Abstract
Background
Radiocarpal dislocations are rare, high-energy injuries. High morbidity and poor functional outcomes are common. Currently, there is limited data on functional outcomes following treatment of this injury.
Methods
A retrospective review was conducted analyzing the radiographic and clinical outcome of patients treated for a radiocarpal dislocation from 1979 to 2010. Outcome assessments included wrist range of motion, grip strength, Mayo wrist score, patient-rated wrist evaluation (PRWE), and disabilities of the arm, shoulder and hand (DASH) score. Statistical analysis was performed with the Student’s t test.
Results
Twenty-six patients (26 wrists) were treated for a radiocarpal dislocation during the study period; 23 wrists were treated acutely (within 4 weeks of injury), and 3 were treated after a delayed presentation (>4 weeks). Clinical follow-up of more than 6 months was available in 17 patients. Three patients (12 %) underwent primary fusion as initial treatment (two radioscapholunate fusion; one total wrist fusion). Four wrists (24 %) failed initial treatment and were salvaged with scapholunate ligament reconstruction (one wrist) or partial wrist fusion (three wrists). Seventeen patients completed PRWE and DASH questionnaires with a mean of 14.6 years following surgery (range 2–32 years). Subjective outcomes tended to be superior in those patients treated with ligament reconstruction versus partial or complete wrist fusion; however, comparisons were not statistically significant.
Conclusion
Radiocarpal dislocations result in significant osseous and ligamentous injury to the distal radius and carpus. Early recognition and treatment of radiocarpal dislocations with open reduction, internal fixation, and repair of ligaments may result in improved long-term functional outcomes when compared to acute partial or complete wrist arthrodesis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Radiocarpal dislocations represent rare, high-energy injuries to the carpus. Unlike marginal rim articular fractures of the distal radius, which were originally described by Barton [2], radiocarpal dislocations represent a severe crush or rotational injury to the carpus that results in intercarpal supination and subsequent disruption of the stout radiocarpal ligaments [7]. Common mechanisms of injury include high-speed motor vehicle accidents, falls from height, and industrial injuries [5].
Treatment of these injuries is often complex as severe soft tissue injuries, open fractures, and associated multi-system trauma are common [5]. Anatomic studies have identified the short radiolunate ligament and radioscaphocapitate ligament to be the primary stabilizers of the carpus in resisting volar and ulnar translocation, respectively [3]. Previous reports have emphasized the importance of anatomic restoration of these structures to prevent late instability and posttraumatic arthrosis [5, 6].
Most historical descriptions of this injury are in the form of case reports or small case series with short or incomplete follow-up. This study is clinical and radiographic review of patients who underwent treatment for a traumatic radiocarpal dislocation. We attempted to define the functional outcomes of these patients through use of validated outcome scores. Secondarily, we attempted to correlate patient or injury characteristics to long-term clinical outcomes.
Materials and Methods
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008. Informed consent was obtained from all patients for being included in the study. This study was performed at a level 1 trauma hospital and associated tertiary referral clinic. We retrospectively reviewed the operative records at our institution for all patients undergoing surgical treatment for a radiocarpal dislocation from 1979 to 2010. We searched an electronic database of all operative records containing a diagnosis of radiocarpal dislocation. Patients with radiographs documenting complete dissociation of the proximal row of the carpus from the radius were included in the study. Associated intercarpal dislocations or associated distal radial metaphyseal fractures were not a reason for exclusion as long as the scaphoid and lunate were completely dissociated from the articular surface of the distal radius. Specifically, we did include patients with a fracture of the radial styloid as long as the ulnar 50 % of the distal radius was intact [5]. Patients without complete clinical records were excluded. Injury patterns that were associated with a fracture of the volar or dorsal margin of the radius (Barton fracture) were excluded [2].
Demographic data was collected. Injury radiographs were analyzed for the direction of dislocation and associated distal radius, radial styloid, or carpal fracture. Severity of the associated soft tissue injury was noted from the medical record. Information regarding the method of reduction and fixation, type of surgical approach (dorsal, palmar, or both), associated injuries, salvage procedures, and complications was recorded.
Postoperative grip strength using a dynamometer (Jamar dynamometer, Cambridge, MA) and range of motion (wrist flexion, extension) were recorded from the patients’ charts. Postoperative Mayo wrist scores (score of 100–90 is excellent, 89–80 is good, 79–65 is fair, and less than 65 is poor) were calculated from the patients’ charts [1].
Posteroanterior and lateral radiographs at the time of injury, immediately postoperative and at the last follow-up were analyzed by an independent observer [11]. The direction of dislocation and associated fractures were noted from injury radiographs. Immediate and latest postoperative radiographs were analyzed, and the modified carpal height ratio [9] as well as the degree of ulnar translocation of the carpus were recorded [4].
After the retrospective review was completed, all patients that confirmed to have a radiocarpal dislocation treated between 1979 and 2010 were contacted through mail to fill out and return two questionnaires: the disabilities of the arm, shoulder, and hand (DASH) and patient-rated wrist evaluation (PRWE). The patients were not asked to return for previously unscheduled clinical follow-up or radiographs at that time.
Statistical Analysis
Association between injury characteristics and treatment variables with follow-up wrist scores were investigated using linear regression models. All tests were two-sided, and p value <0.05 was considered significant. No power analysis was performed a priori.
Results
Twenty-six patients were treated for acute or delayed traumatic radiocarpal dislocation between 1979 and 2010. There were no bilateral injuries. Mean age at time of injury was 39 years (range 19–73 years old) and 23 of 26 patients were male (88 %). Sixteen of 26 injuries (62 %) involved the dominant upper extremity. One patient out of 26 (4 %) sustained a volar radiocarpal dislocation; the remaining twenty-five dislocations were dorsal. Seventeen of the 26 wrists (65 %) presented with a concomitant distal radius fracture, which was defined as a fracture involving more than one third of the scaphoid fossa of the radial styloid. Three out of 26 patients (12 %) presented to our institution at least 4 weeks from the date of injury with an unrecognized or untreated radiocarpal dislocation.
Primary Treatment Modalities
One patient was initially treated with external fixation and subsequently expired of complications from a severe spinal cord injury within 4 weeks, before further surgical intervention for the wrist was performed. Thirteen of 26 wrists (50 %) underwent an attempt at primary ligament repair as initial treatment (Fig. 1, Table 1). Eight out of 13 of these wrists presented with a distal radius fracture that was treated at the time of ligament repair. Ligament repair was performed through a combined dorsal and volar approach in 11 of 13 wrists, volar only in 1 wrist, and dorsal only in 1 wrist. The patient who underwent a dorsal-only approach had a radiostyloid fracture which involved more than one third the width of the scaphoid fossa of the distal radius. The wrist was noted to be stable after repair of the dorsal radiocarpal ligaments and percutaneous pinning of the styloid process; thus, a volar approach was not performed.
Injury (a) and 1-year postoperative (b) radiographs of a patient treated for a radiocarpal dislocation by open reduction and percutaneous pinning of the radial and ulnar styloid with ligament repair via suture anchors. The patient’s PRWE and DASH scores at 4 years after injury were 7 and 4, respectively
Percutaneous pinning to stabilize the radiocarpal articulation without primary ligament repair was performed in 6 of 26 wrists (23 %) (Fig. 2). Three out of six of these injuries were severe, open crush, and/or degloving type injuries with soft tissue loss precluding an immediate attempt at ligament repair. These injuries were temporarily stabilized with percutaneous pins as part of staged soft tissue reconstruction. One patient required a groin flap for dorsal and radial soft tissue injury, a second patient required a dorsal rotational flag flap for the first webspace soft tissue loss with full-tickness skin grafting, and the third patient required a rectus abdominus flap for soft tissue loss. The remaining three wrists did not have a soft tissue injury that precluded primary ligament repair but were treated with percutaneous pinning of a large radial styloid fracture (two wrists) or with reduction and temporary pin fixation across the radiocarpal articulation.
Injury (a) and postoperative (b) radiographs of a patient treated for a radiocarpal dislocation by open reduction with percutaneous pinning. Two-year follow-up (c) radiographs demonstrate severe degenerative changes. The patient’s PRWE and DASH scores at 5 years after injury were 17 and 19, respectively
Three patients (12 %) underwent primary fusion as initial treatment (two radioscapholunate fusion and one total wrist fusion). In each case, the treating surgeon cited severe destruction of large areas of articular cartilage as the indication for primary fusion. Two of these injuries were open, one was also a volar radiocarpal dislocation, and another was associated with a brachial plexopathy as part of a severe traction and crush injury to the involved extremity.
The remaining three patients presented with an untreated or unrecognized radiocarpal dislocation at least 4 weeks from the time of injury. The first patient had been treated in a long arm cast for 6 weeks for a “wrist fracture.” The patient presented to our institution 10 months after injury, and radiographs revealed a small radial styloid fracture (less than one third of the scaphoid fossa) with severe ulnar translocation of the carpus, DISI deformity, and secondary radiocarpal arthritis. This patient was treated with proximal row carpectomy 10 months after the original injury. Another patient presented with wrist pain after ORIF of a distal radius fracture at another institution 6 months prior. Dorsal and ulnar carpal subluxation with degenerative changes were noted, and a radiocarpal dislocation was suspected. The patient declined further surgical treatment. A third patient was treated at another institution for a distal femur fracture and placed into a splint for a “wrist injury.” They presented to our institution 4 months after the initial injury with continued wrist pain, radiographs revealed dorsal and ulnar subluxation of the carpus with severe secondary arthritic changes. This patient was treated with radioscapholunate fusion 4.5 months after the original injury.
Follow-Up
Clinical follow-up was available for 17 of 26 wrists at a minimum of 6 months from the date of surgery; one patient expired of a concomitant traumatic spinal cord injury 4 weeks after injury and another eight patients were lost to follow-up. The mean clinical follow up was 2.8 years (range 6 months to 14.2 years). The average Mayo wrist score at the last follow-up was 64 (range 50 to 80). Mean flexion to extension arc was 76° (range 20° to 135°), and mean grip strength was 68 % (range 38 to 113 %) of the uninjured side at 30 kg (range 14 to 48 kg). Thirteen patients (76 %) had returned to gainful employment.
Complete radiographic follow-up at a minimum of 6 months was available for 14 patients at a median of 15 months (range 6 months to 28.6 years). At the time of most recent radiographs, 4 of the 13 (31 %) wrists that had not already undergone partial or total wrist fusion had evidence of moderate to severe posttraumatic arthrosis (Fig. 3). Three of 13 wrists (23 %) also had progressive ulnar subluxation of the carpus, as measured by a Bouman ratio of less than 0.83 [4]. There was no change in the modified carpal height ratio from the immediate postoperative radiographs to the last follow-up (0.66 and 0.69, respectively) [9].
Salvage Procedures
Salvage procedures were performed on 4 of 17 wrists available for follow-up (24 %). Two wrists had presented greater than 4 weeks after injury and were treated with RSL fusion and PRC 4 and 10 months after injury, respectively. One wrist, which was initially treated with percutaneous pinning only due to a severe open crush-type injury, was salvaged with a radiocarpal fusion 2 months after injury. One wrist initially treated with ligament repair through a combined volar and dorsal approach had subsequent scapholunate instability and underwent scapholunate ligament repair with dorsal capsulodesis 5 weeks after initial treatment.
Clinical Follow-Up
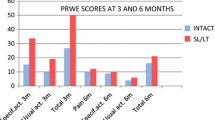
Seventeen patients completed and returned a survey questionnaire including DASH and PRWE at a mean of 14.8 years (range 2 to 32 years) after initial surgical treatment. The mean PRWE score was 15 (range 0–61), and the DASH score was 12 (range 0–32). The PRWE and DASH scores according to injury characteristics and method of initial treatment are shown in Table 2. Those patients that underwent acute open reduction and ligament repair or reconstruction tended to report lower PRWE and DASH scores than patients that underwent open reduction and percutaneous stabilization without ligament repair or acute arthrodesis. Similarly, those patients that presented in a delayed fashion and required salvage procedures tended to have higher PRWE and DASH scores. The clinical outcome scores tended to be similar between those patients that presented with a distal radius fracture and those that did not. However, none of these comparisons reached statistical significance (all p values >0.1).
Discussion
Radiocarpal dislocations represent a spectrum of severe injury to the carpus and distal forearm. They are often associated with a variety of severe soft tissue injuries and open fractures to the metacarpals, digits as well as distal radius and ulna. This is represented in our series of patients, as some patients were treated with acute arthrodesis or external fixation and pinning in anticipation of free tissue transfer, and others presented as missed injuries that had been treated with closed reduction and immobilization similar to a distal radius fracture. Given the rarity of this injury and the wide spectrum of injury, statistical comparisons between treatment approaches are difficult to interpret. Our small numbers with limited follow-up and the heterogenous nature of the patient population in regard to injury severity and type of treatment were the primary weakness of this study. In order to make conclusions about treatment for radiocarpal dislocations, we would have required more patients with more complete follow-up. However, this represents a very rare and severe injury that does not lend itself to a standardized treatment algorithm. To our knowledge, ours is the only series of patients treated for radiocarpal dislocation followed long-term with validated clinical outcome measures.
Previous studies have demonstrated that persistent ulnar translation of the carpus is the predictable consequence of an avulsive injury to the volar radiocarpal ligaments, specifically the radioscaphocapitate and radiolunate ligaments [5, 10]. We observed progressive ulnar translocation of the carpus in 23 % (3 of 13) of the patients with radiographic follow-up. Rates of posttraumatic arthrosis reported in the literature have ranged from 11–25 % [5, 8], consistent with our observed rate of 31 % (4 out of 13 wrists).
Dumontier classified radiocarpal fracture dislocations into two groups, based on the perceived integrity of the volar radiocarpal ligaments [5]. Group 1 was defined as radiocarpal dislocations without a fracture of the distal radius or with only a fracture of the tip of the radial styloid, representing avulsion or tearing of the volar radiocarpal ligaments. These injuries were rare in their series, representing only 3 of 27 cases. Group 2 included patients with a fracture through more than one third of the width of the scaphoid fossa, leaving the volar radiocarpal ligaments intact to the fractured styloid fragment. The authors recommended ligamentous repair in group 1 injuries and anatomic reduction with fixation of the styloid fragment in group 2 injuries. In theory, injuries with intact volar radiocarpal ligaments would heal more predictably and lead to less risk of progressive ulnar subluxation of the carpus and posttraumatic arthrosis. In this cohort, 17 of 26 injuries were associated with a distal radial styloid fracture. We observed no significant difference in long-term outcome of patients who presented with or without a distal radius fracture, inconsistent with prior reports, which likely was due to insufficient power to detect this difference. Many wrists in this cohort with an associated distal radius fracture represented a high-energy mechanism of injury that may have contributed to a worse outcome as well.
Additionally, there was a trend toward improved long-term outcomes in wrists treated with primary ligament repair; however, these wrists likely represent a subgroup of injuries that may have been less severe than those that were treated with percutaneous pinning only or those treated with acute arthrodesis. The indication for percutaneous pinning only was often a severe open or crush injury, and for fusion was severe irreparable damage to articular cartilage. These naturally represent a more severe pattern of injury to the entire upper extremity, which may also lead to impaired long-term outcomes. Either way, the rarity of radiocarpal dislocation did not allow these trends to reach significance.
Radiocarpal dislocations result from severe, high-energy injury to the carpus. As a result, treatment must first take into account the nature of the entire injury to the involved upper extremity and patient, including neurologic, vascular, soft tissue and bony injury. Surgical treatment should be directed initially at stabilization and soft tissue coverage as necessary. If possible, any associated distal radius or radial styloid fracture should be treated appropriately with internal fixation, followed by repair of the volar radiocarpal ligaments. Our study demonstrates the wide spectrum of trauma to the bone, carpal ligaments, and surrounding soft tissue associated with this injury. As expected, we observed a high rate of posttraumatic arthrosis; however, despite the often poor radiographic outcome, we observed that good long-term outcomes can be obtained when these injuries are recognized and treated appropriately in the acute setting. Larger studies with more homogenous injury patterns are necessary to make meaningful comparisons between treatment modalities.
References
Amadio PC, Berquist TH, Smith DK, Ilstrup DM, Cooney 3rd WP, Linscheid RL. Scaphoid malunion. J Hand Surg [Am]. 1989;14:679–87.
Barton J. Views and treatment of an important injury of the wrist. Med Examiner Rec Med Sci. 1838;1:365–8.
Berger RA, Landsmeer JM. The palmar radiocarpal ligaments: a study of adult and fetal human wrist joints. J Hand Surg [Am]. 1990;15:847–54.
Bouman HW, Messer E, Sennwald G. Measurement of ulnar translation and carpal height. J Hand Surg (Br). 1994;19:325–9.
Dumontier C. Meyer zu Reckendorf G, Sautet A, Lenoble E, Saffar P, Allieu Y. Radiocarpal dislocations: classification and proposal for treatment. A review of twenty-seven cases. J Bone Joint Surg Am. 2001;83-A:212–8.
Ilyas AM, Mudgal CS. Radiocarpal fracture-dislocations. J Am Acad Orthop Surg. 2008;16:647–55.
Mayfield JK, Johnson RP, Kilcoyne RK. Carpal dislocations: pathomechanics and progressive perilunar instability. J Hand Surg [Am]. 1980;5:226–41.
Mudgal CS, Psenica J, Jupiter JB. Radiocarpal fracture-dislocation. J Hand Surg (Br). 1999;24:92–8.
Nattrass GR, King GJ, McMurtry RY, Brant RF. An alternative method for determination of the carpal height ratio. J Bone Joint Surg Am. 1994;76:88–94.
Rayhack JM, Linscheid RL, Dobyns JH, Smith JH. Posttraumatic ulnar translation of the carpus. J Hand Surg [Am]. 1987;12:180–9.
Yang Z, Mann FA, Gilula LA, Haerr C, Larsen CF. Scaphopisocapitate alignment: criterion to establish a neutral lateral view of the wrist. Radiology. 1997;205:865–9.
Conflict of Interest
Sanjeev Kakar has received royalties from Arthrex (Naples, FL) and is a paid consultant for Arthrex and Skeletal Dynamics (Miami, FL).
David G. Dennison receives research support from DePuy (Warsaw, IN).
Bassem T. Elhassan has no conflicts to disclose.
Brandon J. Yuan has no conflicts to disclose.
Statement of Human and Animal Rights
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008.
Statement of Informed Consent
Informed consent was obtained from all individual participants included in the study.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Yuan, B.J., Dennison, D.G., Elhassan, B.T. et al. Outcomes after radiocarpal dislocation: a retrospective review. HAND 10, 367–373 (2015). https://doi.org/10.1007/s11552-014-9736-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11552-014-9736-5