Abstract
Background
A longstanding gender gap exists in the retention of women in academic medicine. Several strategies have been suggested to promote the retention of women, but there are limited data on impacts of interventions.
Objective
To identify what institutional factors, if any, impact women faculty’s intent to remain in academic medicine, either at their institutions or elsewhere.
Design
A survey was designed to evaluate institutional retention-linked factors, programs and interventions, their impact, and women’s intent to remain at their institutions and within academic medicine. Survey data were analyzed using non-parametric statistics and regression analyses.
Participants
Women with faculty appointments within departments of medicine recruited from national organizations and specific social media groups.
Main Measures
Institutional factors that may be associated with women’s decision to remain at their current institutions or within academic medicine.
Key Results
Of 410 surveys of women at institutions across the USA, fair and transparent family leave policies and opportunities for work-life integration showed strong associations with intent to remain at one’s institution (leave policies: OR 2.22, 95% CI 1.20–4.18, p = 0.01; work-life: OR 4.82, 95% CI 2.50–9.64, p < 0.001) and within academic medicine (leave policies: OR 2.31, 95% CI 1.09–5.03, p = 0.03; work-life: OR 4.66, 95% CI 2.04–11.36, p < 0.001). Other institutional factors associated with intent to remain in academics include peer mentorship (OR 3.16, 95% CI 1.56–6.57, p < 0.01) and women role models (OR 2.21, 95% CI 1.04–4.68, p = 0.04). Institutions helping employees recognize bias, fair compensation and provision of resources, satisfaction with mentorship, peer mentorship, and women role models within the institutions were associated with intent to remain at an institution.
Conclusions
Our findings suggest that institutional factors such as support for work-life integration, fair and transparent policies, and meaningful mentorship opportunities appear impactful in the retention of women in academic medicine.
Similar content being viewed by others
INTRODUCTION
Women now enter medical school and academic medicine at higher rates than men; however, women faculty also leave academic medicine at higher rates than faculty who are men.1,2,3 Women may leave, or intend to leave, academic medicine due to a lack of productivity,4,8 lack of mentorship,4,6,9 gender bias (in pay and promotion),5,6,7,9 work environments that are perceived as non-collaborative and oriented towards men,2,5,7,8,9 higher degree of work/family conflicts,2,6,8,9 and lack of role models effectively balancing work and family commitments.2,6,8 In the only known multi-institutional prospective study, publication-related productivity was a strong predictor of retention of women in medicine.4
A gender gap in academic medicine leadership has also been well documented, with far more men in leadership roles than women.10,11 Even though this gender gap was identified decades ago, minimal progress has been made in closing it.4 A lack of women in leadership roles may result in a lack of women role models and mentors as well as potential losses in organizational effectiveness.12 In order for academic medicine to address the gender gap in leadership in academic medicine, we must first address the leaky pipeline and confront retention.1
The literature suggests gender bias is a strong reason for women leaving academic medicine2,6 and that addressing gender bias in compensation, recognition, and institutional support can be helpful.7,10,13,14,15,16 Furthermore, gender bias training has been shown to improve women’s perception of their environment and value.17 Participation in career development programs12,18,19,20,21 had a positive impact on retention, and interventions targeted towards work-life integration such as flexible work schedules, fair and transparent family leave policies, and onsite day care have been proposed as well.6,22,23,24
While a multipronged approach to addressing many of these issues in retention (and promotion) has been proposed,1,4,23 a minority of academic medical centers have implemented such strategies thus far and very few studies have examined the actual impact of these initiatives on the self-perception of retention of women in academic medicine.4 We sought to identify any demographic or institutional factors that may be associated with women faculty’s intent to remain at their institutions and/or remain in academic medicine in hopes to further guide academic institutions in addressing gender gaps within their own institutions.
METHODS
Survey Recruitment
We recruited women at American academic medical centers to complete our survey from October through December 2019 using listservs for Alliance for Academic Internal Medicine (AAIM), The Society of General Internal Medicine (SGIM), and a national social media group for women physician mothers, Physician Moms Group (PMG). The anonymous survey, administered through Qualtrics®, was voluntary, and participants were informed that completion of the survey served as consent to participate in the study. No incentive was provided for completion of the survey. Inclusion criteria included (1) women with an active faculty appointment within a department of medicine and (2) women with a doctoral degree (e.g., MD, DO). Women faculty contacted the research team regarding the exclusion of women faculty with PhDs and the potential implications. In November 2019, the research team refined the inclusion criteria to include PhDs during continued recruitment. Using 17,504 as the number of women faculty in internal medicine departments in 2018 according to the AAMC, a 95% confidence interval and p value < .05, and Cochran’s formula, we calculated an ideal sample size of 376 participants for a representative sample25.
Survey Development
To our knowledge, a validated survey tool to investigate retention factors of women in academic medicine does not exist. Survey items were derived from review of the existing literature regarding identified retention factors and proposed solutions (addressing gender bias in resources, salary, and promotion; career development programs; skill building opportunities; mentorship; networking; fair and transparent policies and procedures; and support for work-life integration) to address retention of women in academic medicine.6,23,26,27 The survey was piloted by seven women faculty of various ranks (results not included in final analysis), reviewed in consultation with an expert in human and organizational learning, and refined for construct validity. The full final survey (see Supplemental Material 1) included a set of 27 agreement Likert scale questions regarding specific institutional factors, perceptions of bias, one’s intent to remain at one’s institution and in academic medicine, and attendance at a National Career Development Program (CDP). Survey respondents also reported on their demographics, professional experience, academic rank, support for household responsibilities, and childcare status. The study was designated as exempt by The George Washington University IRB.
Statistical Analyses
Our main outcome measures were (1) intent to remain at the current institution and (2) intent to remain in academic medicine. We re-coded Likert scale responses for our two outcome measures to create a binary measure (strongly agree or agree = Yes, intend to remain at institution or in academic medicine; all other Likert scale responses = No, do not intend to remain at institution or in academic medicine). Survey question responses were compared across these binary outcome measures using chi-squared tests (Table 2).
We constructed three logistic regression models for each binary primary outcome measure to assess for factors associated with the intent to remain at an institution and intent to remain in academic medicine. Each of the three models for each outcome included survey questions from one domain of interest as covariates. The three domains included in this paper are gender bias/fairness, mentorship, and work-life integration. Within each outcome, the fit of each of the three domain models were compared using Akaike information criterion (AIC). All models also included the demographic variables in Table 1 as covariates. Likert survey question responses were binarized as was done for the outcome measures. Results are reported as odds ratios (ORs) with corresponding 95% confidence intervals (CIs). All data were analyzed using R version 3.6.1 (Foundation for Statistical Computing).
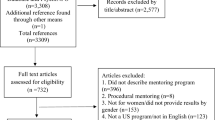
RESULTS
We received 553 initial responses, 18 of those did not meet inclusion criteria. A total of 114 participants did not progress through the entire survey, and their responses were excluded from all analyses. Due to the small number of women PhD participants (N = 11), we excluded this group as it was not representative of the proportion of women faculty with doctorates other than MD/DO within departments of medicine nationally (12%)25. Data from the remaining 410 survey participants were analyzed.
Demographics
The demographics of participants are shown in Table 1. The sample included women across all academic ranks and across all regions of the country. Almost half (46.3%) of the participants held assistant professor appointments. The ethnic distribution was representative to what is seen in academic medicine.25 Most participants were in general internal medicine (64.4%). The majority (87.8%) work at least 0.76 FTE, but over half have less than 60% clinical time (60.0%). Two-thirds of the women care for children under the age of 18. Close to half of all women (43.9%) felt that they had minimal to no sufficient support for household responsibilities unrelated to their career.
Primary Outcome: Intent to Remain at Institution
The majority of women (67.6%) surveyed reported intent to remain at their academic institution for the next 5 years and 80.6% reported intent to remain in academic medicine for the next 5 years (Table 2). The distribution of survey responses between women who agreed they intend to remain at their institution versus not remain at their institution was significantly different for all of the survey questions compared with the exception of onsite childcare (Table 2). Results were similar when restricting to women who participated in a national CDP (data not shown). AIC was lowest for the regression model including work-life domain questions, indicating a better fit than the models with the bias/fairness and mentorship domain questions (Table 3). Bias/fairness and mentorship domain item regression analysis results are included in supplemental tables. Western region participants had lower odds of intending to remain at their current institutions (OR 0.37, 95% CI 0.15–0.88, p = 0.03) compared to women from other regions of the USA. Women who identified as Black (OR 0.17, 95% CI 0.04–0.70, p = 0.01) or “other” (OR 0.31, 95% CI 0.12–0.79, p = 0.02) had lower odds of intending to remain at their current institution. Survey responses associated with the intent to remain at their current institution included agreement with the following: the institution helps employees recognize gender bias (OR 1.77, 95% CI 1.01–3.13, p < 0.05), they were compensated fairly for the work they do (OR 2.00, 95% CI 1.07–3.79, p = 0.03), provided resources similar to others to support role (OR 2.83, 95% CI 1.56–5.24, p < 0.001), satisfied with mentorship opportunities (OR 2.94, 95% CI 1.46–6.03, p < 0.01), participated in peer mentorship (OR 2.09, 95% CI 1.18–3.73, p = 0.01), saw women role models in positions of leadership at the institution (OR 2.11, 95% CI 1.11–4.04, p = 0.02), perceived family leave policy as fair and transparent (OR 2.22, 95% CI 1.20–4.18, p = 0.01), emergency child care was present (OR 2.23, 95% CI 1.07–4.90, p = 0.04), and that their institutions provided opportunities for work-life integration (OR 4.82, 95% CI 2.50–9.64, p < 0.001) (Table 3; Supplemental Tables).
Primary Outcome: Intent to Remain in Academic Medicine
The distribution of survey responses between women who agreed they intend to remain in academic medicine versus not remain in academic medicine was significantly different for all of the survey questions compared (p < 0.05; Table 2) except for the items regarding onsite childcare, lactation support, emergency childcare, and implementation of gender bias training for leaders. Results were similar when restricting to women who participated in a national CDP (data not shown). AIC was lowest for the regression model including work-life domain questions, indicating a better fit than the models with the bias/fairness and mentorship domain questions (Table 3). Bias/fairness and mentorship domain item regression analysis results are included in supplemental tables. Women who worked in the Southern USA had higher odds of intending to stay in academic medicine, while women who identified as Black or other race had lower odds of intending to stay in academic medicine (Southern USA: OR 3.14, 95% CI 1.17–8.75, p = 0.02; Black race: OR = 0.11, 95% CI 0.02–0.50, p < 0.01; other race: OR = 0.26, 95% CI 0.10–0.73, p = 0.01; Table 3). No other demographic elements had a significant association. However, survey responses that were associated with the intent to remain in academic medicine included agreement with the following: participated in peer mentorship (OR 3.16, 95% CI 1.56–6.57, p < 0.01), there were women role models in positions of leadership at one’s institution (OR 2.21, 95% CI 1.04–4.68, p = 0.04), the family leave policy at their institution is fair and transparent (OR = 2.31, 95%CI 1.09–5.03, p = 0.03), and that their institution provides opportunities for one to integrate their work and life identities (OR = 4.66, 95% CI 2.04–11.36, p < 0.001).
DISCUSSION
This study of women faculty in academic medicine is, to our knowledge, the first nationwide cross-sectional study looking at institutional factors and their relationship to women faculty’s intent to remain at their current academic institutions and in academic medicine in general. We found that the majority of women intend to stay at their current institutions. There was a significant association with intent to stay at their current institution and remain in academic medicine if women faculty participated in peer mentorship, there were women leaders as role models at one’s institution, the institution’s family leave policy was perceived as fair and transparent, and the institution provided opportunities for work-life integration, with work-life integration carrying the strongest association in both categories. In addition, there was a significant association specifically with intent to stay at their current institution if the participants agreed the institution helped employees recognize bias, perceived fair compensation and similar access to resources, and were satisfied with mentorship in general. There were a considerable number of women who either felt neutral, disagreed, or stated that specific interventions were not present at their institution, which is consistent with a prior study of women leaders at 23 academic institutions showing that retention-linked interventions have not been fully adopted across academic institutions.23
While gender bias has been reported as a reason some women leave academic medicine2 and gender bias training has shown some positive impacts,17 our study showed intention to stay at one’s institution if the institution helps employees recognize bias, and participants perceived fair compensation and provision of resources similar to others but no association with the presence of gender bias training for leadership and committee members and intent to stay. These findings do not negate the positive impacts of gender bias training seen in prior studies,17 but it suggests that bias training for leadership and selection committees alone is not enough to impact the intent to remain at an institution without addressing other factors, such as helping all employees recognize their bias as well as attention to fair compensation and fair allocation of resources and support.
In addition, identifying as Black or “other” in the survey was associated with a lower intent to remain within academic medicine when compared to other ethnic groups. It is important to not only recognize the additional barriers that women faculty from groups underrepresented in medicine (UIM) face, but academia must be intentional in recognizing that retention strategies may not be a one-size fit all.
Mentorship has also been described as a meaningful way to promote retention of women in academic medicine. Our study showed a statistically significant association between peer mentorship, satisfaction of mentorship opportunities, and women role models in positions of leadership and intent to remain at one’s institution. However, while showing a positive trend, a statistically significant association between formal mentorship, facilitated peer mentorship, or women in medicine programs and women faculty’s intent to stay at their institutions or in academic medicine was not found. Given the relatively small percentages of women faculty in our study sample who agreed that formal mentorship (55%) or facilitated peer mentorship (24%) programs were present at their institution, the presence of informal mentorship may be the driving factor for this finding. Again, our findings do not diminish the importance of formally facilitated mentorship and sponsorship (not studied) discussed in other literature, but more research is needed to determine the optimal implementation and the impact of these programs.
Agreement that the institution provided work-life integration opportunities had the strongest impact on intent to remain both at the institution and in academic medicine. However, emergency childcare and a fair and transparent family leave policy were the only specific aspects of work-life integration from the survey that showed a statistically significant association with intent to stay at one’s current institution. A family leave policy that was fair and transparent was the only work-life-related factor that showed a statistically significant association with both intent to stay at one’s current institution and in academic medicine. We did not define work-life integration for study participants. It is also unclear how and to what degree institutions provide such opportunities, indicating a need for further investigation to evaluate individual aspects of work-life integration.
Strengths of our study are that it includes women faculty, recruited through national listservs, from institutions across the country at various ranks and stages in their career. The survey, derived from the review of the literature, allowed us to study retention-linked factors across multiple domains. Our sample size exceeded our ideal sample size and participant distribution based on rank and ethnic group appears similar to the distribution within academic departments of medicine nationwide.25 Our study also included general internal medicine specialists as well as subspecialists within general medicine.
There were limitations to our study as well as opportunities for future research. Participation in the study was voluntary which could lead to selection bias wherein women who were more interested in the topic chose to participate. Generalizability may be limited. Recruitment through AAIM, SGIM, and PMG listservs allowed us to capture women nationwide; however, we cannot estimate a response rate or true representativeness since we do not know the total number of women academic internists on the listservs nor the number of people in the target population that viewed the posts. Also, in the initial recruitment phase, non-MD or DOs were not included due to concern about introducing more variables. Despite inclusion criteria expansion, our final sample did not yield a representative sample of this group, and their responses were excluded in this manuscript. Although relatively consistent with AAMC data25, the actual percentages of Black or African American, Hispanic or Latina, and Asian women faculty were low which limits generalizability to non-majority groups. Finally, we were not able to report on actual retention of women in medicine and instead report intent to remain in academic medicine. It is possible factors influencing retention change over time and are not captured here using our survey instrument.
Opportunities for future research include targeting non-MD/DO faculty and sampling women within other areas/specialties of medicine. Future studies specifically focusing on women faculty belonging to ethnic minority groups are also needed, especially in light that identifying as Black or “other” was associated with a lower intent to remain in academic medicine. Further investigation into specific work-life integration strategies may guide institutions as well.
Data show that gender gaps in retention and promotion in academic medicine exist despite women entering medicine at higher rates than men. Our study of women faculty of various ranks in departments of medicine across the USA sheds light on factors associated with women faculty’s intent to remain in academic medicine and at one’s institution. Our data supports that fair compensation and resource allocation, effective mentorship opportunities, transparent and fair policies, and improved work-life integration appear impactful for the retention of women in academic institutions. In addition, the majority of women faculty reported caring for minor child(ren) and close to half have minimal to no support for non-career-related responsibilities. These findings and the strong association between opportunities for work-life integration and intent to stay at one’s institution and remain within academic medicine highlight the importance of work-life integration strategies, policies, and practices in institutional efforts to retain women faculty.
References
Lautenberger DM, Dandar VM. The State of Women in Academic Medicine: Exploring pathways to equity, 2018–2019. 2020. Washington, DC: Association of American Medical Colleges. [cited 2020 Dec 31]. Available from: https://www.aamc.org/data-reports/data/2018-2019-state-women-academic-medicine-exploring-pathways-equity
Levine RB, Lin F, Kern DE, Wright SM, Carrese J. Stories from early-career women physicians who have left academic medicine: a qualitative study at a single institution. AcadMed. 2011; Jun 1;86(6):752-8.
Liu CQ, Morrison E. US medical school full-time faculty attrition. Anal Brief. 2014; Feb;14:1-2.
Carr PL, Raj A, Kaplan SE, Terrin N, Breeze JL, Freund KM. Gender differences in academic medicine: retention, rank, and leadership comparisons from the National Faculty Survey. Acad Med. 2018; Nov 1;93(11):1694-9.
Pololi LH, Civian JT, Brennan RT, Dottolo AL, Krupat E. Experiencing the culture of academic medicine: gender matters, a national study. J of Gen Intern Med. 2013; Feb 1;28(2):201-7.
Horn KV. Gender bias in academic medicine. Donald School J Ultrasound Obstet Gynecol. 2014; 8:97-9.
Sege R, Nykiel-Bub L, Selk S. Sex differences in institutional support for junior biomedical researchers. Jama. 2015; Sep 15;314(11):1175-7.
Westring AF, Speck RM, Sammel MD, et al. Culture matters: the pivotal role of culture for women’s careers in academic medicine. Acad Med. 2014; Apr;89(4):658.
Shollen SL, Bland CJ, Finstad DA, Taylor AL. Organizational climate and family life: how these factors affect the status of women faculty at one medical school. Acad Med. 2009; Jan 1;84(1):87-94.
Ash AS, Carr PL, Goldstein R, Friedman RH. Compensation and advancement of women in academic medicine: is there equity? Ann of Intern Med. 2004; Aug 3;141(3):205-12.
Nonnemaker L. Women physicians in academic medicine—new insights from cohort studies. New Engl J Med. 2000; Feb 10;342(6):399-405.
Chang S, Morahan PS, Magrane D, et al. Retaining faculty in academic medicine: the impact of career development programs for women. J Women’s Health. 2016; Jul 1;25(7):687-96.
Asgari MM, Carr PL, Bates CK. Closing the gender wage gap and achieving professional equity in medicine. Jama. 2019; May 7;321(17):1665-6.
Jagsi R, Griffith KA, Stewart A, Sambuco D, DeCastro R, Ubel PA. Gender differences in the salaries of physician researchers. Jama. 2012; Jun 13;307(22):2410-7.
Freund KM, Raj A, Kaplan SE, et al.. Inequities in academic compensation by gender: a follow-up to the National Faculty Survey cohort study. Acad med. 2016; Aug;91(8):1068.
Morgan AU, Chaiyachati KH, Weissman GE, Liao JM. Eliminating gender-based bias in academic medicine: more than naming the “elephant in the room”. J Gen Intern Med. 2018; Jun 1;33(6):966-8.
Carnes M, Devine PG, Manwell LB, et al. Effect of an intervention to break the gender bias habit for faculty at one institution: a cluster randomized, controlled trial. Acad Med. 2015; Feb;90(2):221.
Bauman MD, Howell LP, Villablanca AC. The Women in Medicine and Health Science program: an innovative initiative to support female faculty at the University of California Davis School of Medicine. Acad Med. 2014; Nov;89(11):1462.
Fassiotto M, Maldonado Y, Hopkins J. A long-term follow-up of a physician leadership program. J of Health Organ Manage. 2018; Mar 19.
Valantine HA, Grewal D, Ku MC, et al. The gender gap in academic medicine: comparing results from a multifaceted intervention for Stanford faculty to peer and national cohorts. Acad Med. 2014; Jun 1;89(6):904-11.
Fried LP, Francomano CA, MacDonald SM, et al. Career development for women in academic medicine: multiple interventions in a department of medicine. Jama. 1996; Sep 18;276(11):898-905.
McGuire LK, Bergen MR, Polan ML. Career advancement for women faculty in a US school of medicine: perceived needs. Acad Med. 2004; Apr 1;79(4):319-25.
Carr PL, Gunn C, Raj A, Kaplan S, Freund KM. Recruitment, promotion, and retention of women in academic medicine: how institutions are addressing gender disparities. Womens Health Issues. 2017; May 1;27(3):374-81.
Jolly S, Griffith KA, DeCastro R, Stewart A, Libel P, Jagsi R. Gender Differences in Time Spent on Parenting and Domestic Responsibilities by High-Achieving Young Physician-Researchers. Ann of Intern Med. 2014; 160(5):344-53. doi: https://doi.org/10.7326/M13-0974.
Aamc.org [Internet]. Association of American Medical Colleges (2019). Table 19: U.S. Medical School Faculty by Sex, Race/Ethnicity, Rank, and Department, 2018. [cited 2020 Jan 11]. Available from: https://www.aamc.org/system/files/2020-01/2018Table19.pdf .
Sambunjak, D., Straus, S.E., Marusić, A. Mentoring in academic medicine: a systematic review. Jama. 2016; 296, 1103–1115.
George, C. Retaining professional workers: what makes them stay? Employee Relations. 2015; 37 (10)102-121.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they do not have a conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
ESM 1
(DOCX 33 kb)
Rights and permissions
About this article
Cite this article
Onumah, C., Wikstrom, S., Valencia, V. et al. What Women Need: a Study of Institutional Factors and Women Faculty’s Intent to Remain in Academic Medicine. J GEN INTERN MED 36, 2039–2047 (2021). https://doi.org/10.1007/s11606-021-06771-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-021-06771-z