Abstract
Background
Physical activity (PA) can play an important role in optimizing metabolic/bariatric surgery (MBS) outcomes. However, many MBS patients have difficulty increasing PA, necessitating the development of theory-driven counseling interventions. This study aimed to (1) assess the feasibility and acceptability of the TELEhealth BARIatric behavioral intervention (TELE-BariACTIV) trial protocol/methods and intervention, which was designed to increase moderate-to-vigorous intensity physical activity (MVPA) in adults awaiting MBS and (2) estimate the effect of the intervention on MVPA.
Methods
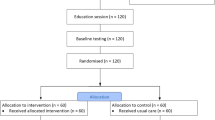
This trial used a repeated single-case experimental design. Twelve insufficiently active adults awaiting MBS received 6 weekly 45-min PA videoconferencing counseling sessions. Feasibility and acceptability data (i.e., refusal, recruitment, retention, attendance, and attrition rates) were tracked and collected via online surveys, and interviews. MVPA was assessed via accelerometry pre-, during, and post-intervention.
Results
Among the 24 patients referred to the research team; five declined to participate (refusal rate = 20.8%) and seven were ineligible or unreachable. The recruitment rate was 1.2 participants per month between 2021–09 and 2022–07. One participant withdrew during the baseline phase, and one after the intervention (retention rate = 83.3%). No participant dropouts occurred during the intervention and 98.6% of sessions were completed. Participants’ anticipated and retrospective acceptability of the intervention was 3.2/4 (IQR, 0.5) and 3.0/4 (IQR, 0.2), respectively. There was a statistically significant increase in MVPA [Tau-U = 0.32(0.11; 0.51)] from pre- to post-intervention.
Conclusion
Despite a low recruitment rate, which could be explained by circumstances (COVID-19 pandemic), results support feasibility, acceptability, and preliminary efficacy of the TELE-Bari-ACTIV intervention for increasing MVPA in patients awaiting MBS.
Graphical Abstract

Similar content being viewed by others
Data Availability
The R syntax for main analyses is provided on the Open Sciences Framework (https://osf.io/vpmzf/). Raw MVPA, light PA, sedentary time, daily steps, and pain score data are available in Supplemental Files. Other data described in the manuscript and code book will be made available on request pending application.
References
Perdomo CM, Cohen RV, Sumithran P, et al. Contemporary medical, device, and surgical therapies for obesity in adults. Lancet. 2023;401(10382):1116–30.
King WC, Chen JY, Bond DS, Belle SH, Courcoulas AP, Patterson EJ, et al. Objective assessment of changes in physical activity and sedentary behavior: pre-through 3 years post-bariatric surgery. Obesity (Silver Spring). 2015;23(6):1143–50.
Reis Barbosaa C, Verlengiaa R, Vilela Ribeiroa A, Marques de Oliveira M, Harley Crisp C. Changes in physical activities patterns assessed by accelerometry after bariatric surgery: a systematic review and meta-analysis. Obesity Med. 2019;13:6–12.
Bellicha A, van Baak MA, Battista F, Beaulieu K, Blundell JE, Busetto L, et al. Effect of exercise training before and after bariatric surgery: a systematic review and meta-analysis. Obes Revity reviews : An Official J Int Assoc Study Obesity. 2021;22(Suppl 4): e13296.
Schurmans G, Caty G, Reychler G. Is the peri-bariatric surgery exercise program effective in adults with obesity: a systematic review. Obes Surg. 2022;32(2):512–35.
Boppre G, Diniz-Sousa F, Veras L, Oliveira J, Fonseca H. Does exercise improve the cardiometabolic risk profile of patients with obesity after bariatric surgery? A systematic review and meta-analysis of randomized controlled trials. Obes Surg. 2022;32(6):2056–68.
Zabatiero J, Hill K, Gucciardi DF, Hamdorf JM, Taylor SF, Hagger MS, Smith A. Beliefs, barriers and facilitators to physical activity in bariatric surgery candidates. Obes Surg. 2016;26(5):1097–109.
Toft BS, Uhrenfeldt L. The lived experiences of being physically active when morbidly obese: a qualitative systematic review. Int J Qual Stud Health Well-being. 2015;10:28577.
Bond D. Introducing physical activity and reducing sedentary behaviours in people living with obesity before and after metabolic and bariatric surgerys. In: disorders IFSO, editor. Consensus on definitions and clinical practice guidelines for patients considering metabolic-bariatric surgery 2023. 2023. p. 20–3 https://bariatriarf.ru/wp-content/uploads/2023/10/IFSO-CONSENSUS-CONFERENCE-2023-BOOK.pdf.
Samdal GB, Eide GE, Barth T, Williams G, Meland E. Effective behaviour change techniques for physical activity and healthy eating in overweight and obese adults; systematic review and meta-regression analyses. The Int J Behav Nutrition Phys Activity. 2017;14(1):42.
Gourlan M, Bernard P, Bortolon C, Romain AJ, Lareyre O, Carayol M, et al. Efficacy of theory-based interventions to promote physical activity. A meta-analysis of randomised controlled trials. Health Psych Rev. 2015:1–17. https://doi.org/10.1080/17437199.2014.981777
Prestwich A, Webb TL, Conner M. Using theory to develop and test interventions to promote changes in health behaviour: evidence, issues, and recommendations. Curr Opin Psychol. 2015;5:1–5.
Bond D. Bari-Active: A preoperative intervention to increase physical activity. Obes Surg. 2011;21(8):1042.
Bond DS, Thomas JG, Vithiananthan S, Unick J, Webster J, Roye GD, et al. Intervention-related increases in preoperative physical activity are maintained 6-months after bariatric surgery: results from the bari-active trial. Int J Obes (Lond). 2017;41(3):467–70.
Kairy D, Lehoux P, Vincent C, Visintin M. A systematic review of clinical outcomes, clinical process, healthcare utilization and costs associated with telerehabilitation. Disabil Rehabil. 2009;31(6):427–47.
Patel ML, Wakayama LN, Bass MB, Breland JY. Motivational interviewing in eHealth and telehealth interventions for weight loss: a systematic review. Prev Med. 2019;126: 105738.
Hutchesson MJ, Rollo ME, Krukowski R, Ells L, Harvey J, Morgan PJ, et al. eHealth interventions for the prevention and treatment of overweight and obesity in adults: a systematic review with meta-analysis. Obesity Rev An Official J Int Assoc Study Obesity. 2015;16(5):376–92.
Hakala S, Rintala A, Immonen J, Karvanen J, Heinonen A, Sjogren T. Effectiveness of technology-based distance interventions promoting physical activity: systematic review, meta-analysis and meta-regression. J Rehabil Med. 2017;49(2):97–105.
Cotie LM, Prince SA, Elliott CG, Ziss MC, McDonnell LA, Mullen KA, et al. The effectiveness of eHealth interventions on physical activity and measures of obesity among working-age women: a systematic review and meta-analysis. Obesity Rev Official J Int Assoc Study Obesity. 2018;19(10):1340–58.
Messiah SE, Sacher PM, Yudkin J, Ofori A, Qureshi FG, Schneider B, et al. Application and effectiveness of eHealth strategies for metabolic and bariatric surgery patients: a systematic review. Digit Health. 2020;6:2055207619898987.
Coldebella B, Armfield NR, Bambling M, Hansen J, Edirippulige S. The use of telemedicine for delivering healthcare to bariatric surgery patients: a literature review. J Telemed Telecare. 2018;24(10):651–60.
Bradley LE, Forman EM, Kerrigan SG, Goldstein SP, Butryn ML, Thomas JG, et al. Project HELP: a remotely delivered behavioral intervention for weight regain after bariatric surgery. Obes Surg. 2017;27(3):586–98.
Mundi MS, Lorentz PA, Grothe K, Kellogg TA, Collazo-Clavell ML. Feasibility of smartphone-based education modules and ecological momentary assessment/intervention in pre-bariatric surgery patients. Obes Surg. 2015;25(10):1875–81.
Hayotte M, Iannelli A, Negre V, Pradier C, Therouanne P, Fuch A, et al. Effects of technology-based physical activity interventions for women after bariatric surgery: study protocol for a three-arm randomised controlled trial. BMJ Open. 2021;11(7): e046184.
Lurbe Puerto K, Bruzzi M, Rives-Lange C, Poghosyan T, Bretault M, Chatellier G, et al. MyGood Trip, a telemedicine intervention for physical activity recovery after bariatric surgery: randomized controlled trial. JMIR Form Res. 2023;7: e26077.
Czajkowski SM, Powell LH, Adler N, Naar-King S, Reynolds KD, Hunter CM, et al. From ideas to efficacy: the ORBIT model for developing behavioral treatments for chronic diseases. Health Psychol. 2015;34(10):971–82.
Tate RL, Perdices M, Rosenkoetter U, Shadish W, Vohra S, Barlow DH, et al. The single-case reporting guideline in behavioural interventions (SCRIBE) 2016 statement. J Clin Epidemiol. 2016;73:142–52.
Perdices M, Tate RL. Single-subject designs as a tool for evidence-based clinical practice: are they unrecognised and undervalued? Neuropsychol Rehabil. 2009;19(6):904–27.
Clanchy KM, Tweedy SM, Tate RL, Sterling M, Day MA, Nikles J, Ritchie C. Evaluation of a novel intervention to improve physical activity for adults with whiplash associated disorders: Protocol for a multiple-baseline, single case experimental study. Contemp Clin Trials Commun. 2019;16: 100455.
Caneiro JP, Smith A, Linton SJ, Moseley GL, O’Sullivan P. How does change unfold? an evaluation of the process of change in four people with chronic low back pain and high pain-related fear managed with cognitive functional therapy: a replicated single-case experimental design study. Behav Res Ther. 2019;117:28–39.
Kwasnicka D, Dombrowski SU, White M, Sniehotta FF. N-of-1 study of weight loss maintenance assessing predictors of physical activity, adherence to weight loss plan and weight change. Psychol Health. 2017;32(6):686–708.
Lapointe J, Comtois AS, Romain AJ, Bernard P. The Transtheoretical model’s processes of change in the heart of a physical activity intervention: a series of n-of-1. Psychol Sport Exerc. 2023;67: 102430.
Quilez-Orden A, Ferreres-Galan V, Osma J. Feasibility and clinical usefulness of the unified protocol in online group format for bariatric surgery candidates: study protocol for a multiple baseline experimental design. Int J Environ Res Public Health. 2020;17(17). https://doi.org/10.3390/ijerph17176155
Grammatikopoulou MG, Gkouskou KK, Gkiouras K, Bogdanos DP, Eliopoulos AG, Goulis DG. The niche of n-of-1 trials in precision medicine for weight loss and obesity treatment: back to the future. Current Nutrition Rep. 2022;11(2):133–45.
Baillot A, St-Pierre M, Lapointe J, Bernard P, Bond D, Romain AJ, et al. Acceptability and feasibility of the telehealth bariatric behavioral intervention to increase physical activity: protocol for a single-case experimental study. JMIR Res Protoc. 2022;11(9): e39633.
Kazdin AE. Single-case research designs: methods for clinical and applied settings. 2nd ed. 2011. p. xi þ 452.
Deci EL, Ryan RM. Intrinsic motivation and self-determination in human behaviour. New York: Plenum Press; 1985.
Bandura A. Social learning theory: Englewood Cliffs. Nj: Prentice-Hall; 1977. p. 247.
Sekhon M, Cartwright M, Francis JJ. Acceptability of healthcare interventions: an overview of reviews and development of a theoretical framework. BMC Health Serv Res. 2017;17(1):88.
LeRouge C, Garfield M, Hevner A. Quality attributes in telemedicine video conferencing. In: Proceedings of the 35th Annual Hawaii International Conference on System Sciences (HICSS-35i02). 2002. https://doi.org/10.1109/HICSS.2002.994132.
Trost S, McIver K, Tate R. Conducting accelerometer-based activity measurements in field based research. Med Sci Sports Exerc. 2005;37:S531–43.
King WC, Li J, Leishear K, Mitchell JE, Belle SH. Determining activity monitor wear time: an influential decision rule. J Phys Act Health. 2011;8(4):566–80.
Freedson PS, Melanson E, Sirard J. Calibration of the Computer Science and Applications. Inc accelerometer Med Sci Sports Exerc. 1998;30(5):777–81.
Tate RL, Rosenkoetter U, Wakim D, Sigmundsdottir L, Doubleday J, Logher T, et al. In: Tate RL, et al., editors. The risk of bias in N-Of-1 trials (RoBiNT) scale: an expanded manual for the critical appraisal of single-case report, vol. 2015. Sydney, Australia; 2015. p. 101.
Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–13.
Spitzer RL, Kroenke K, Williams JB, Lowe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006;166(10):1092–7.
Bauer-Staeb C, Kounali DZ, Welton NJ, Griffith E, Wiles NJ, Lewis G, et al. Effective dose 50 method as the minimal clinically important difference: evidence from depression trials. J Clin Epidemiol. 2021;137:200–8.
Hays RD, Morales LS. The RAND-36 measure of health-related quality of life. Ann Med. 2001;33(5):350–7.
Bond DS, Thomas JG, King WC, Vithiananthan S, Trautvetter J, Unick JL, et al. Exercise improves quality of life in bariatric surgery candidates: results from the bari-active trial. Obesity (Silver Spring). 2015;23(3):536–42.
Warkentin LM, Majumdar SR, Johnson JA, Agborsangaya CB, Rueda-Clausen CF, Sharma AM, et al. Weight loss required by the severely obese to achieve clinically important differences in health-related quality of life: two-year prospective cohort study. BMC Med. 2014;12:175.
Stewart AL, Greenfield S, Hays RD, Wells K, Rogers WH, Berry SD, et al. Functional status and well-being of patients with chronic conditions. Results from the medical outcomes study. JAMA. 1989;262(7):907–13.
Wyrwich KW, Tierney WM, Babu AN, Kroenke K, Wolinsky FD. A comparison of clinically important differences in health-related quality of life for patients with chronic lung disease, asthma, or heart disease. Health Serv Res. 2005;40(2):577–91.
Bush K, Kivlahan DR, McDonell MB, Fihn SD, Bradley KA. The AUDIT alcohol consumption questions (AUDIT-C): an effective brief screening test for problem drinking Ambulatory Care Quality Improvement Project (ACQUIP). Alcohol Use Disorders Identification Test. Arch Intern Med. 1998;158(16):1789–95.
Bull FC, Maslin TS, Armstrong T. Global physical activity questionnaire (GPAQ): nine country reliability and validity study. J Phys Act Health. 2009;6(6):790–804.
Parker RI, Vannest KJ, Davis JL, Sauber SB. Combining nonoverlap and trend for single-case research: Tau-U. Behav Ther. 2011;42(2):284–99.
Bulte I, Onghena P. Randomization tests for multiple-baseline designs: an extension of the SCRT-R package. Behav Res Methods. 2009;41(2):477–85.
Wilbert J, Lueke T. Analyzing single-case data with R and scan. 2021. https://jazznbass.github.io/scan-Book/.
Lane JD, Gast DL. Visual analysis in single case experimental design studies: brief review and guidelines. Neuropsychol Rehabil. 2014;24(3–4):445–63.
King WC, Hsu JY, Belle SH, Courcoulas AP, Eid GM, Flum DR, et al. Pre- to postoperative changes in physical activity: report from the longitudinal assessment of bariatric surgery-2. Surgery Obesity Related Dis. 2012;8(5):522–32.
Baillot. A, Bernard P, Eddine JN, Thomas JG, Schumacher L, Papasavas PK, et al. Associations of weather and air pollution with objective physical activity and sedentary time before and after bariatric surgery: a secondary analysis of a prospective cohort study. medRxiv. 2023. https://doi.org/10.1101/2023.03.22.23287589.
Baillot A, Boissy P, Tousignant M, Langlois MF. Feasibility and effect of in-home physical exercise training delivered via telehealth before bariatric surgery. J Telemed Telecare. 2017;23(5):529–35.
Gonzalez-Cutre D, Megias A, Beltran-Carrillo VJ, Cervello E, Spray CM. Effects of a physical activity program on post-bariatric patients: a qualitative study from a self-determination theory perspective. J Health Psychol. 2020;25(10–11):1743–54.
Roddy MK, Pfammatter AF, Mayberry LS. Optimizing adaptive stepped-care interventions to change adults’ health behaviors: a systematic review. J Clin Transl Sci. 2023;7(1): e190.
Conroy MB, Yang K, Elci OU, Gabriel KP, Styn MA, Wang J, et al. Physical activity self-monitoring and weight loss: 6-month results of the SMART trial. Med Sci Sports Exerc. 2011;43(8):1568–74.
Gul RB, Ali PA. Clinical trials: the challenge of recruitment and retention of participants. J Clin Nurs. 2010;19(1–2):227–33.
Parkinson B, Meacock R, Sutton M, Fichera E, Mills N, Shorter GW, et al. Designing and using incentives to support recruitment and retention in clinical trials: a scoping review and a checklist for design. Trials. 2019;20(1):624.
Treweek S, Pitkethly M, Cook J, Fraser C, Mitchell E, Sullivan F, et al. Strategies to improve recruitment to randomised trials. Cochrane Database Syst Rev. 2018;2(2):MR000013.
Houghton C, Dowling M, Meskell P, Hunter A, Gardner H, Conway A, et al. Factors that impact on recruitment to randomised trials in health care: a qualitative evidence synthesis. Cochrane Database Syst Rev. 2020;10(10):MR000045.
Stephens S, Beyene J, Tremblay MS, Faulkner G, Pullnayegum E, Feldman BM. Strategies for dealing with missing accelerometer data. Rheum Dis Clin North Am. 2018;44(2):317–26.
Tudor-Locke C, Barreira TV, Schuna JM Jr, Mire EF, Chaput JP, Fogelholm M, et al. Improving wear time compliance with a 24-hour waist-worn accelerometer protocol in the International Study of Childhood Obesity, Lifestyle and the Environment (ISCOLE). Int J Behav Nut Phys Act. 2015;12:11.
Xu X, Tupy S, Robertson S, Miller AL, Correll D, Tivis R, Nigg CR. Successful adherence and retention to daily monitoring of physical activity: lessons learned. PLoS ONE. 2018;13(9): e0199838.
Konig LM, Allmeta A, Christlein N, Van Emmenis M, Sutton S. A systematic review and meta-analysis of studies of reactivity to digital in-the-moment measurement of health behaviour. Health Psychol Rev. 2022;16(4):551–75.
Baillot A, St-Pierre M, Bernard P, Burkhardt L, Chorfi W, Oppert JM, et al. Exercise and bariatric surgery: a systematic review and meta-analysis of the feasibility and acceptability of exercise and controlled trial methods. Obes Rev. 23(9):e13480. https://doi.org/10.1111/obr.13480.
Singh B, Olds T, Curtis R, Dumuid D, Virgara R, Watson A, et al. Effectiveness of physical activity interventions for improving depression, anxiety and distress: an overview of systematic reviews. Br J Sports Med. 2023;57(18):1203–9.
Swierz MJ, Storman D, Jasinska KW, Storman M, Staskiewicz W, Gorecka M, et al. Systematic review and meta-analysis of perioperative behavioral lifestyle and nutritional interventions in bariatric surgery: a call for better research and reporting. Surg Obes Relat Dis. 2020;16(12):2088–104.
Acknowledgements
The authors would like to thank Maxime St-Pierre, Mélanie Nadeau, Annie Quesnel, Mélissa Pelletier, and Mélanie Belley for assisting with the recruitment of participants and data collection, Karine Lavallée for conducting the interviews, Jenson Price for contributing to the intervention, and Felix-Gabriel Duval for managing the accelerometer data. Maxime St-Pierre received a scholarship grant from the Regroupement intersectoriel de recherche en santé de l’Université du Québec (RISUQ). AB and AJR are recipients of salary awards from the Fonds de recherche du Québec-Santé (FRQ-S). JB is supported by a Tier II Canada Research Chair in Physical Activity Promotion for Cancer Prevention and Survivorship.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics Approval
Ethics approval was obtained from three institutions: Quebec Heart and Lung Institute, Sacré Cœur Hospital, Montreal [Centre Intégré Universitaire de Soins et de Services de Santé (CIUSSS) du Nord-de-l’Île-de-Montréal] and Chicoutimi Hospital, Chicoutimi [CIUSSS Saguenay–Lac-Saint-Jean]. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Conflicts of Interest
AT and LB received funding from Johnson & Johnson, Medtronic, and GI Windows for studies on bariatric surgery. AT has been a consultant for Biotwin, Bausch Health, Novo Nordisk, and Eli Lilly. MFL has been a consultant for Eli Lilly, Novo Nordisk, Rhythm, and Takeda and received research funding from Merck Canada and Novo Nordisk. AT and LB are codirectors of the Research Chair in Bariatric and Metabolic Surgery at Laval University. AB, MA, PB, JL, DB, PYG, JB, PB, and AJR have no conflict of interest.
Human Rights
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Study Registration and Analytic Plan Registration
The study protocol with analytic plan was previously registered in Baillot et al. (2022). Acceptability and Feasibility of the Telehealth Bariatric Behavioral Intervention to Increase Physical Activity: Protocol for a Single-Case Experimental Study. JMIR Res Protoc, 11(9), e39633.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Key Points
1. Six weeks of physical activity (PA) tele-counseling is feasible for adults awaiting MBS.
2. Six weeks of PA tele-counseling (45 min/week) is acceptable for adults awaiting MBS.
3. A theory-based tele-counseling shows promise to increase MVPA in adults awaiting MBS.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Baillot, A., Asselin, M., Bernard, P. et al. Acceptability and Feasibility of the Telehealth Bariatric Behavioral Intervention to Increase Physical Activity Before Bariatric Surgery: A Single-Case Experimental Study (Part I). OBES SURG 34, 1639–1652 (2024). https://doi.org/10.1007/s11695-024-07161-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-024-07161-0