Abstract
Purpose
This review aims to discuss the diagnosis and assessment of dysfunctional voiding in both children and adults.
Recent Findings
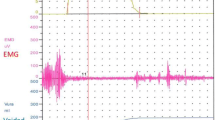
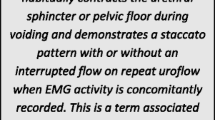
Although the pillars of diagnosing dysfunctional voiding are a history, physical exam, and uroflowmetry with electromyography or urodynamics, new technology may aid in this evaluation. The use of urinary biomarkers may be a helpful, non-invasive adjunct in diagnosis. In addition, novel devices and smartphone apps may make diagnosis more accessible to patients and providers.
Summary
Dysfunctional voiding refers to the condition where there is a lack of coordination between the sphincter and detrusor muscle during bladder emptying in the absence of anatomic or neurologic cause. Commonly diagnosed in children, this condition may persist or be diagnosed de novo in adulthood. As such, thorough evaluation is critical to diagnosis to prevent recurrent infections and deterioration of the upper urinary tract. Uroflowmetry, with or without electromyography, and/or urodynamics remain the gold standard for diagnosis, while new technology may facilitate evaluation.


Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Everaert K, Van Laecke E, De Muynck M, Peeters H, Hoebeke P. Urodynamic assessment of voiding dysfunction and dysfunctional voiding in girls and women. Int Urogynecology J. 2000;11:254–64.
Hinman F, Baumann FW. Vesical and ureteral damage from voiding dysfunction in boys without neurologic or obstructive disease. J Urol. 1973;109:727–32.
Allen TD. The non-neurogenic neurogenic bladder. J Urol. 1977;117:232–8.
Abrams P, Cardozo L, Fall M, Griffiths D, Rosier P, Ulmsten U, van Kerrebroeck P, Victor A, Wein A, Standardisation Sub-committee of the International Continence Society. The standardisation of terminology of lower urinary tract function: report from the Standardisation Sub-committee of the International Continence Society. Neurourol Urodyn. 2002;21:167–78.
Austin PF, Bauer SB, Bower W, et al. The standardization of terminology of lower urinary tract function in children and adolescents: update report from the standardization committee of the International Children’s Continence Society. Neurourol Urodyn. 2016;35:471–81.
Sinha S. Dysfunctional voiding: a review of the terminology, presentation, evaluation and management in children and adults. Indian J Urol IJU J Urol Soc India. 2011;27:437–47.
Feldman AS, Bauer SB. Diagnosis and management of dysfunctional voiding. Curr Opin Pediatr. 2006;18:139–47.
Fernandez-Ibieta M, Ayuso-Gonzalez L. Dysfunctional voiding in pediatrics: a review of pathophysiology and current treatment modalities. Curr Pediatr Rev. 2016;12:292–300.
Groutz A, Blaivas JG, Pies C, Sassone AM. Learned voiding dysfunction (non-neurogenic, neurogenic bladder) among adults. Neurourol Urodyn. 2001;20:259–68.
Hinman F. Nonneurogenic neurogenic bladder (the Hinman syndrome)--15 years later. J Urol. 1986;136:769–77.
Sandri S. 470 - Adult follow up of major dysfunctional voiding in children. Eur Urol Suppl. 2017;16:e817–8.
Clothier JC, Wright AJ. Dysfunctional voiding: the importance of non-invasive urodynamics in diagnosis and treatment. Pediatr Nephrol. 2018;33:381–94.
Swinn MJ, Fowler CJ. Isolated urinary retention in young women, or Fowler’s syndrome. Clin Auton Res Off J Clin Auton Res Soc. 2001;11:309–11.
Morin F, Akhavizadegan H, Kavanagh A, Moore K. Dysfunctional voiding: challenges of disease transition from childhood to adulthood. Can Urol Assoc J J Assoc Urol Can. 2018;12:S42–7.
Özen MA, Mutluer T, Necef I, Shabsog M, Taşdemir M, Bilge I, Eroğlu E. The overlooked association between lower urinary tract dysfunction and psychiatric disorders: a short screening test for clinical practice. J Pediatr Urol. 2019;15:332.e1–5.
Ho G-R, Wei C-W, Kuo H-C. Voiding dysfunction due to urethral sphincter dysfunction might be an early neurological presentation of central nervous system disorders in aged patients. J Pers Med. 2023;13:693.
Jiang R, Kelly MS, Routh JC. Assessment of pediatric bowel and bladder dysfunction: a critical appraisal of the literature. J Pediatr Urol. 2018;14:494–501.
Farhat W, Bägli DJ, Capolicchio G, O’Reilly S, Merguerian PA, Khoury A, McLorie GA. The dysfunctional voiding scoring system: quantitative standardization of dysfunctional voiding symptoms in children. J Urol. 2000;164:1011–5.
Nelson CP, Park JM, Bloom DA, Wan J, Dunn RL, Wei JT. Incontinence Symptom Index-Pediatric: development and initial validation of a urinary incontinence instrument for the older pediatric population. J Urol. 2007;178:1763–7. discussion 1767
Sureshkumar P, Craig JC, Roy LP, Knight JF. A reproducible pediatric daytime urinary incontinence questionnaire. J Urol. 2001;165:569–73.
Ebiloglu T, Kaya E, Kopru B, Ergin G, Sahin S, Irkilata HC, Kibar Y. Concised form for lower urinary tract dysfunction symptom scale in children. J Clin Diagn Res JCDR. 2016;10:PC04–6.
Krishnappa P, Sinha M, Krishnamoorthy V. A prospective study to evaluate the efficacy of botulinum toxin-a in the management of dysfunctional voiding in women. Clin Med Insights Womens Health. 2018;11
• Chiang C-H, Jiang Y-H, Kuo H-C. Therapeutic efficacy of biofeedback pelvic floor muscle exercise in women with dysfunctional voiding. Sci Rep. 2021;11:13757. Study that highlighted the clinical tools used to diagnose dysfunctional voiding
Cameron AP, Wiseman JB, Smith AR, et al. Are Three-Day Voiding Diaries Feasible and Reliable? Results from the Symptoms of Lower Urinary Tract Dysfunction Research Network (LURN) Cohort. Neurourol Urodyn. 2019;38:2185–93.
López-Fando L, Santiago M, Ruiz M, et al. Is the first day of the bladder diary enough for symptom assessment in women with lower urinary tract symptoms? Continence. 2022;2:100026.
Lopes I, Veiga ML, Braga AA, Brasil CA, Hoffmann A, Barroso U Jr. A two-day bladder diary for children: is it enough? J Pediatr Urol. 2015;11:348.e1–4.
Mateu Arrom L, Peri Cusi L, López-Fando L, Franco de Castro A, Jiménez Cidre MÁ, Alcaraz A. Validation of a 3 day electronic bladder diary as an app for smart-phone. Neurourol Urodyn. 2019;38:764–9.
Whangbo T-K, Eun S-J, Jung E-Y, Park DK, Kim SJ, Kim CH, Chung KJ, Kim K-H. Personalized urination activity recognition based on a recurrent neural network using smart band. Int Neurourol J. 2018;22:S91–100.
Fuentes M, Magalhães J, Barroso U. Diagnosis and management of bladder dysfunction in neurologically normal children. Front Pediatr. 2019;7:298.
Quaghebeur J, Petros P, Wyndaele J-J, De Wachter S. Pelvic-floor function, dysfunction, and treatment. Eur J Obstet Gynecol Reprod Biol. 2021;265:143–9.
• Jiang Y-H, Jhang J-F, Ho H-C, Hsu Y-H, Kuo H-C. Diagnostic and prognostic value of urine biomarkers among women with dysfunctional voiding. Sci Rep. 2022;12:6608. Novel use of biomarkers in diagnosing dysfunctional voiding
Siddiqui NY, Helfand BT, Andreev VP, et al. Biomarkers implicated in lower urinary tract symptoms: systematic review and pathway analyses. J Urol. 2019;202:880–9.
Van Batavia JP, Combs AJ. The role of non-invasive testing in evaluation and diagnosis of pediatric lower urinary tract dysfunction. Curr Urol Rep. 2018;19:34.
Ballstaedt L, Woodbury B. Bladder post void residual volume. StatPearls; 2023.
Chang S-J, Chiang I-N, Hsieh C-H, Lin C-D, Yang SS-D. Age- and gender-specific nomograms for single and dual post-void residual urine in healthy children. Neurourol Urodyn. 2013;32:1014–8.
Scarpero H. Urodynamics in the evaluation of female LUTS: when are they helpful and how do we use them? Urol Clin North Am. 2014;41:429–38.
Tangal S, Gökçe Mİ, Özayar A, Gülpınar B, Haliloğlu AH, Burgu B, Özdiler E. Evaluation of a new ultrasound measurement tool for the diagnosis of dysfunctional voiding in pediatric population: full/empty bladder wall thickness ratio. Urology. 2014;83:1369–72.
Chan L. Pelvic ultrasound in the assessment of female voiding dysfunction. In: Chan L, Tse V, The S, Stewart P, editors. Pelvic floor ultrasound Princ. Appl. Case Stud. Cham: Springer International Publishing; 2015. p. 63–76.
Stoffel JT, Peterson AC, Sandhu JS, Suskind AM, Wei JT, Lightner DJ. AUA white paper on nonneurogenic chronic urinary retention: consensus definition, treatment algorithm, and outcome end points. J Urol. 2017;198:153–60.
Franco I, Shei-Dei Yang S, Chang S-J, Nussenblatt B, Franco JA. A quantitative approach to the interpretation of uroflowmetry in children. Neurourol Urodyn. 2016;35:836–46.
Dayanc MM, Kibar Y, Irkilata HC, Sancaktutar AA, Ebiloglu T, Gur A, Ergin G, Alp BF, Gok F. Effect of voided volume on voiding patterns and reliability of uroflowmetry-electromyography results in children with lower urinary tract dysfunction. Low Urin Tract Symptoms. 2017;9:46–51.
Winters JC, Dmochowski RR, Goldman HB, et al. Urodynamic studies in adults: AUA/SUFU guideline. J Urol. 2012;188:2464–72.
•• Sinha S, Yang CC, Arlandis S, Goldman HB. Female voiding dysfunction: a review of clinical presentation, urodynamic diagnosis and management. Continence. 2023;6:100578. Review on voiding dysfunction in women
Wenske S, Van Batavia JP, Combs AJ, Glassberg KI. Analysis of uroflow patterns in children with dysfunctional voiding. J Pediatr Urol. 2014;10:250–4.
Netto JMB, Hittelman A, Lambert S, Murphy K, Collette-Gardere T, Franco I. Interpretation of uroflow curves: a global survey measuring inter and intra rater reliability. Neurourol Urodyn. 2020;39:826–32.
Yang SS-D, Chang S-J. Uroflowmetry and postvoid residual urine tests in incontinent children. In: Pediatr. Incontinence. John Wiley & Sons Ltd; 2015. p. 99–106.
Gupta DK, Sankhwar SN, Goel A. Uroflowmetry nomograms for healthy children 5 to 15 years old. J Urol. 2013;190:1008–14.
Franco I, Franco J, Lee YS, Choi EK, Han SW. Can a quantitative means be used to predict flow patterns: agreement between visual inspection vs. flow index derived flow patterns. J Pediatr Urol. 2016;12:218.e1–8.
• Schultz RE. Smartphone app for in-home uroflowmetry. Urol Pract. 2022;9:524–30. New technology for at home uroflow
Matulewicz RS, Hairston JC. The UroCuff test: a non-invasive alternative to pressure flow studies in adult males with lower urinary tract symptoms secondary to bladder outlet obstruction. Can J Urol. 2015;22:7896–901.
Khosla L, Codelia-Anjum A, Sze C, Martinez Diaz S, Zorn KC, Bhojani N, Elterman D, Chughtai B. Use of the penile cuff test to diagnose bladder outlet obstruction: a systematic review and meta-analysis. LUTS Low Urin Tract Symptoms. 2022;14:318–28.
Glassberg KI, Van Batavia JP, Combs AJ. Can children with either overactive bladder or dysfunctional voiding transition from one into the other: are both part of a single entity? J Pediatr Urol. 2016;12:217.e1–8.
Chen Y-C, Kuo H-C. Clinical and video urodynamic characteristics of adult women with dysfunctional voiding. J Formos Med Assoc Taiwan Yi Zhi. 2014;113:161–5.
Peng C-H, Chen S-F, Kuo H-C. Videourodynamic analysis of the urethral sphincter overactivity and the poor relaxing pelvic floor muscles in women with voiding dysfunction. Neurourol Urodyn. 2017;36:2169–75.
Saxton HM, Borzyskowski M, Mundy AR, Vivian GC. Spinning top urethra: not a normal variant. Radiology. 1988;168:147–50.
Kutlu O, Koksal IT, Guntekin E, Kukul E. Role of spinning top urethra in dysfunctional voiding. Scand J Urol Nephrol. 2010;44:32–7.
• Lee C-L, Chen S-F, Jiang Y-H, Kuo H-C. Effect of videourodynamic subtypes on treatment outcomes of female dysfunctional voiding. Int Urogynecology J. 2022;33:1283–91. How different urodynamic patterns may impact our understanding and outcomes of dysfunctional voiding
Funding
No funding was received for this article.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Joanna Marantidis and Rachael D. Sussman declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Marantidis, J., Sussman, R.D. How to Diagnose Dysfunctional Voiding. Curr Bladder Dysfunct Rep 19, 76–82 (2024). https://doi.org/10.1007/s11884-024-00735-9
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11884-024-00735-9