Abstract
Purpose of Review
Exercise causes various dynamic changes in all body parts either in healthy subject or in heart failure (HF) patients. The present review of current knowledge about HF patients with reduced ejection fraction focuses on dynamic changes along a “metabo-hemodynamic” perspective.
Recent Findings
Studies on the dynamic changes occurring during exercise span many years. Thanks to the availability of advanced methods, it is nowadays possible to properly characterize respiratory, hemodynamic, and muscular function adjustments and their mismatch with the pulmonary and systemic circulations.
Summary
Exercise is a dynamic event that involves several body functions. In HF patients, it is important to know at what level the limitation takes place in order to better manage these patients and to optimize therapeutic strategies.





Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
Ponikowski P, et al. ESC guidelines for the diagnosis and treatment of acute and chronic heart failure. Rev Esp Cardiol (Engl Ed). 2016;69(12):1167.
Dempsey JA, Vidruk EH, Mitchell GS. Pulmonary control systems in exercise: update. Fed Proc. 1985;44(7):2260–70.
Cundrle I Jr, Olson LJ, Johnson BD. Pulmonary limitations in heart failure. Clin Chest Med. 2019;40(2):439–48.
Wasserman K, Zhang YY, Gitt A, Belardinelli R, Koike A, Lubarsky L, et al. Lung function and exercise gas exchange in chronic heart failure. Circulation. 1997;96(7):2221–7.
Piepoli M, Clark AL, Volterrani M, Adamopoulos S, Sleight P, Coats AJS. Contribution of muscle afferents to the hemodynamic, autonomic, and ventilatory responses to exercise in patients with chronic heart failure: effects of physical training. Circulation. 1996;93(5):940–52.
Chua TP, Ponikowski PP, Harrington D, Chambers J, Coats AJ. Contribution of peripheral chemoreceptors to ventilation and the effects of their suppression on exercise tolerance in chronic heart failure. Heart. 1996;76(6):483–9.
Agostoni P, Bussotti M, Cattadori G, Margutti E, Contini M, Muratori M, et al. Gas diffusion and alveolar-capillary unit in chronic heart failure. Eur Heart J. 2006;27(21):2538–43.
Morosin M, Vignati C, Novi A, Salvioni E, Veglia F, Alimento M, et al. The alveolar to arterial oxygen partial pressure difference is associated with pulmonary diffusing capacity in heart failure patients. Respir Physiol Neurobiol. 2016;233:1–6.
Agostoni PG, Bussotti M, Palermo P, Guazzi M. Does lung diffusion impairment affect exercise capacity in patients with heart failure? Heart. 2002;88(5):453–9.
Agostoni P, Apostolo A, Cattadori G, Salvioni E, Berna G, Antonioli L, et al. Effects of beta-blockers on ventilation efficiency in heart failure. Am Heart J. 2010;159(6):1067–73.
Agostoni P, Cattadori G, Bussotti M, Apostolo A. Cardiopulmonary interaction in heart failure. Pulm Pharmacol Ther. 2007;20(2):130–4.
Kraemer MD, Kubo SH, Rector TS, Brunsvold N, Bank AJ. Pulmonary and peripheral vascular factors are important determinants of peak exercise oxygen uptake in patients with heart failure. J Am Coll Cardiol. 1993;21(3):641–8.
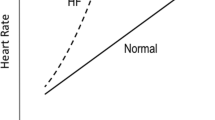
Hansen JE, Sue DY, Oren A, Wasserman K. Relation of oxygen uptake to work rate in normal men and men with circulatory disorders. Am J Cardiol. 1987;59(6):669–74.
Koike A, et al. Evidence that the metabolic acidosis threshold is the anaerobic threshold. J Appl Physiol (1985). 1990;68(6):2521–6.
Wagner PD. Gas exchange and peripheral diffusion limitation. Med Sci Sports Exerc. 1992;24(1):54–8.
Zweerink A, et al. Chronotropic incompetence in chronic heart failure. Circ Heart Fail. 2018;11(8):e004969.
Brubaker PH, Kitzman DW. Chronotropic incompetence: causes, consequences, and management. Circulation. 2011;123(9):1010–20.
Agostoni P, Emdin M, Corra U, Veglia F, Magri D, Tedesco CC, et al. Permanent atrial fibrillation affects exercise capacity in chronic heart failure patients. Eur Heart J. 2008;29(19):2367–72.
Witte KK, Clark AL. Chronotropic incompetence in heart failure. J Am Coll Cardiol. 2006;48(3):595; author reply 595-6–595; author reply 596.
Brawner CA, Ehrman JK, Schairer JR, Cao JJ, Keteyian SJ. Predicting maximum heart rate among patients with coronary heart disease receiving beta-adrenergic blockade therapy. Am Heart J. 2004;148(5):910–4.
Magri D, et al. Cardiovascular mortality and chronotropic incompetence in systolic heart failure: the importance of a reappraisal of current cut-off criteria. Eur J Heart Fail. 2014;16(2):201–9.
Magri D, et al. Chronotropic incompentence and functional capacity in chronic heart failure: no role of beta-blockers and beta-blocker dose. Cardiovasc Ther. 2012;30(2):100–8.
Wilson JR, Martin JL, Schwartz D, Ferraro N. Exercise intolerance in patients with chronic heart failure: role of impaired nutritive flow to skeletal muscle. Circulation. 1984;69(6):1079–87.
Miyazaki A, Adachi H, Oshima S, Taniguchi K, Hasegawa A, Kurabayashi M. Blood flow redistribution during exercise contributes to exercise tolerance in patients with chronic heart failure. Circ J. 2007;71(4):465–70.
Zelis R, Flaim SF. Alterations in vasomotor tone in congestive heart failure. Prog Cardiovasc Dis. 1982;24(6):437–59.
Agostoni P, Wasserman K, Perego GB, Marenzi GC, Guazzi M, Assanelli E, et al. Oxygen transport to muscle during exercise in chronic congestive heart failure secondary to idiopathic dilated cardiomyopathy. Am J Cardiol. 1997;79(8):1120–4.
Cattadori G, Schmid JP, Brugger N, Gondoni E, Palermo P, Agostoni P. Hemodynamic effects of exercise training in heart failure. J Card Fail. 2011;17(11):916–22.
Ye LF, Wang SM, Wang LH. Efficacy and safety of exercise rehabilitation for heart failure patients with cardiac resynchronization therapy: a systematic review and meta-analysis. Front Physiol. 2020;11:980.
Schlosshan D, Barker D, Pepper C, Williams G, Morley C, Tan LB. CRT improves the exercise capacity and functional reserve of the failing heart through enhancing the cardiac flow- and pressure-generating capacity. Eur J Heart Fail. 2006;8(5):515–21.
Linde C, Ellenbogen K, McAlister FA. Cardiac resynchronization therapy (CRT): clinical trials, guidelines, and target populations. Heart Rhythm. 2012;9(8 Suppl):S3–S13.
Cattadori G, Giraldi F, Berti M, Carbucicchio C, Pepi M, Della Bella P, et al. Assessment of cardiac resynchronization therapy response. Int J Cardiol. 2009;136(2):240–2.
Convertino VA, Keil LC, Bernauer EM, Greenleaf JE. Plasma volume, osmolality, vasopressin, and renin activity during graded exercise in man. J Appl Physiol Respir Environ Exerc Physiol. 1981;50(1):123–8.
Perego GB, et al. Contribution of PO2, P50, and Hb to changes in arteriovenous O2 content during exercise in heart failure. J Appl Physiol (1985). 1996;80(2):623–31.
Agostoni P, Wasserman K, Guazzi M, Cattadori G, Palermo P, Marenzi G, et al. Exercise-induced hemoconcentration in heart failure due to dilated cardiomyopathy. Am J Cardiol. 1999;83(2):278–80 A6.
Agostoni P, Cerino M, Palermo P, Magini A, Bianchi M, Bussotti M, et al. Exercise capacity in patients with beta-thalassaemia intermedia. Br J Haematol. 2005;131(2):278–81.
Agostoni P, et al. Relationship of resting hemoglobin concentration to peak oxygen uptake in heart failure patients. Am J Hematol. 2010;85(6):414–7.
Magri D, et al. Anemia and Iron deficiency in heart failure: clinical and prognostic role. Heart Fail Clin. 2019;15(3):359–69.
Tanner H, Moschovitis G, Kuster GM, Hullin R, Pfiffner D, Hess OM, et al. The prevalence of anemia in chronic heart failure. Int J Cardiol. 2002;86(1):115–21.
Silverberg DS, Wexler D, Blum M, Keren G, Sheps D, Leibovitch E, et al. The use of subcutaneous erythropoietin and intravenous iron for the treatment of the anemia of severe, resistant congestive heart failure improves cardiac and renal function and functional cardiac class, and markedly reduces hospitalizations. J Am Coll Cardiol. 2000;35(7):1737–44.
Maggioni AP, Opasich C, Anand I, Barlera S, Carbonieri E, Gonzini L, et al. Anemia in patients with heart failure: prevalence and prognostic role in a controlled trial and in clinical practice. J Card Fail. 2005;11(2):91–8.
Tang YD, Katz SD. Anemia in chronic heart failure: prevalence, etiology, clinical correlates, and treatment options. Circulation. 2006;113(20):2454–61.
Harnett JD, Kent GM, Foley RN, Parfrey PS. Cardiac function and hematocrit level. Am J Kidney Dis. 1995;25(4 Suppl 1):S3–7.
Agostoni P, Cattadori G. Noninvasive cardiac output measurement: a new tool in heart failure. Cardiology. 2009;114(4):244–6.
Benedetto D, Rao CM, Cefalù C, Aguglia DO, Cattadori G, D’Ascola DG, et al. Effects of blood transfusion on exercise capacity in thalassemia major patients. PLoS One. 2015;10(5):e0127553.
Agostoni P, Assanelli E, Guazzi M, Grazi M, Perego GB, Lomanto M, et al. Mechanisms facilitating oxygen delivery during exercise in patients with chronic heart failure. Cardiologia. 1997;42(7):743–50.
Hamaoka T, McCully KK, Quaresima V, Yamamoto K, Chance B. Near-infrared spectroscopy/imaging for monitoring muscle oxygenation and oxidative metabolism in healthy and diseased humans. J Biomed Opt. 2007;12(6):062105.
Hirsch DJ, Cooper JR Jr. Cardiac failure and left ventricular assist devices. Anesthesiol Clin North Am. 2003;21(3):625–38.
Apostolo A, et al. Comprehensive effects of left ventricular assist device speed changes on alveolar gas exchange, sleep ventilatory pattern, and exercise performance. J Heart Lung Transplant. 2018;37(11):1361–71 First integrated analysis on the effects of cardiac output changes in LVAD patients on several body functions. This paper has clinical and physiological relevance.
Koike A, Wasserman K, Taniguchi K, Hiroe M, Marumo F. Critical capillary oxygen partial pressure and lactate threshold in patients with cardiovascular disease. J Am Coll Cardiol. 1994;23(7):1644–50.
Agostoni PG, Guazzi M, Bussotti M, Grazi M, Palermo P, Marenzi G. Lack of improvement of lung diffusing capacity following fluid withdrawal by ultrafiltration in chronic heart failure. J Am Coll Cardiol. 2000;36(5):1600–4.
Agostoni P, Magini A, Andreini D, Contini M, Apostolo A, Bussotti M, et al. Spironolactone improves lung diffusion in chronic heart failure. Eur Heart J. 2005;26(2):159–64.
Guazzi M. Alveolar gas diffusion abnormalities in heart failure. J Card Fail. 2008;14(8):695–702.
Mettauer B, Lampert E, Charloux A, Zhao QM, Epailly E, Oswald M, et al. Lung membrane diffusing capacity, heart failure, and heart transplantation. Am J Cardiol. 1999;83(1):62–7.
Hoppeler H, Lüthi P, Claassen H, Weibel ER, Howald H. The ultrastructure of the normal human skeletal muscle. A morphometric analysis on untrained men, women and well-trained orienteers. Pflugers Arch. 1973;344(3):217–32.
Schrepper A, Schwarzer M, Schöpe M, Amorim PA, Doenst T. Biphasic response of skeletal muscle mitochondria to chronic cardiac pressure overload - role of respiratory chain complex activity. J Mol Cell Cardiol. 2012;52(1):125–35.
Sullivan MJ, Green HJ, Cobb FR. Skeletal muscle biochemistry and histology in ambulatory patients with long-term heart failure. Circulation. 1990;81(2):518–27.
Drexler H, Riede U, Münzel T, König H, Funke E, Just H. Alterations of skeletal muscle in chronic heart failure. Circulation. 1992;85(5):1751–9.
Schaufelberger M, Eriksson BO, Grimby G, Held P, Swedberg K. Skeletal muscle fiber composition and capillarization in patients with chronic heart failure: relation to exercise capacity and central hemodynamics. J Card Fail. 1995;1(4):267–72.
Philippou A, Xanthis D, Chryssanthopοulos C, Maridaki M, Koutsilieris M. Heart failure-induced skeletal muscle wasting. Curr Heart Fail Rep. 2020;17(5):299–308.
Takada S, Sabe H, Kinugawa S. Abnormalities of skeletal muscle, adipocyte tissue, and lipid metabolism in heart failure: practical therapeutic targets. Front Cardiovasc Med. 2020;7:79.
Caforio AL, et al. Type 1 fiber abnormalities in skeletal muscle of patients with hypertrophic and dilated cardiomyopathy: evidence of subclinical myogenic myopathy. J Am Coll Cardiol. 1989;14(6):1464–73.
Severinghaus JW. Paradoxical relation of mitochondrial PO2 to Vo(2). Oxygen Transport to Tissue Xxi. 1999;471:595–604.
Radak Z, Zhao Z, Koltai E, Ohno H, Atalay M. Oxygen consumption and usage during physical exercise: the balance between oxidative stress and ROS-dependent adaptive signaling. Antioxid Redox Signal. 2013;18(10):1208–46.
Tucker WJ, et al. Impaired exercise tolerance in heart failure: role of skeletal muscle morphology and function. Curr Heart Fail Rep. 2018;15(6):323–31 Nice review on the importance of the scheletal muscle function and the anatomy changes in heart failure.
Del Torto A, et al. Contribution of central and peripheral factors at peak exercise in heart failure patients with progressive severity of exercise limitation. Int J Cardiol. 2017;248:252–6.
Cattadori G, Schmid JP, Agostoni P. Noninvasive measurement of cardiac output during exercise by inert gas rebreathing technique. Heart Fail Clin. 2009;5(2):209–15.
Gabrielsen A, et al. Non-invasive measurement of cardiac output in heart failure patients using a new foreign gas rebreathing technique. Clin Sci (Lond). 2002;102(2):247–52.
Kemps HM, et al. Evaluation of two methods for continuous cardiac output assessment during exercise in chronic heart failure patients. J Appl Physiol (1985). 2008;105(6):1822–9.
Charloux A, Lonsdorfer-Wolf E, Richard R, Lampert E, Oswald-Mammosser M, Mettauer B, et al. A new impedance cardiograph device for the non-invasive evaluation of cardiac output at rest and during exercise: comparison with the "direct" Fick method. Eur J Appl Physiol. 2000;82(4):313–20.
Vignati C, Apostolo A, Cattadori G, Farina S, del Torto A, Scuri S, et al. Lvad pump speed increase is associated with increased peak exercise cardiac output and vo2, postponed anaerobic threshold and improved ventilatory efficiency. Int J Cardiol. 2017;230:28–32.
Fresiello L, Jacobs S, Timmermans P, Buys R, Hornikx M, Goetschalckx K, et al. Limiting factors of peak and submaximal exercise capacity in LVAD patients. PLoS One. 2020;15(7):e0235684.
Gross C, Marko C, Mikl J, Altenberger J, Schlöglhofer T, Schima H, et al. LVAD pump flow does not adequately increase with exercise. Artif Organs. 2019;43(3):222–8.
Cairo G, Bernuzzi F, Recalcati S. A precious metal: Iron, an essential nutrient for all cells. Genes Nutr. 2006;1(1):25–39.
Beard JL. Iron biology in immune function, muscle metabolism and neuronal functioning. J Nutr. 2001;131(2S-2):568S–79S discussion 580S.
Munoz M, Villar I, Garcia-Erce JA. An update on iron physiology. World J Gastroenterol. 2009;15(37):4617–26.
Anderson GJ, Vulpe CD. Mammalian iron transport. Cell Mol Life Sci. 2009;66(20):3241–61.
Bolger AP, Bartlett FR, Penston HS, O’Leary J, Pollock N, Kaprielian R, et al. Intravenous iron alone for the treatment of anemia in patients with chronic heart failure. J Am Coll Cardiol. 2006;48(6):1225–7.
Anker SD, Comin Colet J, Filippatos G, Willenheimer R, Dickstein K, Drexler H, et al. Ferric carboxymaltose in patients with heart failure and iron deficiency. N Engl J Med. 2009;361(25):2436–48.
Okonko DO, Grzeslo A, Witkowski T, Mandal AKJ, Slater RM, Roughton M, et al. Effect of intravenous iron sucrose on exercise tolerance in anemic and nonanemic patients with symptomatic chronic heart failure and iron deficiency FERRIC-HF: a randomized, controlled, observer-blinded trial. J Am Coll Cardiol. 2008;51(2):103–12.
Ponikowski P, van Veldhuisen DJ, Comin-Colet J, Ertl G, Komajda M, Mareev V, et al. Beneficial effects of long-term intravenous iron therapy with ferric carboxymaltose in patients with symptomatic heart failure and iron deficiencydagger. Eur Heart J. 2015;36(11):657–68.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Dr. Agostoni reports non-financial support from Menarini, Novartis, and Boeringer; grants and non-financial support from Actelion; and grants from Daiichi Sankyo and Bayer.
The other authors declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
All reports studies/experiments with human or animal subjects performed by the authors have been previously published and complied with all applicable ethical standards (including the Helsinki declaration and its amendments, institutional/national research committee standards, and international/national/institutional guidelines).
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Myocardial Disease
Rights and permissions
About this article
Cite this article
Rovai, S., Mattavelli, I., Salvioni, E. et al. Exercise Dynamic of Patients with Chronic Heart Failure and Reduced Ejection Fraction. Curr Cardiol Rep 23, 92 (2021). https://doi.org/10.1007/s11886-021-01491-6
Accepted:
Published:
DOI: https://doi.org/10.1007/s11886-021-01491-6