Abstract
Background
In the last decades, the studies performed on the field of endothelial dysfunction confirmed the fact that the starting point of this pathology is the inflammation. Several inflammatory biomarkers had been discovered and studied, ones showing systemic inflammation, and others being more specific biomarkers and showing the local inflammation. Pentraxin-3 (PTX3) is a new inflammatory biomarker, from the same family as high-selectivity C-reactive protein (hs-CRP), but it is a more specific biomarker, due to its local production: the endothelial cells and not the liver like in the case of hs-CRP.
Aims
Several antihypertensive classes of drugs seem to have a positive impact on reducing the local endothelial inflammation, beyond their effect of lowering the blood pressure, so this study aims to analyze the effect of candesartan on the two inflammatory biomarkers: PTX3 and CRP, compared with other antihypertensive drugs, in hypertensive patients with endothelial dysfunction.
Methods
A total of 365 patients were included in the study: 127 hypertensive patients were under treatment with candesartan, 134 patients were under treatment with other hypotensive medication (beta blockers, calcium channel blockers, and diuretics), both groups with controlled values of blood pressure, and 104 were normotensive persons. Classical methods of assessing the endothelial function were correlated with these biochemical markers.
Results
The patients treated with candesartan had a significant lower value of PTX3 and hs-CRP, compared with those under treatment with other antihypertensive medication as follows: PTX3: 0.61 ± 0.49 vs 0.95 ± 1.04 ng/ml, P = 0.006 and hs-CRP: 0.19 ± 0.20 vs 0.20 ± 0.22 mg/dl, P = 0.54.
Conclusions
Candesartan decreases PTX3 and hs-CRP plasma levels more powerful than other classes of antihypertensive drugs (beta blockers, calcium channel blockers, and diuretics), so we may assume that candesartan has a more potent action in reversing endothelial dysfunction and that it offers a higher vascular protection than other classes of antihypertensive drugs. We are suggesting that this new biochemical marker, PTX3, might be better and more specific marker for endothelial dysfunction, than hs-CRP.




Similar content being viewed by others
References
Brandes RP (2014) Endothelial dysfunction and hypertension. Hypertension 64:924–928
Andor M, Tomescu M (2005) Endothelial dysfunction—methods of assessment and pharmacological approach in cardiovascular diseases. TMJ 55(1):58–63
Widmer RJ, Lerman A (2014) Endothelial dysfunction and cardiovascular disease. Global Cardiol Sci Pract 2014(3):291–308
Szmitko PE, Wang CH, Weisel RD et al (2003) New markers of inflammation and endothelial cell activation part I. Circulation 108:1917–1923
Szmitko PE, Wang CH, Weisel RD et al (2003) Biomarkers of vascular disease linking inflammation to endothelial activation part II. Circulation 108:2041–2048
Inoue K, Kodama T, Daida H (2012) Pentraxin 3: a novel biomarker for inflammatory cardiovascular disease. Int J Vasc Med (Hindawi Publishing Corporation ID 657025)
Lech M, Rommele C, Anders HJ (2013) Pentraxins in nephrology: C-reactive protein, serum amyloid P and pentraxin-3. Nephrol Dial Transplant 28:803–811
Kume N, Mitsuoka H, Hayashida K, Tanaka M (2011) Pentraxin 3 as a biomarker for acute coronary syndrome: comparison with biomarkers for cardiac damage. J Cardiol 58:38–45
Jenny NS, Blumenthal RS, Kronmal RA, Rotter JI, Siscovick DS, Psaty BM (2014) Associations of pentraxin 3 with cardiovascular disease: the multi-ethnic study of atherosclerosis. J Thromb Hemost 12:999–1005
Matsubara J, Sugiyama S, Nozaki T, Sugamura K, Konishi M et al (2011) Pentraxin 3 is a new inflammatory marker correlated with left ventricular diastolic dysfunction and heart failure with normal ejection fraction. J Am Coll Cardiol 57:861–869
Tousoulis D, Antoniades C, Stefanadic C (2005) Evaluating endothelial function in humans: a guide to invasive and non invasive techniques. Heart 91:553–558
Touboul PJ, Hennerici MG, Meairs S et al (2012) Mannheim carotid intima-media thickness and plaque consensus (2004–2006–2011). An update on behalf of the advisory board of the 3rd, 4th and 5th watching the risk symposia, at the 13th, 15th and 20th European stroke conferences, Mannheim, 2004, Brussels, 2006, and Hamburg, 2011. Cerebrovasc Dis 34(4):290–296
Husain A, Azim S, Mitra M, Bhasin PS (2011) A review on candesartan: pharmacological and pharmaceutical profile. J Appl Pharm Sci 10:12–17
Buda V, Andor M, Cristescu C, Voicu M, Suciu L, Suciu M, Tomescu M (2014) Blockers of the RAA system: perindopril and candesartan and their implication on endothelial dysfunction. Med Evol 3:509–517
Burnier M (2001) Angiotensin II type 1 receptor blockers. Circulation 103:904–912
Miura S, Karnik SS, Saku K (2011) Angiotensin II type 1 receptor blockers: class effects versus molecular effects. J Renin–Angiotensin–Aldosterone Syst. doi:10.1177/1470320310370852
Munger MA (2011) Use of angiotensin receptor blockers in cardiovascular protection. Curr Evid Future Dir P&T 36:1
Michel MC, Foster C, Brunner HR, Liu L (2013) A systematic comparison of the properties of clinically used angiotensin II type 1 receptor antagonists. Pharmacol Rev 65:809–848
Hajjar I, Hart M, Milberg W et al (2009) The rationale and design of the antihypertensives and vascular, endothelial, and cognitive function (AVEC) trial in elderly hypertensives with early cognitive impairment: role of the renin angiotensin system inhibition. BMC Geriatr 9:48
Nishida Y, Takahashi Y, Nakayama T et al (2010) Effect of candesartan monotherapy on lipid metabolism in patients with hypertension: a retrospective longitudinal survey using data from electronic medical records. Cardiovasc Diabetol 9:38
Zorad S, Dou JT, Benicky J, Hutanu D et al (2006) Long-term angiotensin II AT1 _receptor inhibition produces adipose tissue hypotrophy accompanied by increased expression of adiponectin and PPARγ. Eur J Pharmacol 552:112–122
Doggrell SA (2004) Telmisartan—killing two birds with one stone. Pharmacotherapy 5:2397–2400
Kitamura N, Takahashi Y, Yamadate S, Asai S (2007) Angiotensin II receptor blockers decreased blood glucose levels: a longitudinal survey using data from electronic medical records. Cardiovasc Diabetol 6:26
Kwang KK, Jeong JA et al (2003) Pleiotropic effects of ang II receptor blocker in hypertensive patients. J Am Coll Cardiol 42(5):905–910
Lithell H, Hansson L, Skoog I et al (2003) SCOPE study groups: the study on cognitive and prognosis in the elderly: principal results of a randomized double-blind interventional trial. Hypertension 21:875–886
Schrader J, Luders S, Kulschewski A et al (2003) Acute candesartan cilexitil therapy in stroke survivors study group: the-ACCESS study: evaluation of acute candesartan cilexitil therapy in stroke survivors. Stroke 34:1699–1703
Pfeffer MA, Swedberg K et al (2016) CHARM investigators and committees: effect of candesartan on mortality and morbidity in patients with chronic heart failure: the CHARM-overall programme. Lancet 362:759–766
Yilmaz MI, Carreo JJ, Martin-Ventura JL et al (2010) Combined therapy with renin–angiotensin system and calcium channel blockers in type 2 diabetic hypertensive patients with proteinuria: effects on soluble TWEAK, PTX3 and flow-mediated dilatation. Clin J Am Soc Nephrol 5(7):1174–1181
Buda V, Andor M, Cristescu C et al (2016) The influence of perindopril on PTX3 plasma levels in hypertensive patients with endothelial dysfunction. Farmacia 64(3):382–389
Yano Y, Matsuda S, Hatakeyama K et al (2010) Plasma pentraxin 3 but not high-sensitivity C-reactive protein, is a useful inflammatory biomarker for predicting cognitive impairment in elderly hypertensive patients. J Gerontol A Biol Sci Med Sci 65(5):547–552
Yilmaz MI, Axelsson J, Sonmez A et al (2009) Effect of renin angiotensin system blockade on pentraxin 3 levels in type-2 diabetic patients with proteinuria. Clin J Am Soc Nephrol 4(3):535–541
Unlu M, Karaman M, Ahmet SA et al (2013) The comparative effects of valsartan and amlodipine on vascular microinflammation in newly diagnosed hypertensive patients. Clin Exp Hypertens 35(6):418–423
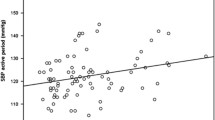
Parlak A, Aydogan U, Iyisoy A et al (2012) Elevated pentraxin-3 levels are related to blood pressure levels in hypertensive patients: an observational study. Anatol J Cardiol 12(4):298–304
Carrizzo A, Lenzi P, Procaccini C et al (2015) Pentraxin 3 induces vascular endothelial dysfunction through a P-selectin/matrix metalloproteinase-1 pathway. Circulation 131(17):1495–1505. doi:10.1161/CIRCULATIONAHA
Yasunaga T, Ikeda S, Koga S et al (2014) Plasma pentraxin 3 is a more potent predictor of endothelial dysfunction than high-sensitive C-reactive protein. Int Heart J 55(2):160–164
Acknowledgements
This work was supported by the Grant PII-C4-TC-2016-16441-09 offered by the “Victor Babes” University of Medicine and Pharmacy of Timisoara, Romania.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
All procedures performed in this study with human participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. This study has been approved by the Ethical Committee of the “Victor Babes” University of Medicine and Pharmacy, Timisoara, Romania (no. 7/2016).
Conflict of interest
None.
Rights and permissions
About this article
Cite this article
Buda, V., Andor, M., Cristescu, C. et al. The effect of candesartan on pentraxin-3 plasma levels as marker of endothelial dysfunction in patients with essential arterial hypertension. Ir J Med Sci 186, 621–629 (2017). https://doi.org/10.1007/s11845-017-1580-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11845-017-1580-5