Abstract
Background
Women physicians have faced persistent challenges, including gender bias, salary inequities, a disproportionate share of caregiving and domestic responsibilities, and limited representation in leadership. Data indicate the COVID-19 pandemic further highlighted and exacerbated these inequities.
Objective
To understand the pandemic’s impact on women physicians and to brainstorm solutions to better support women physicians.
Design
Mixed-gender semi-structured focus groups.
Participants
Hospitalists in the Hospital Medicine Reengineering Network (HOMERuN).
Approach
Six semi-structured virtual focus groups were held with 22 individuals from 13 institutions comprised primarily of academic hospitalist physicians. Rapid qualitative methods including templated summaries and matrix analysis were applied to identify major themes and subthemes.
Key Results
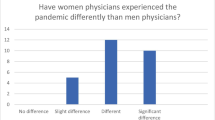
Four key themes emerged: (1) the pandemic exacerbated perceived gender inequities, (2) women’s academic productivity and career development were negatively impacted, (3) women held disproportionate roles as caregivers and household managers, and (4) institutional pandemic responses were often misaligned with workforce needs, especially those of women hospitalists. Multiple interventions were proposed including: creating targeted workforce solutions and benefits to address the disproportionate caregiving burden placed on women, addressing hospitalist scheduling and leave practices, ensuring promotion pathways value clinical and COVID-19 contributions, creating transparency around salary and non-clinical time allocation, and ensuring women are better represented in leadership roles.
Conclusions
Hospitalists perceived and experienced that women physicians faced negative impacts from the pandemic in multiple domains including leadership opportunities and scholarship, while also shouldering larger caregiving duties than men. There are many opportunities to improve workplace conditions for women; however, current institutional efforts were perceived as misaligned to actual needs. Thus, policy and programmatic changes, such as those proposed by this cohort of hospitalists, are needed to advance equity in the workplace.
Similar content being viewed by others
Data Availability
De-identified data generated and/or analyzed during the current study are available from the corresponding author upon reasonable request.
References
Jena AB, Olenski AR, Blumenthal DM. Sex Differences in Physician Salary in US Public Medical Schools. JAMA Intern Med. 2016;176(9):1294-1304. https://doi.org/10.1001/jamainternmed.2016.3284
Gottlieb AS, Jagsi R. Closing the Gender Pay Gap in Medicine. N Engl J Med. 2021;385(27):2501-2504. https://doi.org/10.1056/NEJMp2114955
Carr PL, Raj A, Kaplan SE, Terrin N, Breeze JL, Freund KM. Gender Differences in Academic Medicine: Retention, Rank, and Leadership Comparisons From the National Faculty Survey. Acad Med J Assoc Am Med Coll. 2018;93(11):1694-1699. https://doi.org/10.1097/ACM.0000000000002146
Richter KP, Clark L, Wick JA, et al. Women Physicians and Promotion in Academic Medicine. N Engl J Med. 2020;383(22):2148-2157. https://doi.org/10.1056/NEJMsa1916935
Jolly S, Griffith KA, DeCastro R, Stewart A, Ubel P, Jagsi R. Gender Differences in Time Spent on Parenting and Domestic Responsibilities by High-Achieving Young Physician-Researchers. Ann Intern Med. 2014;160(5):344-353. https://doi.org/10.7326/M13-0974
Northcutt N, Papp S, Keniston A, et al. SPEAKers at the National Society of Hospital Medicine Meeting: A Follow-UP Study of Gender Equity for Conference Speakers from 2015 to 2019. The SPEAK UP Study. J Hosp Med. 2020;15(4):228-231. https://doi.org/10.12788/jhm.3401
Hart KL, Perlis RH. Trends in Proportion of Women as Authors of Medical Journal Articles, 2008-2018. JAMA Intern Med. 2019;179(9):1285-1287. https://doi.org/10.1001/jamainternmed.2019.0907
Jagsi R, Guancial EA, Worobey CC, et al. The “Gender Gap” in Authorship of Academic Medical Literature — A 35-Year Perspective. N Engl J Med. 2006;355(3):281-287. https://doi.org/10.1056/NEJMsa053910
Keller T, Wilson M, Chung K, Andrilla CH, Evans D, Cawse-Lucas J. Gender Differences in Authorship of Family Medicine Publications, 2002-2017. Fam Med. 2021;53(6):416-422. https://doi.org/10.22454/FamMed.2021.866524
Weaver AC, Wetterneck TB, Whelan CT, Hinami K. A matter of priorities? Exploring the persistent gender pay gap in hospital medicine. J Hosp Med. 2015;10(8):486-490. https://doi.org/10.1002/jhm.2400
Burden M, Frank MG, Keniston A, et al. Gender disparities in leadership and scholarly productivity of academic hospitalists. J Hosp Med. 2015;10(8):481-485. https://doi.org/10.1002/jhm.2340
Kibbe MR. Consequences of the COVID-19 Pandemic on Manuscript Submissions by Women. JAMA Surg. 2020;155(9):803-804. https://doi.org/10.1001/jamasurg.2020.3917
Wright KM, Wheat S, Clements DS, Edberg D. COVID-19 and Gender Differences in Family Medicine Scholarship. Ann Fam Med. 2022;20(1):32-34. https://doi.org/10.1370/afm.2756
Andersen JP, Nielsen MW, Simone NL, Lewiss RE, Jagsi R. COVID-19 medical papers have fewer women first authors than expected. eLife. 9:e58807. https://doi.org/10.7554/eLife.58807
Sumarsono A, Keshvani N, Saleh SN, et al. Scholarly Productivity and Rank in Academic Hospital Medicine. J Hosp Med. 2021;16(9):545-548. https://doi.org/10.12788/jhm.3631
Gross T. Pandemic Makes Evident “Grotesque” Gender Inequality In Household Work. NPR. https://www.npr.org/2020/05/21/860091230/pandemic-makes-evident-grotesque-gender-inequality-in-household-work. Published May 21, 2020. Accessed June 13, 2022.
Brown C, Jain S, Santhosh L. How Has the Pandemic Affected Women in Medicine? A Survey-Based Study on Perceptions of Personal and Career Impacts of COVID-19. Womens Health Rep New Rochelle N. 2021;2(1):396-399. https://doi.org/10.1089/whr.2021.0031
Koval ML. Medscape Hospitalist Compensation Report 2022. Medscape. Accessed November 28, 2022. https://www.medscape.com/slideshow/2022-compensation-hospitalist-6015551#21
Auerbach AD, Patel MS, Metlay J, et al. The Hospital Medicine Reengineering Network (HOMERuN): A learning organization focused on improving hospital care. Acad Med J Assoc Am Med Coll. 2014;89(3):415-420. https://doi.org/10.1097/ACM.0000000000000139
Keniston A, McBeth L, Astik G, et al. Practical Applications of Rapid Qualitative Analysis for Operations, Quality Improvement, and Research in Dynamically Changing Hospital Environments. Jt Comm J Qual Patient Saf. Published online November 2022:S1553725022002689. https://doi.org/10.1016/j.jcjq.2022.11.003
Creswell J. Qualitative Inquiry and Research Design: Choosing Among Five Approaches. Fourth Edition. Fourth Edition. SAGE Publications; 2017.
Averill JB. Matrix analysis as a complementary analytic strategy in qualitative inquiry. Qual Health Res. 2002;12(6):855-866. https://doi.org/10.1177/104973230201200611
Hamilton AB. Qualitative Methods in Rapid Turn-Around Health Services Research. Presented at: VA HSR&D Cyberseminar Spotlight on Women’s Health; December 11, 2013; VA Greater Los Angeles Healthcare Innovation, Implementation, & Policy. Accessed May 1, 2021. https://www.hsrd.research.va.gov/for_researchers/cyber_seminars/archives/780-notes.pdf
Keniston A, Sakumoto M, Astik GJ, et al. Adaptability on Shifting Ground: a Rapid Qualitative Assessment of Multi-institutional Inpatient Surge Planning and Workforce Deployment During the COVID-19 Pandemic. J Gen Intern Med. Published online March 22, 2022:1–9. https://doi.org/10.1007/s11606-022-07480-x
Birt L, Scott S, Cavers D, Campbell C, Walter F. Member Checking: A Tool to Enhance Trustworthiness or Merely a Nod to Validation? Qual Health Res. 2016;26(13):1802-1811. https://doi.org/10.1177/1049732316654870
Santhosh L, Keenan BP, Jain S. The “Third Shift”: A Path Forward to Recognizing and Funding Gender Equity Efforts. J Womens Health 2002. 2020;29(11):1359–1360. https://doi.org/10.1089/jwh.2020.8679
Landau C. The Third Shift. The Third Shift. Published October 23, 2020. Accessed May 1, 2022. https://www.psychologytoday.com/us/blog/mood-prep-101/202010/the-third-shift
Pay inequity, flex schedules top concerns for women physicians. American Medical Association. Accessed June 13, 2022. https://www.ama-assn.org/delivering-care/health-equity/pay-inequity-flex-schedules-top-concerns-women-physicians
Frank E, Zhao Z, Fang Y, Rotenstein LS, Sen S, Guille C. Experiences of Work-Family Conflict and Mental Health Symptoms by Gender Among Physician Parents During the COVID-19 Pandemic. JAMA Netw Open. 2021;4(11):e2134315. https://doi.org/10.1001/jamanetworkopen.2021.34315
Pino-Jones AD, Cervantes L, Flores S, et al. Advancing Diversity, Equity, and Inclusion in Hospital Medicine. J Hosp Med. 2021;16(4):198-203. https://doi.org/10.12788/jhm.3574
Defoe MV, Cameron KA, Burden M, et al. Men and Women Pursue Nonlinear Career Paths, but Impacts Differ: a Cross-Sectional Study of Academic Hospitalists. J Gen Intern Med. 2022;37(12):3097-3104. https://doi.org/10.1007/s11606-022-07402-x
Arogyaswamy S, Vukovic N, Keniston A, et al. The Impact of Hospital Capacity Strain: a Qualitative Analysis of Experience and Solutions at 13 Academic Medical Centers. J Gen Intern Med. 2022;37(6):1463-1474. https://doi.org/10.1007/s11606-021-07106-8
Sharma U. Ideal Hospitalist Workload in a 12-Hour Shift. Am J Med Qual. 2019;34(1):98-98. https://doi.org/10.1177/1062860618778347
Elliott DJ, Young RS, Brice J, Aguiar R, Kolm P. Effect of hospitalist workload on the quality and efficiency of care. JAMA Intern Med. 2014;174(5):786-793. https://doi.org/10.1001/jamainternmed.2014.300
Brown DR, Hernández A, Saint-Jean G, et al. A participatory action research pilot study of urban health disparities using rapid assessment response and evaluation. Am J Public Health. 2008;98(1):28-38. https://doi.org/10.2105/AJPH.2006.091363
Burks DJ, Robbins R, Durtschi JP. American Indian gay, bisexual and two-spirit men: a rapid assessment of HIV/AIDS risk factors, barriers to prevention and culturally-sensitive intervention. Cult Health Sex. 2011;13(3):283-298. https://doi.org/10.1080/13691058.2010.525666
Vindrola-Padros C, Chisnall G, Cooper S, et al. Carrying Out Rapid Qualitative Research During a Pandemic: Emerging Lessons From COVID-19. Qual Health Res. 2020;30(14):2192-2204. https://doi.org/10.1177/1049732320951526
Beebe J. Rapid Qualitative Inquiry: A Field Guide to Team-Based Assessment. Second.
Gale RC, Wu J, Erhardt T, et al. Comparison of rapid vs in-depth qualitative analytic methods from a process evaluation of academic detailing in the Veterans Health Administration. Implement Sci. 2019;14(1):11. https://doi.org/10.1186/s13012-019-0853-y
Moreau J. Rapid qualitative methods. Presented at: Colorado Pragmatic Research in Health Conference (Virtual Conference); August 12, 2020.
Zuchowski JL, Chrystal JG, Hamilton AB, et al. Coordinating Care Across Health Care Systems for Veterans With Gynecologic Malignancies: A Qualitative Analysis. Med Care. 2017;55 Suppl 7 Suppl 1:S53-S60. https://doi.org/10.1097/MLR.0000000000000737
Taylor B, Henshall C, Kenyon S, Litchfield I, Greenfield S. Can rapid approaches to qualitative analysis deliver timely, valid findings to clinical leaders? A mixed methods study comparing rapid and thematic analysis. BMJ Open. 2018;8(10):e019993. https://doi.org/10.1136/bmjopen-2017-019993
Kulkarni SA, Keniston A, Linker AS, et al. Building a thriving academic hospitalist workforce: A rapid qualitative analysis identifying key areas of focus in the field. J Hosp Med. 2023;18(4):329-336. https://doi.org/10.1002/jhm.13074
Acknowledgements
Thanks to our participants and members of the HOMERuN COVID-19 Collaborative Group, especially Tiffany Lee who skillfully manages this group.
Funding
Dr. Leykum receives salary support from the Department of Veterans Affairs (SDR 18–313). The views expressed do not represent the position of the Department of Veterans Affairs or other organizations affiliated with the authors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they do not have a conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
ESM 1
(DOCX 26.1 kb)
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Busch, J.I., Keniston, A., Astik, G.J. et al. Exploring the Impact of COVID-19 on Women Hospitalists: A Mixed-Gender Qualitative Analysis. J GEN INTERN MED 38, 3180–3187 (2023). https://doi.org/10.1007/s11606-023-08371-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-023-08371-5