Abstract
Purpose of Review
This review will allow the reader to understand the rationale for urodynamic testing in a child who is neurologically intact and is suspected of having dysfunctional voiding. We will look to define criteria that will prevent the overuse and unnecessary use of this invasive test in children.
Recent findings
The literature does not support the routine use of invasive urodynamics for children with urge syndrome but does support its use for elucidation of dysfunctional voiding abnormalities in neurologically intact children.
Summary
The child with functional voiding issues presents itself with factors that are different from the child with neurogenic causes of incontinence. The role of the brain cannot be taken out of the equation in the normal sensate child and its impact can be quite significant leading to results that may not be what is actually occurring in day to day life. It is also critical that the person ordering VUD understand that there is limited value in ordering these tests for urge incontinence and frequency since the diagnosis of DO can be made for the most part from the history. Judicious use of the VUD study can be quiet valuable in allowing the user to pinpoint in complex cases the cause of the incontinence or poor voiding dynamics that are present. VUD should be a final choice in the workup of the sensate child with functional voiding problems and rarely used as a first line evaluation.






Similar content being viewed by others
References
Austin PF, Bauer SB, Bower W, Chase J, Franco I, Hoebeke P, et al. The standardization of terminology of lower urinary tract function in children and adolescents: update report from the Standardization Committee of the International Children's Continence Society. J Urol. 2014;191:1863–1865.e13.
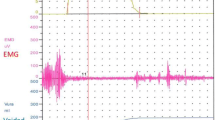
Combs AJ, Grafstein N, Horowitz M, et al. Primary bladder neck dysfunction in children and adolescents I: pelvic floor electromyography lag time—a new noninvasive method to screen for and monitor therapeutic response. J Urol. 2005;173:207–10; discussion 10–1.
Franco I, Grantham EC, Cubillos J, et al. Can a simple question predict prolonged uroflow lag times in children? J Pediatr Urol. 2016;12(157):e1–8.
Hoebeke P, Van Laecke E, Van Camp C, et al. One thousand video-urodynamic studies in children with non-neurogenic bladder sphincter dysfunction. BJU Int. 2001;87:575–80.
Webster GD, Koefoot RB Jr, Sihelnik S. Urodynamic abnormalities in neurologically normal children with micturition dysfunction. J Urol. 1984;132:74–7.
Borzyskowski M, Mundy AR. Videourodynamic assessment of diurnal urinary incontinence. Arch Dis Child. 1987;62:128–31.
Mayo ME, Burns MW. Urodynamic studies in children who wet. Br J Urol. 1990;65:641–5.
Weerasinghe N, Malone PS. The value of videourodynamics in the investigation of neurologically normal children who wet. Br J Urol. 1993;71:539–42.
Glazier DB, Murphy DP, Fleisher MH, et al. Evaluation of the utility of video-urodynamics in children with urinary tract infection and voiding dysfunction. Br J Urol. 1997;80:806–8.
Kaufman MR, DeMarco RT, Pope JC t, et al. High yield of urodynamics performed for refractory nonneurogenic dysfunctional voiding in the pediatric population. J Urol. 2006;176:1835–7.
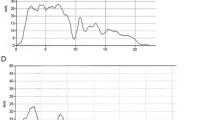
Franco I, Shei-Dei Yang S, Chang SJ, Nussenblatt B, Franco JA. A quantitative approach to the interpretation of uroflowmetry in children. Neurourol Urodyn. 2015;35(7):836–46. https://doi.org/10.1002/nau.22813.
Bael A, Lax H, de Jong TP, et al. The relevance of urodynamic studies for urge syndrome and dysfunctional voiding: a multicenter controlled trial in children. J Urol. 2008;180:1486–93; discussion 94–5.
Stone JJ, Rozzelle CJ, Greenfield SP. Intractable voiding dysfunction in children with normal spinal imaging: predictors of failed conservative management. Urology. 2010;75:161–5.
Hubeaux K, Deffieux X, Raibaut P, le Breton F, Jousse M, Amarenco G. Evidence for autonomic nervous system dysfunction in females with idiopathic overactive bladder syndrome. Neurourol Urodyn. 2011;30:1467–72.
Unalacak M, Aydin M, Ermis B, Ozeren A, Sogut A, Demirel F, et al. Assessment of cardiac autonomic regulation in children with monosymptomatic nocturnal enuresis by analysis of heart rate variability. Tohoku J Exp Med. 2004;204:63–9.
Ambartsumyan L, Siddiqui A, Bauer S, Nurko S. Simultaneous urodynamic and anorectal manometry studies in children: insights into the relationship between the lower gastrointestinal and lower urinary tracts. Neurogastroenterol Motil. 2016;28:924–33.
Burgers R, Liem O, Canon S, Mousa H, Benninga MA, di Lorenzo C, et al. Effect of rectal distention on lower urinary tract function in children. J Urol. 2010;184:1680–5.
Panayi DC, Khullar V, Digesu GA, Spiteri M, Hendricken C, Fernando R. Rectal distension: the effect on bladder function. Neurourol Urodyn. 2011;30:344–7.
Blethyn AJ, Jenkins HR, Roberts R, Verrier Jones K. Radiological evidence of constipation in urinary tract infection. Arch Dis Child. 1995;73:534–5.
Herz D, Weiser A, Collett T, et al. Dysfunctional elimination syndrome as an etiology of idiopathic urethritis in childhood. J Urol. 2005;173:2132–7.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Israel Franco declares that he has no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Pediatric Voiding Dysfunction
Rights and permissions
About this article
Cite this article
Franco, I. Utility of Urodynamics in Children with Dysfunctional Voiding. Curr Bladder Dysfunct Rep 13, 178–190 (2018). https://doi.org/10.1007/s11884-018-0466-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11884-018-0466-3