Abstract
Background
Operable esophageal carcinoma is potentially curable with surgical resection. The short-term outcomes and overall survival rate for operable esophageal carcinoma may be impacted by the healthcare facility type where patients receive care.
Methods
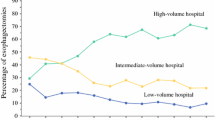
A total of 37, 271 cases with the American Joint Committee on Cancer clinical stage I, II, and III esophageal carcinoma that were reported to the National Cancer Data Base at over 12,721 facilities were analyzed. Healthcare facilities were dichotomized into the community and academic facility types. Marginal multivariable Cox proportional hazard models were used to evaluate differences in overall survival between facility types, which accounted for facility esophageal cancer volume. Propensity score methodology with inverse probability of treatment weighting was used to adjust for patient related baseline differences between facility types.
Results
Patients with clinical stage I–III esophageal carcinoma who underwent esophagectomy at academic healthcare facilities had a significantly better overall survival compared with patients who underwent esophagectomy at community healthcare facilities [HR = 0.89: CI [0.84–0.95] (p = 0.0005)]. The rate of esophagectomy was significantly higher at the academic facilities (49.0% versus 26.5%; p < 0.0001). The 30-day and 90-day mortality rates for esophagectomy were significantly better for patients who underwent esophagectomy for esophageal cancer at the academic facility types.
Conclusion
Patients with clinical stage I–III esophageal carcinoma who received care at academic facility types had significantly better overall survival compared with community facility types. The utilization of esophagectomy was significantly higher and the short-term surgical outcomes were better for patients treated at academic facility types.






Similar content being viewed by others
References
Siegel RL, Miller KD, Jemal A. Cancer statistics, 2019. CA: a cancer journal for clinicians. 2019; 69(1):7-34.
Kamangar F, Dores GM, Anderson WF. Patterns of cancer incidence, mortality, and prevalence across five continents: defining priorities to reduce cancer disparities in different geographic regions of the world. J Clin Oncol 2006; 24:2137-2150.
Van Hagen P, Hulshof MC, Van Lanschott JJ, et al. Preoperative chemoradiotherapy for esophageal or junctional cancer. N Engl J Med 2012; 366:20174-84.
Begg CB, Cramer LD, Hoskins WJ, et al. Impact of hospital volume on operative mortality for major cancer surgery. JAMA 1998:280:1747-51.
Birkmeyer JD, Sun Y, Goldfaden A, et al. Volume and process of care in high risk cancer surgery. Cancer 2006:106:2476-2481.
Birkmeyer JD, Sun Y, Wong Sl, et al. Hospital volume and late survival after cancer surgery, Ann Surg 2007;245:777-83.
Bilimoria KY, Stewart AK, Winchester DP, Ko CY. The National Cancer Database: a powerful initiative to improve cancer care in the United States. Ann Surg Oncol 2008; 15:683-690.
Commission on Cancer- Cancer Program Categories. https://www.facs.org/qualityprograms/cancer/coc/accreditation/categories#cccp. Accessed on August 8, 2020.
Austin PC. A tutorial on multilevel survival analysis: methods, models, and applications. Int Stat Rev 2017 August; 85(20:185-203.
Austin PC and Stuart EA. Moving towards best practice when using inverse probability of treatment weighting (IPTW) using the propensity score to estimate causal treatment effects in observational studies. Statist Med 2015; 34:3661-79.
Wright CD, Kucharczuk JC, O’Brien SM, et al. Predictors of major morbidity and mortality after esophagectomy for esophageal cancer: a Society of Thoracic Surgeons General Thoracic Surgery Database risk adjustment model. J Thorac Cardiovasc Surg 2009; 137:587-95.
Kozower BD and Stukenborg GJ. Hospital esophageal cancer resection volume does not predict patient mortality risk. Ann Thorac Surg 2012;93:1690-98.
Markar SR, Karthikesalingam A, Thrumurthy S, Low DE. Volume-outcome relationship in surgery for esophageal malignancy: systematic review and meta-analysis 2000-2011. J Gastointestinal Surg 2012; 16:1055-63.
Massarweh NN, Flum DR, Symons RG, et al. A critical evaluation of the impact of Leapfrog’s evidence-based hospital referral. J Am Coll Surg 2011;212(2):150-59.
The Leapfrog Group. Leapgrog Hospital Survey-Factsheet: inpatient surgery. Available at: http://www.leapfrog.org/sites/default/files/2020. Accessed June 5, 2020.
Clark JM, Cooke DT, Hashimi H, et al. Do the 2018 Leaprfrog Group minimal hospital and surgeon volume thresholds for esophagectomy favor specific patient demographics? Ann Surg 2019.
Paulson EC, Ra J, Armstrong, Wirtralla BA, et al. Underuse of esophagectomy as treatment of resectable esophageal cancer. Arch Surg 2008;143(12):1198-1203.
Taylor LJ, Greenberg CC, Lidor AO, et al. Utilization of surgical treatment for local and locoregional esophageal cancer: analysis of the National Cancer Data Base. Cancer 2017;123:410-219.
Dubecz A, Sepesi B, Salvador R, et al. Surgical resection for locoregional esophageal cancer is underutilized in the United States. J Am Coll Surg 2010;211:754-761.
Mariette C, Markar SR, Dabakuyo-Yonli, et al. Hybrid minimally invasive esophagectomy for esophageal cancer. N Engl J Med 2019;380:152-62.
Biere SS, Van Berge Henegouwen MI, Bonavina K, et al. Minimally invasive versus open oesophagectomy for patients with oesopahgeal cancer: a multi-centre, open-label, randomized control trial. Lancet 2012; 379(9829): 1887-92.
Birkmeyer JD, Stukel TA, Siewers AE, et al. Surgeon volume and operative mortality in the United States. N Engl J Med 2003;349:2117-2127.
Lagarde SM, de Boer JD, Ten Kate FJ, et al. Postoperative complications after esophagectomy for adenocarcinoma of the esophagus are related to timing of death die to recurrence Ann Surg 2008:247:71-76.
Lerut T, Moons J, Coosemans W, et al. Postoperative complications after transthoracic esophagectomy for cancer of the esophagus and gastroesophageal junction are correlated with early cancer recurrence: role of systematic grading of complications using the modified Clavien classification. Ann Surg 2009;250:798-807.
Rizk NP, Bach PB, Schrag D, et al. The impact of complications on outcomes after resection for esophageal and gastroesophageal junction carcinoma. J Am Coll Surg 2004;198:42-50.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Merritt, R.E., Abdel-Rasoul, M., Fitzgerald, M. et al. The Academic Facility Is Associated with Higher Utilization of Esophagectomy and Improved Overall Survival for Esophageal Carcinoma. J Gastrointest Surg 25, 1677–1689 (2021). https://doi.org/10.1007/s11605-020-04817-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-020-04817-x