Abstract
Purpose
Bariatric surgery reduces mortality in patients with severe obesity and is predominantly performed in women. Therefore, an analysis of sex-specific differences after bariatric surgery in a population-based dataset from Austria was performed. The focus was on deceased patients after bariatric surgery.
Materials and Methods
The Austrian health insurance funds cover about 98% of the Austrian population. Medical health claims data of all Austrians who underwent bariatric surgery from 01/2010 to 12/2018 were analyzed. In total, 19,901 patients with 107,806 observed years postoperative were eligible for this analysis. Comorbidities based on International Classification of Diseases (ICD)-codes and drug intake documented by Anatomical Therapeutical Chemical (ATC)-codes were analyzed in patients deceased and grouped according to clinically relevant obesity-associated comorbidities: diabetes mellitus (DM), cardiovascular disease (CV), psychiatric disorder (PSY), and malignancy (M).
Results
In total, 367 deaths were observed (1.8%) within the observation period from 01/2010 to 04/2020. The overall mortality rate was 0.34% per year of observation and significantly higher in men compared to women (0.64 vs. 0.24%; p < 0.001(Chi-squared)). Moreover, the 30-day mortality was 0.19% and sixfold higher in men compared to women (0.48 vs. 0.08%; p < 0.001). CV (82%) and PSY (55%) were the most common comorbidities in deceased patients with no sex-specific differences. Diabetes (38%) was more common in men (43 vs. 33%; p = 0.034), whereas malignant diseases (36%) were more frequent in women (30 vs. 41%; p = 0.025).
Conclusion
After bariatric surgery, short-term mortality as well as long-term mortality was higher in men compared to women. In deceased patients, diabetes was more common in men, whereas malignant diseases were more common in women.
Graphical abstract

Similar content being viewed by others
Introduction
Bariatric surgery is a frequently performed procedure in patients with severe obesity with worldwide increasing numbers [1, 2]. According to the International Federation for the Surgery of Obesity and Metabolic Disorders (IFSO) survey 2016, 634,897 primary bariatric surgeries were performed worldwide, of which 2983 bariatric procedures were done in Austria [3].
Bariatric surgery was shown to lead to substantial weight-loss and to a reduction in all-cause mortality compared to controls with severe obesity [4, 5]. However, a recent study indicates that the mortality after bariatric surgery remains higher compared to the general population [6]. According to the IFSO report 2018, the proportion of female bariatric surgery candidates was 73.7% and remarkably higher compared to men [7]. There are several reasons and motivations for this inequality including psychosocial factors and a stronger desire for weight loss in women [8]. The appearance was shown to be the major motivation for women to undergo bariatric surgery, whereas in men, the medical condition is the most important driving factor [9]. Thus, men undergoing bariatric surgery tend to be older and to have more comorbidities at the time of operation compared to women [10]. Moreover, it was previously shown that male patients might have a higher early mortality rate after bariatric surgery compared to female patients [10, 11]. A study including about 10,000 patients after bariatric surgery showed sex differences regarding preoperative comorbidities and postoperative complications [10].
Potential sex-specific differences in morbidity and mortality are of major importance in daily clinical routine. However, large registry analyses with focus on sex-specific differences after bariatric surgery are rare and selection bias might be a relevant shortcoming in previous studies. Here, an analysis of about 20,000 patients with a history of bariatric surgery and a mean follow-up of more than 5 years is presented. Since medical health claims data of all Austrians are included, a relevant selection bias can be excluded. The aim was to study sex-specific differences in a large, real-world registry analysis.
Research Design and Methods
The health insurance system in Austria provides healthcare services for all residents who are assigned to one of the several health insurance funds according to their employment or province of residence. Thus, approximately 98% of all Austrians (2018; 8.9 million [12]) are covered. Data from outpatient and inpatient medical services covered by the health insurance funds are stored in the databases of the Austrian health insurance funds. These data include demographic data, reimbursed drug prescriptions based on Anatomical Therapeutic Chemical (ATC)-codes, and along with discharge dates from hospitals, primary, and secondary medical diagnosis recorded as International Classification of Disease (ICD)-codes and medical procedures recorded as MEL-codes (medical single procedure). Moreover, mortality data are recorded in these databases. Furthermore, as the database comprises accounting data of the Austrian health insurance funds, only publicly funded surgeries are included. The study protocol was approved by the ethical committee of the Medical University of Vienna (EK-Nr. 2052/2018).
Included Patients
All patients with a history of bariatric surgery performed between January 1st, 2010, and December 31st, 2018, based on the following MEL-codes were included in this study: HF220 (sleeve gastrectomy—open), HF230 (sleeve gastrectomy – laparoscopic), HF240 (gastric bypass – open), HF250 (gastric bypass – laparoscopic), HF254 (biliopancreatic diversion – open), HF255 (biliopancreatic diversion – laparoscopic), HF260 (gastric banding – open), and HF270 (gastric banding – laparoscopic).
Comorbidity Categories
Comorbidities of patients who died during the observation period were analyzed. Based on MEL-codes, ICD-codes, and drug histories (ATC-codes), patients were manually grouped according to the most common and clinically relevant obesity-associated comorbidities: diabetes mellitus, cardiovascular diseases, malignancy, and psychiatric disorders. The psychiatric disorder group comprised patients with schizophrenia, depression, alcohol abuse, drug abuse, anxiety disorders, borderline disorders, and eating disorders and/or took psychopharmacological medications used for treatment of these diseases. The diabetes group comprised patients diagnosed with all types of diabetes and/or took blood glucose-lowering medication. The malignancy group included patients diagnosed with malignant disease and/or took associated medication. Patients diagnosed with heart disease, heart failure, cardiac arrythmia, pulmonary disease, arterial/pulmonal hypertension, peripheral artery disease, and thromboembolic event and/or took related drugs were assigned to the cardiovascular disease group. Moreover, the number of days hospitalized and the number of hospitalizations pre- and postoperatively was analyzed in all deceased patients within the observation period. Normalization of the data was performed by dividing the number of days hospitalized and the number of hospitalizations by the individual observation period in years. For the analysis of the ATC-codes, the following substance classes were included: N03A – antiepileptics, N05A – antipsychotics, N05B – anxiolytics, N06A – antidepressants, N07B – drugs used in addictive disorders, M05B – drugs affecting bone structure and mineralization, M01A – anti-inflammatory and antirheumatic products (non-steroids), A10A – insulin and analogues, A10B – blood glucose-lowering drugs (excluding insulins), C02 – antihypertensives, C03 – diuretics, C04 – peripheral vasodilators, C07 – beta blocking agents, C08 – calcium channel blockers, C09 – agents acting on the renin-angiotensin system, C10 – lipid modifying agents, C10AA – statins, and C10AB – fibrates.
Sex-Specific Analysis
Mortality rates, comorbidities, number of days hospitalized, number of hospitalizations, drug intake, frequencies of different bariatric procedures, causes of deaths, and rate of revision operations in men and women were studied. Revision operations were identified by a further MEL-code of bariatric surgery recorded after the initial operation. Furthermore, an analysis of preoperative medication in men and women was performed. The overall mortality rate was calculated as the number of deaths divided by the total years of observation. Sex-specific mortality rate was calculated by division of the sex-specific numbers of death by the sex-specific years of observation.
Statistical Analysis
R (https://www.r-project.org/) was used to combine the datasets from the different institutions and to summarize the data of patients who were insured by multiple Austrian health insurances. Moreover, the ICD-, ATC-, and MEL-codes were linked with their respective lookup tables to enable manual classification of the patient’s comorbidities. Exploratory statistical analysis was performed using SPSS (IBM, version 26) and Microsoft Excel (Microsoft, 2019). Distribution of data was checked by visualization using histograms. Normal distributed data are given in mean ± standard deviation and data not normal distributed are given in median and interquartile range (IQR). Unpaired t-tests were performed for normal distributed data whereas for data not normal distributed, Mann–Whitney U-tests were used. Chi-squared tests were calculated to compare data between the different subgroups. Moreover, a logistic regression model in all patients (n = 19.901) was fitted. Survival/death were used as outcome and gender, age at index surgery, type of surgery, and medication category before the index surgery were used as explanatory variables. Due to the exploratory nature of the study, corrections for multiple testing were not implemented. Data is given as means ± standard deviation. Statistical significance level was set at p < 0.05.
Results
In total, 19,901 patients (5220 men (26%), 14,681 women (74%)) with 107,806 postoperative years of observation were eligible for this analysis. The individual observation period of each enrolled patient ranged from 1 year prior to the date of the bariatric surgery until 04/2020.
Total Group and Differences Between Men and Women (Table 1)
Median follow-up of the total cohort was 65 (IQR 38–91) months (Table 1). The age at operation was significantly higher in men compared to women (41.8 ± 12.6 vs. 40.1 ± 12.4; p < 0.001). Gastric bypass (69%) was the most frequently performed procedure in men and women but with a higher proportion in women (65 vs. 70%; p < 0.001). Overall, sleeve gastrectomy was recorded in 24% and significantly more often performed in men compared to women (30 vs. 22%; p < 0.001). The rate of revision operations was significantly higher in women compared to men (3.4 vs. 2.8%; p = 0.04). In patients with revision surgery, sleeve gastrectomy (40%) was the most frequently performed initial type of procedure followed by gastric banding (34%) and gastric bypass (25%). After the revision surgery, gastric bypass was the most frequently performed type of surgery with 79% followed by sleeve gastrectomy (11%) and gastric banding (10%).
Analysis of Drug Intake Based on ATC-Codes in the Total Group (Table 2)
Medication intake during the year before the bariatric surgery was analyzed. Men were treated significantly more frequently with glucose-lowering drugs including insulin, antihypertensive agents, and lipid-lowering drugs, whereas the intake of antidepressants was significantly higher in women (Table 2).
Characterization of Deceased Patients (Table 3 )
A total of 367 (1.8%) patients died during the observation period with a significantly higher proportion of men compared to women (3.4 vs. 1.3%; p < 0.001) (Table 1). The overall mortality was 0.34% per year of observation and was significantly higher in men compared to women (0.64 vs. 0.24%, p < 0.001 (Chi-squared)). Moreover, the proportion of patients who deceased on the day of the bariatric procedure was 0.12% and significantly higher in men compared to women (0.29 vs. 0.05%, p < 0.001) (Table 1). The postoperative 30-day mortality was 0.19% and sixfold higher in men compared to women (0.48 vs. 0.08%, p < 0.001). Overall, 330 deaths were observed after 30 days postoperative, with a higher proportion of men compared to women (2.9 vs. 1.2%, p < 0.001). The overall mortality rate per year of observation excluding the 30-day mortality was 0.31% with a more than twofold higher mortality rate in men (0.55 vs. 0.22%). Five patients (1 man, 4 women, p = 0.754) died between day 31 and day 60. Gastric bypass surgery was the most frequently performed procedure in all patients deceased (64%) followed by sleeve gastrectomy (29%) and gastric banding (6%), with no sex-specific differences.
Mean age at operation in deceased patients and mean age at death were not significantly different between men and women. Detailed demographics of deceased subjects are given in Table 3. In total, 197 of 367 patients (54%) died in hospital with no significant sex-specific difference. For these patients, potential causes of deaths, based on the ICD-codes recorded on or around the date of the death, are given in Table 4. No sex-specific differences were observed (p = 0.409).
The analysis of the frequency of hospitalizations as well as the number of days hospitalized showed no sex-specific differences neither preoperatively nor postoperatively.
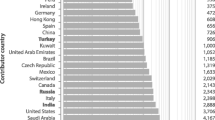
Underlying comorbidities of all 367 patients deceased are given in Fig. 1. Cardiovascular diseases (total 82%, men 84%, women 80%; p = 0.332) and psychiatric disorders (total 55%, men 51%, women 58%; p = 0.147) were the most common comorbidities with no significant sex-specific differences. Malignant diseases (total 36%, men 30%, women 41%; p = 0.025) were significantly more observed in women, whereas diabetes (total 38%, men 43%, women 33%; p = 0.034) was more frequent in men. A total of 93% of all patients deceased had at least one comorbidity with no sex-specific difference regarding the number of comorbidities (p = 0.909). In 33 deceased patients (9%; men 17, women 16; men vs. women; p = 0.668), no definitive comorbidity could be identified. However, all available data on demographics including sex, age, type of bariatric procedure, and date of death were analyzed in these patients.
The logistic regression analysis demonstrated that men (odds ratio 2.4), patients with a higher age at the index surgery (odds ratio 1.1), and patients with preoperative intake of antihypertensive agents (odds ratio 1.6) had a significantly higher risk for death. Preoperative intake of lipid lowering drugs (odds ratio 0.6) and preoperative intake of non-steroidal antirheumatics (odds ratio 0.5) was associated with a significantly lower risk for death.
Discussion
This analysis of medical insurance claims data shows that (i) short-term mortality as well as long-term mortality after bariatric surgery is significantly higher in men compared to women and (ii) that in patients deceased after bariatric surgery, cardiovascular and psychiatric comorbidities were the most common comorbidities with no sex-specific differences. Moreover, in deceased patients, the incidence of diabetes was higher in men, whereas women suffered more frequently from malignancies. Our results highlight the importance of an individualized, sex-specific preoperative counseling and postoperative follow-up of patients after bariatric surgery.
Several studies demonstrated the favorable outcomes after bariatric surgery including a reduction in overall-mortality [4, 5, 13] reduced hospitalization rates and reduced comorbidities [14]. On the contrary, other observations showed an increased risk of drug- and alcohol-associated mortality [15] and a higher suicide risk after metabolic surgery [16]. However, sex-specific outcomes are not comprehensively analyzed but might be of major importance as the barrier to undergo bariatric surgery is higher in men compared to women, which is reflected by the predominance of females among bariatric surgery candidates [7].
The 30-day mortality and 60-day mortality in our analysis was 0.19% and 0.21%, respectively. This is lower compared to others that reported a 30-day mortality rate of up to 1.1%, depending on the procedure performed [17, 18] and a 60-day mortality rate following bariatric surgery of 0.25% [19]. However, recent studies described a lower 30-day mortality with 0.1% [20]. The 30-day mortality in our analysis over the observation period was stable (range 0.1–0.3%) with almost constantly higher mortality in men compared to women. Sex-specific mortality in men (0.64% per year of observation) was more than two times higher compared to women (0.24%). These results are consistent with the findings from an analysis showing that male sex, higher age, higher body mass index, and psychiatric disorders are linked to higher mortality following bariatric surgery [21].
It was shown that men are more often suffering from comorbidities and have a higher body mass index at the time of the operation compared to women [10]. Also, in our study, the intake of cardiovascular and glucose-lowering medication in the year before the operation was higher in men (Table 2). The higher incidence of diabetes in men observed in this analysis is in line with the literature [10] and of major interest, since it was shown that preoperative diabetes mellitus and hypertension are associated with higher mortality risks in patients with bariatric surgery [19]. However, the overall preoperative intake of antidiabetics and insulin, based on ATC-codes, was 8% and might indicate a low rate of diabetics in this cohort. Nevertheless, this low rate might be an underestimation of the diabetes rate, since only reimbursed drug prescriptions were available. Moreover, the higher age at the operation in men in this analysis is in line with findings from other studies [10, 22] and might also explain the higher postoperative mortality rates in males.
One other potential explanation for the overall better outcomes in women after bariatric surgery might be that the adaptation on protein catabolism occurring during the third trimester of pregnancy [23] might prepare women better for the state of catabolism after bariatric surgery. However, the rate of revision operation in our analysis was significantly higher in women compared to men (3.4 vs. 2.8%, p = 0.04). This finding is in line with the literature showing that revision surgery rates in women are remarkably higher compared to men [8, 24]. Nevertheless, the overall revision rate observed in our analysis was lower compared to other studies [25].
The detailed analysis of all deceased patients with a history of bariatric surgery in this study revealed that cardiovascular comorbidities and psychiatric disorders were the most common findings with no sex-specific differences. This is of special interest since it was shown that depression disorder and coronary heart disease are linked to higher postoperative mortality [21, 26]. Moreover, the increased risk of major depression disorders following bariatric surgery [27] might provide one explanation for the high percentage of psychiatric comorbidities observed in our analysis. Regarding sex-specific disease risk, it was shown that women are more likely to have mental health issues before bariatric surgery, whereas men have higher rates of substance abuse and cardiopulmonary diseases [22]. These findings are in line with the results of our analysis, showing that women more frequently use psychopharmacological drugs before bariatric surgery while usage of cardiovascular drugs, glucose-lowering drugs, and drugs used for treatment of addiction disorders was observed predominantly in men. Moreover, it has been shown that men exerted an unhealthier lifestyle after bariatric surgery including higher alcohol intake and a worse macronutrient intake while exceeding recommended calorie intake [28]. However, in our analysis, malignant diseases were significantly more prevalent in women compared to men. Nevertheless, a meta-analysis demonstrated a favorable effect of bariatric surgery on overall obesity-related cancer rates with greater reduction in women compared to men [29].
The pattern of different bariatric procedures observed in this study cohort is different from the worldwide reported frequencies of metabolic procedures [7], since traditionally gastric bypass is performed more frequently than sleeve gastrectomy in Austria. In addition, a sex-specific difference between the frequency of sleeve gastrectomy and gastric bypass was observed in this analysis. Sleeve gastrectomy was more frequent in men, whereas gastric bypass was performed more often in women. This is of interest, since it was shown that sleeve gastrectomy is more effective in men and gastric bypass is neutral concerning sex-specific outcomes [30]. A meta-analysis demonstrated a higher surgery-associated mortality in observational studies after gastric bypass compared to sleeve gastrectomy [25]. However, this might not explain the different mortality rates in men and women observed in this study, since gastric bypass was more commonly performed in women in the present analysis. Nevertheless, in deceased patients, no sex-specific differences regarding bariatric procedures could be observed in our analysis.
The major limitation of this study is the structure of patient’s data based on medical insurance claims data which only comprises ICD-codes, ATC-codes, and MEL-codes. Detailed information on body mass index, weight reduction or gain, metabolic parameters, and diagnoses from family doctors exceeding drug prescriptions are lacking due to the medical insurance health claims data structure. Moreover, potential coding discrepancies between the medical insurance claims data and the real disease must be considered. Furthermore, no data on suicide was available which might be a relevant information since previous studies reported increased suicide rates after bariatric surgery especially for men, underlying psychiatric disorders, and after gastric bypass surgery [16, 31].
On the other hand, the strength of this analysis is the sample size of nearly 20,000 patients with a history of bariatric surgery. Moreover, medical insurance claims data provide a real-world setting including ICD-diagnoses and MEL-codes from hospitals across the whole country as well as information on drug prescription by ATC-codes outside the hospital. As the medical health insurances in Austria are covering more than 98% of all Austrians, several types of selection biases are excluded.
Taken together, this real-world analysis showed a considerably higher sex-specific mortality in men in the first 30 days after bariatric surgery as well as a higher overall mortality rate in men compared to women. Moreover, in patients deceased after bariatric surgery, cardiovascular and psychiatric comorbidities were frequently observed, with no relevant sex-specific differences. However, diabetes rates were higher in men and malignancies were predominant in women. In conclusion, the higher age at operation in men together with a higher intake of cardiovascular drugs and antidiabetics preoperative highlight the importance of an individualized, sex-specific preoperative counseling before bariatric surgery. Further studies are warranted to evaluate if earlier timing of bariatric surgery in men might improve mortality outcomes.
References
English WJ, DeMaria EJ, Hutter MM, Kothari SN, Mattar SG, Brethauer SA, et al. American Society for Metabolic and Bariatric Surgery 2018 estimate of metabolic and bariatric procedures performed in the United States. Surg Obes Relat Dis. 2020;16(4):457–63.
Skogar M, Ahlberg J, Sundbom M. Claims to the patient insurance after bariatric surgery in Sweden 2000–2012. Surg Obes Relat Dis. 2015;11(1):201–6.
Angrisani L, Santonicola A, Iovino P, Vitiello A, Higa K, Himpens J, et al. IFSO Worldwide Survey 2016: primary, endoluminal, and revisional procedures. Obes Surg. 2018;28(12):3783–94.
Sjöström L, Narbro K, Sjöström CD, Karason K, Larsson B, Wedel H, et al. Effects of bariatric surgery on mortality in Swedish obese subjects. N Engl J Med. 2007;357(8):741–52.
Adams TD, Gress RE, Smith SC, Halverson RC, Simper SC, Rosamond WD, et al. Long-term mortality after gastric bypass surgery. N Engl J Med. 2007;357(8):753–61.
Carlsson LMS, Sjöholm K, Jacobson P, Andersson-Assarsson JC, Svensson P-A, Taube M, et al. Life expectancy after bariatric surgery in the Swedish obese subjects study. N Engl J Med. 2020;383(16):1535–43.
Welbourn R, Hollyman M, Kinsman R, Dixon J, Liem R, Ottosson J, et al. Bariatric surgery worldwide: baseline demographic description and one-year outcomes from the fourth IFSO global registry report 2018. Obes Surg. 2019;29(3):782–95.
Harreiter J, Kautzky-Willer A. Sex and gender differences in prevention of type 2 diabetes. Front Endocrinol (Lausanne). 2018;9(MAY):1–15.
Libeton M, Dixon JB, Laurie C, O’Brien PE. Patient motivation for bariatric surgery: characteristics and impact on outcomes. Obes Surg. 2004;14(3):392–8.
Stroh C, Weiner R, Wolff S, Knoll C, Manger T. Influences of Gender on complication rate and outcome after Roux-en-Y gastric bypass: data analysis of more than 10,000 operations from the German Bariatric Surgery Registry. Obes Surg. 2014;24(10):1625–33.
Buchwald H, Avidor Y, Braunwald E, Jensen MD, Pories W, Fahrbach K, et al. Bariatric surgery: a systematic review and meta-analysis. JAMA. 2004;292(14):1724–37.
Statistics Austria. Bevölkerungsstand [Internet]. Available from: https://www.statistik.at/web_de/statistiken/menschen_und_gesellschaft/bevoelkerung/volkszaehlungen_registerzaehlungen_abgestimmte_erwerbsstatistik/bevoelkerungsstand/index.html
Arterburn DE, Olsen MK, Smith VA, Livingston EH, Van Scoyoc L, Yancy WS, et al. Association between bariatric surgery and long-Term survival. JAMA - J Am Med Assoc. 2015;313(1):62–70.
Pontiroli AE, Zakaria AS, Fanchini M, Osio C, Tagliabue E, Micheletto G, et al. A 23-year study of mortality and development of co-morbidities in patients with obesity undergoing bariatric surgery (laparoscopic gastric banding) in comparison with medical treatment of obesity. Cardiovasc Diabetol. 2018;17(1):1–11.
White GE, Courcoulas AP, King WC. Drug- and alcohol-related mortality risk after bariatric surgery: evidence from a 7-year prospective multicenter cohort study. Surg Obes Relat Dis. 2019;15(7):1160–9.
Neovius M, Bruze G, Jacobson P, Sjoholm K, Johansson K, Granath F, et al. Risk of suicide and non-fatal self-harm after bariatric surgery results from two matched cohort studies. Lancet Diabetes Endocrinol. 2018;6(3):197–207.
Buchwald H, Estok R, Fahrbach K, Banel D, Sledge I. Trends in mortality in bariatric surgery: a systematic review and meta-analysis. Surgery. 2007;142(4):621–35.
Smith MD, Patterson E, Wahed AS, Belle SH, Berk PD, Courcoulas AP, et al. Thirty-day mortality after bariatric surgery: independently adjudicated causes of death in the longitudinal assessment of bariatric surgery. Obes Surg. 2011;21(11):1687–92.
Morino M, Toppino M, Forestieri P, Angrisani L, Allaix ME, Scopinaro N. Mortality after bariatric surgery: analysis of 13,871 morbidly obese patients from a National Registry. Ann Surg. 2007;246(6):1002–7.
Wiggins T, Pournaras DJ, Priestman E, Osborne A, Titcomb DR, Finlay I, et al. Effect of preoperative weight loss and baseline comorbidity on short-term complications and reoperations after laparoscopic Roux-en-Y gastric bypass in 2,067 patients. Obes Surg. 2021;31(6):2444–52.
Sakran N, Sherf-Dagan S, Blumenfeld O, Romano-Zelekha O, Raziel A, Keren D, et al. Incidence and risk factors for mortality following bariatric surgery: a nationwide registry study. Obes Surg. 2018;28(9):2661–9.
Schwartz J, Bashian C, Kushnir L, Nituica C, Slotman GJ. Variation in clinical characteristics of women versus men preoperative for laparoscopic Roux-en-Y gastric bypass: analysis of 83,059 patients. Am Surg. 2017;83(9):947–51.
Young MT, Phelan MJ, Nguyen NT. A decade analysis of trends and outcomes of male vs female patients who underwent bariatric surgery. J Am Coll Surg. 2016;222(3):226–31.
Meyer SB, Thompson C, Hakendorf P, Horwood C, McNaughton D, Gray J, et al. Bariatric surgery revisions and private health insurance. Obes Res Clin Pract. 2017;11(5):616–21.
Chang SH, Stoll CRT, Song J, Varela JE, Eagon CJ, Colditz GA. The effectiveness and risks of bariatric surgery an updated systematic review and meta-analysis, 2003–2012. JAMA Surg. 2014;149(3):275–87.
Omalu BI, Ives DG, Buhari AM, Lindner JL, Schauer PR, Wecht CH, et al. Death rates and causes of death after bariatric surgery for Pennsylvania residents, 1995 to 2004. Arch Surg. 2007;142(10):923–8 (discussion 929).
Lu CW, Chang YK, Lee YH, Kuo CS, Chang HH, Huang CT, et al. Increased risk for major depressive disorder in severely obese patients after bariatric surgery — a 12-year nationwide cohort study. Ann Med. 2018;50(7):605–12.
Kanerva N, Larsson I, Peltonen M, Lindroos AK, Carlsson LM. Sociodemographic and lifestyle factors as determinants of energy intake and macronutrient composition: a 10-year follow-up after bariatric surgery. Surg Obes Relat Dis. 2017;13(9):1572–83.
Wiggins T, Antonowicz SS, Markar SR. Cancer risk following bariatric surgery—systematic review and meta-analysis of national population-based cohort studies. Obes Surg. 2019;29(3):1031–9.
Perrone F, Bianciardi E, Benavoli D, Tognoni V, Niolu C, Siracusano A, et al. Gender influence on long-term weight loss and comorbidities after laparoscopic sleeve gastrectomy and Roux-en-Y gastric bypass: a prospective study with a 5-year follow-up. Obes Surg. 2016;26(2):276–81.
Kauppila JH, Santoni G, Tao W, Lynge E, Jokinen J, Tryggvadóttir L, et al. Risk factors for suicide after bariatric surgery in a population-based nationwide study in five Nordic countries. Ann Surg. 2020;Publish Ah(Xx):1–5.
Acknowledgements
The authors thank the members of the Pharmacoeconomics Advisory Council of the Austrian Sickness Funds for provision of the data. We wish to thank Ms. Karin Allmer for quality assurance of the database query and Mr. Ludwig Weissengruber for the organizational support in the data generation.
Funding
Open access funding provided by Medical University of Vienna.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics Approval
All procedures performed in this study involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Consent to Participate
For this type of study, formal consent is not required.
Conflict of Interest
M.K. has received research support from Sanofi, AstraZeneca, Fit for Me, and Ipsen as well as speaker and consulting fees from AstraZeneca, Novo Nordisk, Lilly, Takeda, Ipsen, Lilly, and Sanofi.
T.S. has received grant/research support from AbbVie and Roche, has been a consultant for AbbVie and Sanofi Genzyme, and has been a paid speaker for AbbVie, Roche, Sanofi, and Takeda.
The other authors declare that they have no conflict of interest.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Key points
1. Most bariatric surgery candidates were female.
2. Psychiatric comorbidities and cardiovascular comorbidities were frequently observed in patients deceased after bariatric surgery, independent of sex.
3. The preoperative intake of cardiovascular drugs and antidiabetics was higher in men, whereas psychopharmacological drugs were more frequent in women.
4. Men had a higher short-term mortality and a higher long-term mortality
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Beiglböck, H., Mörth, E., Reichardt, B. et al. Sex-Specific Differences in Mortality of Patients with a History of Bariatric Surgery: a Nation-Wide Population-Based Study. OBES SURG 32, 8–17 (2022). https://doi.org/10.1007/s11695-021-05763-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-021-05763-6