Abstract
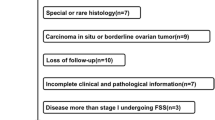
This study was performed to evaluate the oncological and reproductive outcomes of childbearing-age women treated with fertility-sparing surgery (FSS) for non-epithelial ovarian tumors in China. One hundred and forty eight non-epithelial ovarian tumor women treated with FSS between January 1, 2000 and August 31, 2015 from two medical centers in China were identified. Progression-free survival (PFS) was 88.5%, whereas overall survival (OS) was 93.9%. Univariate analysis suggested that delivery after treatment is related to PFS (P = 0.023), whereas histology significantly influenced OS. Cox regression analysis suggested that only histology was associated with PFS and OS (P < 0.05). Among the 129 women who completed adjuvant chemotherapy (ACT), none developed amenorrhea. Among the 44 women who desired pregnancy, 35 (79.5%) successfully had 51 gestations including 35 live births without birth defects. Non-epithelial ovarian tumors can achieve fulfilling prognosis after FSS and chemotherapy. Histology might be the only independent prognostic factor for PFS and OS. FSS followed by ACT appeared to have little or no effect on fertility. Meanwhile, postoperative pregnancy did not increase the PFS or OS. Use of gonadotropin-releasing hormone agonist was not beneficial for fertility.
Similar content being viewed by others
References
Ertas IE, Taskin S, Goklu R, Bilgin M, Goc G, Yildirim Y, Ortac F. Long-term oncological and reproductive outcomes of fertilitysparing cytoreductive surgery in females aged 25 years and younger with malignant ovarian germ cell tumors. J Obstet Gynaecol Res 2014; 40(3): 797–805
Sieh W, Sundquist K, Sundquist J, Winkleby MA, Crump C. Intrauterine factors and risk of nonepithelial ovarian cancers. Gynecol Oncol 2014; 133(2): 293–297
Nishio S, Ushijima K, Fukui A, Fujiyoshi N, Kawano K, Komai K, Ota S, Fujiyoshi K, Kamura T. Fertility-preserving treatment for patients with malignant germ cell tumors of the ovary. J Obstet Gynaecol Res 2006; 32(4): 416–421
Weinberg LE, Lurain JR, Singh DK, Schink JC. Survival and reproductive outcomes in women treated for malignant ovarian germ cell tumors. Gynecol Oncol 2011; 121(2): 285–289
Bryk S, Farkkila A, Butzow R, Leminen A, Heikinheimo M, Anttonen M, Riska A, Unkila-Kallio L. Clinical characteristics and survival of patients with an adult-type ovarian granulosa cell tumor: a 56-year single-center experience. Int J Gynecol Cancer 2015; 25 (1): 33–41
Yesilyurt H, Tokmak A, Guzel AI, Simsek HS, Terzioglu SG, Erkaya S, Gungor T. Parameters for predicting granulosa cell tumor of the ovary: a single center retrospective comparative study. Asian Pac J Cancer Prev 2014; 15(19): 8447–8450
Pectasides D, Pectasides E, Kassanos D. Germ cell tumors of the ovary. Cancer Treat Rev 2008; 34(5): 427–441
Tomao F, Peccatori F, Del Pup L, Franchi D, Zanagnolo V, Panici PB, Colombo N. Special issues in fertility preservation for gynecologic malignancies. Crit Rev Oncol Hematol 2016; 97: 206–219
Yang ZJ, Liu ZC, Wei RJ, Li L. An analysis of prognostic factors in patients with ovarian malignant germ cell tumors who are treated with fertility-preserving surgery. Gynecol Obstet Invest 2016; 81(1): 1–9
Slayton RE, Park RC, Silverberg SG, Shingleton H, Creasman WT, Blessing JA. Vincristine, dactinomycin, and cyclophosphamide in the treatment ofmalignant germ cell tumors of the ovary. A Gynecologic Oncology Group Study (a final report). Cancer 1985; 56(2):243–248
Williams SD, Birch R, Einhorn LH, Irwin L, Greco FA, Loehrer PJ. Treatment of disseminated germ-cell tumors with cisplatin, bleomycin, and either vinblastine or etoposide. N Engl J Med 1987; 316(23):1435–1440
Low JJ, Ilancheran A, Ng JS. Malignant ovarian germ-cell tumours. Best Pract Res Clin Obstet Gynaecol 2012; 26(3): 347–355
Mangili G, Sigismondi C, Lorusso D, Cormio G, Candiani M, Scarfone G, Mascilini F, Gadducci A, Mosconi AM, Scollo P, Cassani C, Pignata S, Ferrandina G. The role of staging and adjuvant chemotherapy in stage I Malignant ovarian germ cell tumors (MOGTs): the MITO-9 study. Ann Oncol 2017; 28(2):333–338
Pedersen-Bjergaard J, Daugaard G, Hansen SW, Philip P, Larsen SO, Rørth M. Increased risk of myelodysplasia and leukaemia after etoposide, cisplatin, and bleomycin for germ-cell tumours. Lancet 1991; 338(8763):359–363
Borovskaya TG, Timina EA, Perova AV, Pakhomova AV, Shchemerova YA, Gol’dberg VE. Pharmacological correction of etoposide ovariotoxicity. Bull Exp Biol Med 2007; 143(5):614–616
Fabbri R, Macciocca M, Vicenti R, Paradisi R, Klinger FG, Pasquinelli G, Spisni E, Seracchioli R, Papi A. Doxorubicin and cisplatin induce apoptosis in ovarian stromal cells obtained from cryopreserved human ovarian tissue. Future Oncol 2016; 12 (14):1699–1711
Swerdlow AJ, Cooke R, Bates A, Cunningham D, Falk SJ, Gilson D, Hancock BW, Harris SJ, Horwich A, Hoskin PJ, Linch DC, Lister A, Lucraft HH, Radford J, Stevens AM, Syndikus I, Williams MV; England and Wales Hodgkin Lymphoma Follow-up Group. Risk of premature menopause after treatment for Hodgkin’s lymphoma. J Natl Cancer Inst 2014; 106(9): dju207
Yoo SC, Kim WY, Yoon JH, Chang SJ, Chang KH, Ryu HS. Young girls with malignant ovarian germ cell tumors can undergo normal menarche and menstruation after fertility-preserving surgery and adjuvant chemotherapy. Acta Obstet Gynecol Scand 2010; 89(1): 126–130
Gadducci A, Lanfredini N, Tana R. Menstrual function and childbearing potential after fertility-sparing surgery and platinumbased chemotherapy for malignant ovarian germ cell tumours. Gynecol Endocrinol 2014; 30(7): 467–471
Cong J, Li P, Zheng L, Tan J. Prevalence and Risk Factors of Infertility at a Rural Site of Northern China. PLoS One 2016; 11(5): e0155563
Acknowledgements
This work was supported by grants from the National Science Foundation of China (No. 81302266) and Hubei Province Health and Family Planning Scientific Research Project (Nos. WJ2015MB003 and WJ2015Q004). The funding sources had no role in the design, analysis, interpretation, or drafting of the manuscript.
Author information
Authors and Affiliations
Corresponding authors
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Yang, B., Yu, Y., Chen, J. et al. Possibility of women treated with fertility-sparing surgery for non-epithelial ovarian tumors to safely and successfully become pregnant—a Chinese retrospective cohort study among 148 cases. Front. Med. 12, 509–517 (2018). https://doi.org/10.1007/s11684-017-0554-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11684-017-0554-3