Abstract
Background
The aim of this study is to provide a contemporary quantitative analysis of the existing literature examining the relationship between surgical caseload and outcome following esophageal resection.
Methods
Medline, Embase, trial registries, conference proceedings and reference lists were searched for trials comparing clinical outcome following esophagectomy from high- and low-volume hospitals since 2000. Primary outcomes were in-hospital and 30-day mortality. Secondary outcomes were length of hospital stay and post-operative complications.
Results
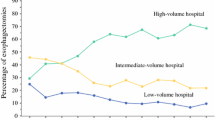
Nine appropriate publications comprising 27,843 esophagectomy operations were included, 12,130 and 15,713 operations were performed in low- and high-volume surgical units, respectively. Esophagectomy at low-volume hospitals was associated with a significant increase in incidence of in-hospital (8.48% vs. 2.82%; pooled odds ratio (POR) = 0.29; P < 0.0001) and 30-day mortality (2.09% vs. 0.73%; POR = 0.31; P < 0.0001). There was insufficient data for conclusive statistical analysis of length of hospital stay or post-operative complications.
Conclusions
This meta-analysis does suggest a benefit in the centralization of esophageal cancer surgery to high-volume institutions with respect to mortality. The outcomes of this study are of interest to patients, healthcare providers and payers, particularly regarding service reconfiguration and more specifically centralization of services. Future studies that look at long-term survival will help improve understanding of any late consequences such as survival and quality of life following esophageal surgery at low- and high-volume hospitals.






Similar content being viewed by others
References
Jamieson GG, Mathew G, Ludemann R, Wayman J, Myers JC, Devitt PG. Postoperative mortality following oesophagectomy and problems in reporting its rate. Br J Surg 2004; 91: 943–947
Kohn GP, Galanako JA, Meyes MO, Feins RH, Farrell TM. National trends in esophageal surgery—are outcomes as good as we believe? J Gastrointest Surg 2009; 13(11): 1900–10
Begg CB, Cramer LD, Hoskins WJ, Brennan MF. Impact of hospital volume on operative mortality for major cancer surgery. JAMA 1998; 280: 1747–51.
Birkmeyer JD, Sun Y, Wong SL, Stukel TA. Hospital volume and late survival after cancer surgery. Ann Surg 2007; 245: 777–783
Finalyson EV, Goodney PP, Birkmeyer JD. Hospital volume and operative mortality in cancer surgery: a national study. Arch Surg 2003; 138: 721–5
Gillison EW, Powell J, McConkey CC, Spychal RT. Surgical workload and outcome after resection for carcinoma of the oesophagus and cardia. Br J Surg 2002; 89: 344–8.
Lauder CIW, Marlow NE, Maddern GJ, Barraclough B, Collier NA, Dickenson IC, Fawcett J, Graham JC. Systematic review of the impact of volume on oesophagectomy and patient outcome. ANZ J Surg 2010; 80: 317–323
Metzger R, Bollschweiler E, Vallbohmer D, Maish M, DeMeester TR, Holscher AH. High volume centers for esophagectomy: what is the number needed to achieve low postoperative mortality? Dis Eso 2004; 17: 310–314
The Leapfrog Group. Fact sheet. Available at: www.leapfroggroup.org
Massarweh NN, Flum DR, Symons RG, Varghese TK, Pellegrini CA. A critical evaluation of the impact of Leapfrog’s evidence-based hospital referral. J Am Coll Surg 2011; 212(2): 150–159
Oxford Centre for Evidence-based Medicine Levels of Evidence (2009). Oxford, UK
DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials 1986; 7: 177–188
Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Sta Med 2002; 21: 1539–1558
Bilimoria KY, Bentrem DJ, Talamonti MS, Stewart AK, Winchester DP, Ko CY. Risk-based selective referral for cancer surgery: a potential strategy to improve perioperative outcomes. Ann Surg 2010; 251(4): 708–716
Birkmeyer JD, Sun Y, Goldfaden A, Birkmeyer NJ, Stukel TA. Volume and process of care in high-risk cancer surgery. Cancer 2006; 106(11): 2476–81
Al-Sariria AA, David G, Willmott S, Slavin JP, Deakin M, Corless DJ. Oesophagectomy practice and outcomes in England. Br J Surg 2007; 94(5): 585–91
Funk LM, Gawande AA, Semel ME, Lipsitz SR, Berry WR, Zinner MJ, Jha AK. Esophagectomy outcomes at low-volume hospitals: the associated between systems characteristics and mortality. Ann Surg 2011; 253(5): 912–7
Fujita H, Ozawa S, Kuwano H, Ueda Y, Hattori S, Yanagawa T, Committee for Scientific Affairs, Japanese Association for Thoracic Surgery. Esophagectomy for cancer: clinical concerns support centralizing operations within the larger hospitals. Dis Esophagus 2010; 23(2): 145–52
Committee for Scientific Affairs, Kazui T, Osada H, Fujita H. An attempt to analysis the relation between hospital surgical volume and clinical outcome. Gen Thorac Cardiovasc Surg 2007; 55(12): 483–92
Lin HC, Xirasagar S, Lee HC, Chai CY. Hospital volume and inpatient mortality after cancer-related gastrointestinal resections: the experience of an Asian country. Ann Surg Oncol 2006; 13(9): 1182–8.
Reavis KM, Smith BR, Hinojosa MW, Nguyen NT. Outcomes of esophagectomy at academic centers: an association between volume and outcome. Ann Surg 2008; 74(10): 939–43
Stavrou PE, Smith SG, Baker DF. Surgical outcomes associated with oesophagectomy in New South Wales: an investigation of hospital volume. J Gastrointest Surg 2010; 14(6): 951–7
Suzuki H, Gotoh M, Sugihara K, Kitagawa Y, Kimura W, Kondon S, Shimada M, Tomita N, Nakagoe T, Hashimoto H, Baba H, Miyata H, Motomura N. Nationwide survey and establishment of a clinical database for gastrointestinal surgery in Japan: targeting integration of a cancer registration system and improving the outcome of cancer treatment. Cancer Sci 2011; 102(1): 226–30
Wouters MW, Karim-Kos HE, le Cessie S, Wijnhoven BP, Stassen LP, Steup WH, Tilanus HW, Tollenaar RA. Centralization of esophageal cancer surgery: does it improve clinical outcome? Ann Surg Oncol 2009; 16(7): 1789–98
Auerbach AD, Maselli J, Carter J, Pekow PS, Lindernauer PK. The relationship between case volume, care quality, and outcomes of complex cancer surgery. J Am Coll Surg 2010; 211(5): 601–8
Kuo EY, Chang Y, Wright CD. Impact of hospital volume on clinical and economic outcomes for esophagectomy. Ann Thorac Surg 2001; 72(4): 1118–24
Padmanabhan RS, Byrnes MC, Helmer SD, Smith RS. Should esophagectomy be performed in a low-volume center? Ann Surg 2002; 68(4): 348–51
Yasunaga H, Matsuyama Y, Ohe K; Japan Surgical Society. Effects of hospital and surgeon case-volumes on post-operative complications and length of stay after esophagectomy in Japan. Surg Today 2009; 39: 566–571
Rutegard M, Lagergren J, Rouvelas I, Lagergren P. Surgeon volume is a poor proxy for skill in esophageal cancer surgery. Ann Surg 2009; 249(2): 256–261
Kruijshaar ME, Essink-Bot ML, Donkers B, Looman CW, Siersema PD, Steyerberg EW. A labeled discrete choice experiment adds realism to the choices presented: preferences for surveillance tests for Barrett esophagus. BMC Med Res Methodol 2009; 9: 31.
Thrumurthy SG, Morris JJA, Mughal MM, Ward JB. Discrete-choice preference comparison between patients and doctors for the surgical management of oesophagogastric cancer. Br J Surg 2011; 98(8):1124–1131
Acknowledgements
This work was supported in part by the Ryan Hill Research Foundation.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Markar, S.R., Karthikesalingam, A., Thrumurthy, S. et al. Volume-Outcome Relationship in Surgery for Esophageal malignancy: Systematic Review and Meta-analysis 2000-2011. J Gastrointest Surg 16, 1055–1063 (2012). https://doi.org/10.1007/s11605-011-1731-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-011-1731-3