Hiemann NE, Wellnhofer E, Knosalla C, et al. Prognostic impact of microvasculopathy on survival after heart transplantation: evidence from 9713 endomyocardial biopsies. Circulation. 2007;116(11):1274–82.
Pober JS, Jane-Wit D, Qin L, Tellides G. Interacting mechanisms in the pathogenesis of cardiac allograft vasculopathy. Arterioscler Thromb Vasc Biol. 2014;34(8):1609–14.
Mehra MR, Crespo-Leiro MG, Dipchand A, et al. International Society for Heart and Lung Transplantation working formulation of a standardized nomenclature for cardiac allograft vasculopathy-2010. J Heart Lung Transplant. 2010;29(7):717–27.
St Goar FG, Pinto FJ, Alderman EL, et al. Intracoronary ultrasound in cardiac transplant recipients. In vivo evidence of “angiographically silent” intimal thickening. Circulation. 1992;85(3):979–87.
Hou J, Lv H, Jia H, et al. OCT assessment of allograft vasculopathy in heart transplant recipients. JACC Cardiovasc Imaging. 2012;5(6):662–3.
Lee JH, Okada K, Khush K, et al. Coronary endothelial dysfunction and the index of microcirculatory resistance as a marker of subsequent development of cardiac allograft vasculopathy. Circulation. 2017;135(11):1093–5.
Chirakarnjanakorn S, Starling RC, Popovic ZB, Griffin BP, Desai MY. Dobutamine stress echocardiography during follow-up surveillance in heart transplant patients: diagnostic accuracy and predictors of outcomes. J Heart Lung Transplant. 2015;34(5):710–7.
Elkaryoni A, Abu-Sheasha G, Altibi AM, Hassan A, Ellakany K, Nanda NC. Diagnostic accuracy of dobutamine stress echocardiography in the detection of cardiac allograft vasculopathy in heart transplant recipients: a systematic review and meta-analysis study. Echocardiography. 2019;36(3):528–36.
Feher A, Sinusas AJ. Quantitative assessment of coronary microvascular function: dynamic single-photon emission computed tomography, positron emission tomography, ultrasound, computed tomography, and magnetic resonance imaging. Circ Cardiovasc Imaging. 2017;10(8).
Czernin J, Muller P, Chan S, et al. Influence of age and hemodynamics on myocardial blood flow and flow reserve. Circulation. 1993;88(1):62–9.
Konerman MC, Lazarus JJ, Weinberg RL, et al. Reduced myocardial flow reserve by positron emission tomography predicts cardiovascular events after cardiac transplantation. Circ Heart Fail. 2018;11(6):e004473.
Miller RJH, Manabe O, Tamarappoo B, et al. Comparative prognostic and diagnostic value of myocardial blood flow and myocardial flow reserve after cardiac transplantation. J Nucl Med. 2020;61(2):249–55.
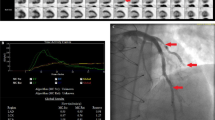
•• Chih S, Chong AY, Erthal F, et al. PET assessment of epicardial intimal disease and microvascular dysfunction in cardiac allograft vasculopathy. J Am Coll Cardiol. 2018;71(13):1444–56. This study assessed the diagnostic performance of PET myocardial blood flow quantification against IVUS and invasive microvascular assessment.
•• Bravo PE, Bergmark BA, Vita T, et al. Diagnostic and prognostic value of myocardial blood flow quantification as non-invasive indicator of cardiac allograft vasculopathy. Eur Heart J. 2018;39(4):316–23. This study assessed the diagnostic and prognostic value of an integrated PET allograft vasculopathy grading system which was based on myocardial perfusion, resting ejection fraction, and myocardial blood flow quantification.
Kofoed KF, Czernin J, Johnson J, et al. Effects of cardiac allograft vasculopathy on myocardial blood flow, vasodilatory capacity, and coronary vasomotion. Circulation. 1997;95(3):600–6.
Wu YW, Chen YH, Wang SS, et al. PET assessment of myocardial perfusion reserve inversely correlates with intravascular ultrasound findings in angiographically normal cardiac transplant recipients. J Nucl Med. 2010;51(6):906–12.
Allen-Auerbach M, Schoder H, Johnson J, et al. Relationship between coronary function by positron emission tomography and temporal changes in morphology by intravascular ultrasound (IVUS) in transplant recipients. J Heart Lung Transplant. 1999;18(3):211–9.
Ahn JM, Zimmermann FM, Arora S, et al. Prognostic value of comprehensive intracoronary physiology assessment early after heart transplantation. Eur Heart J. 2021;42(48):4918–29.
Gunther A, Andersen R, Gude E, et al. The predictive value of coronary artery calcium detected by computed tomography in a prospective study on cardiac allograft vasculopathy in heart transplant patients. Transpl Int. 2018;31(1):82–91.
Mc Ardle BA, Davies RA, Chen L, et al. Prognostic value of rubidium-82 positron emission tomography in patients after heart transplant. Circ Cardiovasc Imaging. 2014;7(6):930–7.
Nelson LM, Christensen TE, Rossing K, Hasbak P, Gustafsson F. Prognostic value of myocardial flow reserve obtained by 82-rubidium positron emission tomography in long-term follow-up after heart transplantation. J Nucl Cardiol. 2021.
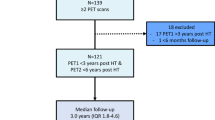
•• Feher A, Srivastava A, Quail MA, et al. Serial assessment of coronary flow reserve by rubidium-82 positron emission tomography predicts mortality in heart transplant recipients. JACC Cardiovasc Imaging. 2020;13(1 Pt 1):109–20. This study showed the long-term prognostic value of PET myocardial blood flow quantification as well as the value of serial PET assessments in heart transplant patients.
Zhao XM, Delbeke D, Sandler MP, Yeoh TK, Votaw JR, Frist WH. Nitrogen-13-ammonia and PET to detect allograft coronary artery disease after heart transplantation: comparison with coronary angiography. J Nucl Med. 1995;36(6):982–7.
Kushwaha SS, Narula J, Narula N, et al. Pattern of changes over time in myocardial blood flow and microvascular dilator capacity in patients with normally functioning cardiac allografts. Am J Cardiol. 1998;82(11):1377–81.
Preumont N, Berkenboom G, Vachiery J, et al. Early alterations of myocardial blood flow reserve in heart transplant recipients with angiographically normal coronary arteries. J Heart Lung Transplant. 2000;19(6):538–45.
Wiefels C, Almufleh A, Yao J, et al. Prognostic utility of longitudinal quantification of PET myocardial blood flow early post heart transplantation. J Nucl Cardiol. 2022;29(2):712–23.
Raichlin E, Edwards BS, Kremers WK, et al. Acute cellular rejection and the subsequent development of allograft vasculopathy after cardiac transplantation. J Heart Lung Transplant. 2009;28(4):320–7.
Asimacopoulos EP, Garbern JC, Gauvreau K, Blume ED, Daly KP, Singh TP. Association of clinical rejection versus rejection on protocol biopsy with cardiac allograft vasculopathy in pediatric heart transplant recipients. Transplantation. 2020;104(1):e31–7.
Svobodova E, Gazdic T, Kubanek M, et al. Novel insights into pretransplant allosensitization in heart transplant recipients in the contemporary era of immunosuppression and rejection surveillance. Transpl Int. 2016;29(1):63–72.
Su JA, Baxter-Lowe LA, Kantor PF, Szmuszkovicz JR, Menteer J. The clinical impact of donor-specific antibodies on antibody-mediated rejection and long-term prognosis after heart transplantation. Curr Opin Organ Transplant. 2019;24(3):245–51.
Chan SY, Kobashigawa J, Stevenson LW, Brownfield E, Brunken RC, Schelbert HR. Myocardial blood flow at rest and during pharmacological vasodilation in cardiac transplants during and after successful treatment of rejection. Circulation. 1994;90(1):204–12.
Feher A, Sinusas AJ. Evaluation of cardiac allograft vasculopathy by positron emission tomography. J Nucl Cardiol. 2021;28(6):2616–28.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Dr. Feher has nothing to disclose. Dr. Miller reports personal fees from Roivant, Pfizer, and Alnylam and grants from Eidos, Pfizer, Alnylam, and NIH, outside the submitted work.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Nuclear Cardiology
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Feher, A., Miller, E.J. PET Myocardial Blood Flow for Post-transplant Surveillance and Cardiac Allograft Vasculopathy in Heart Transplant Recipients. Curr Cardiol Rep 24, 1865–1871 (2022). https://doi.org/10.1007/s11886-022-01804-3
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11886-022-01804-3