Abstract
Background
Posttraumatic wrist osteoarthritis is an irreversible and often progressive condition. Many surgical treatments, used in (daily) practice, aim to relieve symptoms like pain and restore function. The aim of this systematic review is to assess the patient reported and functional outcomes of the most common surgical interventions in patients with posttraumatic wrist osteoarthritis. This overview can help clinicians select the best treatment and manage patient’s expectations.
Methods
A literature search was performed in Pubmed, Embase and Cochrane for articles published between 1990 and November 2022 according to the PRISMA guidelines. The study protocol has been registered in the PROSPERO database (CRD42017080427). Studies that describe patient reported outcomes (pain and Disability of Arm, Shoulder and Hand (DASH) –score) and functional outcomes (range of motion (ROM) and grip strength) after surgical intervention with a minimal follow-up of 1 year were included. The identified surgical procedures included denervation, proximal row carpectomy, interpositional- and total arthroplasty, and midcarpal-, radiocarpal- and total arthrodesis. The pre-and postoperative outcomes were pooled and presented per salvage procedure.
Results
Data from 50 studies was included. Pain score improved after all surgeries except denervation. Flexion/extension decreased after radiocarpal arthrodesis, did not show significant changes after proximal row carpectomy, and improved for all other surgeries. DASH score improved after arthroplasty, proximal row carpectomy and midcarpal arthrodesis. Grip strength improved after interposition arthroplasty and partial arthrodesis.
Conclusion
Evidence from this review did not support the indication for denervation in this particular patient population. In patients with SLAC/SNAC II, proximal row carpectomy might be favourable to a midcarpal arthrodesis solely based on better FE ROM of the radiocarpal joint after proximal row carpectomy. In terms of radiocarpal mobility, total wrist arthroplasty might be preferred to radiocarpal arthrodesis in patients with osteoarthritis after a distal radius fracture. More uniform measurements of outcomes would improve the understanding of the effect of surgical treatments of the posttraumatic osteoarthritic wrist.
Similar content being viewed by others
Introduction
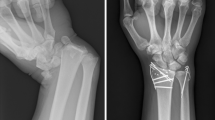
Posttraumatic wrist osteoarthritis is an irreversible and often progressive condition. It commonly occurs secondary to fractures of either the distal radius or the carpal bones or secondary to ligamentous disruption of the radiocarpal or intercarpal joints. [1,2,3]. At the radial side of the radiocarpal joint, osteoarthritis can occur secondary to a distal radius fracture in which the cartilage covering the radius is damaged [4, 5]. Although more frequently seen after intra-articular fractures, osteoarthritis can also occur after extra-articular fractures.
At the carpal side of the radiocarpal joint, wrist osteoarthritis occurs mostly secondary to either a scaphoid nonunion advanced collapse (SNAC) or a scapholunate advanced collapse (SLAC) of the proximal carpal row. [5,6,7] Both the scaphoid nonunion and scapholunate ligamentous injury potentially lead to alteration of the kinetics of the proximal carpal row. The altered biomechanics cause a predictive pattern of osteoarthritis, starting at the radial styloid and progressing to the scaphoid fossa and midcarpal joints. [6, 8, 9]
Osteoarthritis of the wrist can eventually lead to severe pain and functional impairment [9]. The primary goal of treatment is to decrease pain. The secondary goal is to preserve a functional range of motion and stability of the affected wrist [10]. Patients with radiocarpal osteoarthritis can frequently be helped by nonsurgical interventions. The use of immobilizing casts, non-steroidal anti-inflammatory drugs or intra-articular injections of corticosteroids may enable and improve functional use of the wrist by decreasing pain. Surgery is indicated only when non-surgical treatment fails [3, 6,7,8]. Numerous techniques have been proposed, including denervation, excisional arthroplasties, partial or total wrist arthrodesis and partial or total wrist arthroplasties. The choice of surgery depends heavily on the patient’s occupational and functional demands and the degree of wrist osteoarthritis [7, 8, 11].
Numerous retrospective single-centre cohort studies describing a plethora of surgical techniques for treating the osteoarthritic wrist have been published. Additionally, multiple systematic reviews and comparative studies describing outcomes after various wrist salvage procedures have been published [12,13,14,15]. However, these studies do not describe the outcomes exclusively for posttraumatic wrist osteoarthritis patients. Although the incidence of posttraumatic wrist osteoarthritis is unknown, it is becoming a more frequent and challenging problem in today’s demanding patient population. An overview of patient reported and functional outcomes per surgery could help manage a patient’s expectations and help select the best surgical treatment for each specific patient. Therefore, the aim of this study is to systematically review the literature on patient reported and functional outcomes for the most frequently described surgical techniques for treating posttraumatic wrist osteoarthritis.
Methods
This study was performed according to Preferred Reporting Items for Systematic review and Meta-Analyses (PRISMA) [16]. The study protocol has been registered in the PROSPERO database (CRD42017080427).
Data sources and searches
Electronic databases Pubmed, OVID Embase and Cochrane Central were systematically searched to find eligible studies covering January 1st 1990 until November 15th 2022. Studies published before 1990 were excluded since outcomes from surgical salvage procedures performed before 1990 only have historical value. Studies that described patient reported and functional outcomes after surgical salvage procedures for patients with posttraumatic wrist osteoarthritis with a minimal follow-up of 12 months were included. Studies written in a language other than English, Dutch, German or French were excluded. Furthermore, a manual search of the reference lists of the included full-text studies was performed. The detailed search strategy can be found in Additional Table S1.
Eligibility criteria
Studies were included if 1) the patients were adults (18 years or older), 2) have undergone surgical salvage procedure for posttraumatic radiocarpal joint osteoarthritis (e.g., SNAC ≥II, SLAC ≥II, distal radius fracture) and 3) patient reported and functional outcome measures of interest (e.g., pain score (Visual Analogue Scale (VAS)), Disability Arm, Hand and Shoulder (DASH) score, flexion/extension (FE) and ulnar/radial deviation (RU) range of motion (ROM) and grip strength) with a minimal follow-up of 12 months were described.
Studies which included SNAC I, SLAC I or non-posttraumatic radiocarpal osteoarthritis such as rheumatoid arthritis or Kienbock’s disease were excluded if data of these patients could not be separated. Studies describing both posttraumatic radiocarpal osteoarthritis, secondary surgeries and non-posttraumatic radiocarpal osteoarthritis were only included when data were separately presented per patient (group). Finally, biomechanical and cadaveric studies, case studies (n<3), (systematic) reviews, meta-analyses and congress abstracts were excluded.
Study selection
Eligible studies were imported into the Covidence systematic review software (Veritas Health Innovation, Melbourne Australia, available at www.covidence.org). Duplicates were removed by the Covidence software. Two reviewers (J.G., P.S.) independently evaluated titles and abstracts in a standardized blinded way. Inconsistencies were resolved by a consensus discussion. Uncertainty or unresolved disagreements were resolved by a third reviewer (I.P.). In case the title and abstract provided insufficient information to either in or exclude the study, the full-text was accessed and assessed for inclusion.
Next, eligible full-text studies were imported into the Covidence systematic review software and evaluated by two reviewers (J.G., P.S.).
Data extraction
Three reviewers (J.G., P.S. or I.P.) independently extracted data using a standardized form created using Microsoft Access 2013 in a blinded manner. Inconsistencies were resolved in a consensus discussion. Uncertainty or unresolved disagreements were resolved by a third reviewer (P.S. or I.P.). The following information was collected: general study information (first author, year of publication, study design, country of study), type of surgical salvage procedure, participant characteristics at baseline (age, sex, diagnosis), patient reported and functional outcome measures of interest, unit of measurements and duration of follow-up. If data were missing, the corresponding author was contacted via e-mail (including one reminder). If the data was not provided, the study or a specific aspect of the study was excluded.
Risk of bias assessment
The risk of bias of the included studies was independently evaluated by two reviewers (J.G., P.S.) using the validated Methodological Index for Non-Randomized Studies (MINORS) score (criteria 1-8) [17]. The items on the questionnaire were scored as not reported (0), reported but inadequate (1) or reported and adequate (2). With a maximum score of 16, the studies were rated as high (<8), moderate (8-12) or low risk of bias (>12). Conflicts in rating were resolved during a consensus meeting. A third reviewer (I.P.) was available to resolve any remaining disagreements.
Data analysis
The outcomes of patient reported and functional measures were pooled using common-effects meta-analysis techniques stratified by surgery. Pre- and postoperative means were calculated for each functional outcome. As studies generally did not contribute head-to-head comparisons of pre-and postoperative scores, t-values and associated p-values were computed. As the correlation between pre- and postoperative scores was unknown, our test statistics can be regarded as conservative; actual p-values would be lower given a positive correlation between scores. A significance level of 0.05 and a confidence level of 0.95 were used. For patients with a SNAC or SLAC grade II, the most commonly performed surgical salvage procedure is proximal row carpectomy or midcarpal arthrodesis [18]. Multiple systematic reviews and meta-analyses have been performed to compare the outcomes of these surgical procedures. Some of these studies either failed to specify the degree of SLAC or SNAC or they included patients with a SLAC or SNAC grade III. Therefore, a sub-analysis of patients with SNAC or SLAC grade II after proximal row carpectomy and midcarpal arthrodesis is described separately.The pre-and postoperative difference in patient reported and functional outcomes were also compared with the Minimum Clinically Important Difference (MCID). The MCID is the smallest change in a treatment outcome that an individual patient would identify as important and which would indicate a change in the patient's management. If the found pre- and postoperative difference is larger than the MCID, we consider this difference clinically relevant. No MCID for the VAS score, DASH score and grip strength has been specifically described for wrist salvage procedures. To provide some perspective, we refer to MCID found in literature that was calculated in postoperative upper extremity populations. According to Randall et al., the MCID for the VAS score in a population undergoing non-shoulder, hand and upper extremity surgery ranges from 16 and 19 [19]. For the DASH score, the MCID is 10 according to Gummesson et al. in a population with patients who received surgery for upper extremity musculoskeletal conditions [20]. Additionally, Kim et al. presented a MCID for grip strength of 19.5% of the unaffected wrist in a patient population that received a volar plate fixation to treat a distal radius fracture [21].
Results
Search results
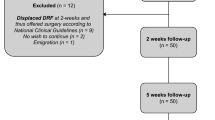
A total of 951 studies were identified in all databases, which resulted in 837 studies for screening after duplicate removal. After evaluating the abstracts, 269 full text studies were examined and 50 studies were included in the systematic review (see Fig. 1).
Study characteristics
The studies were divided by the performed surgery (denervation (n=4), proximal row carpectomy (n=10), interposition arthroplasty (n=2), total arthroplasty (n=2), total arthrodesis (n=1) and partial arthrodesis divided in midcarpal (n=25) and radiocarpal arthrodesis (n=10)). Characteristics and outcome measures of all studies per surgery can be found in Tables 1 and 2.
Risk of bias
All included studies demonstrated a moderate or low risk of bias. The scores for each individual study can be found in Additional Table S2.
Participants
The diagnoses of the included patients per surgery are presented in Additional Table S3. Proximal row carpectomy, interposition arthroplasty and midcarpal arthrodesis were mainly performed in patients with SNAC/SLAC with a grade II/III. Total wrist arthroplasty was performed in both grade III or IV SNAC/SLAC and secondary to distal radius fractures. Radiocarpal arthrodesis was mainly performed in osteoarthritic wrists secondary to distal radius fractures. Denervation was performed in all of the above-mentioned diagnoses.
Patient reported and functional outcomes
The pooled pre- and postoperative data, number of included studies and wrists per surgical procedure can be found in Additional Table S4. The MCID and difference between pre-and postoperative mean of VAS score, DASH score and grip strength are presented in Table 3.
Denervation
The weighted mean ROM FE and RU decreased (p<0.02), and the VAS score showed no significant change after denervation (p>0.05) (Fig. 2). No grip strength and only postoperative DASH scores were reported.
Interposition arthroplasty
All patient reported and functional outcome weighted means improved (p<0.01), except for ROM RU which showed no significant change (p>0.05) after interposition arthroplasty (Fig. 3). The differences in pre- and postoperative patient reported outcomes were clinically relevant. However, the difference in pre-and postoperative grip strength was not clinically relevant.
Total arthroplasty
The weighted mean of the patient reported outcomes both decreased (p<0.01) and are clinically relevant (Fig. 4). The weighted mean ROM FE and RU increased (p<0.01). There were no DASH scores available.
Proximal row carpectomy
The weighted mean VAS score and DASH score improved after proximal row carpectomy (p<0.01) (Fig. 5). The difference in pre- and postoperative patient reported outcomes was clinically relevant. Additionally, the ROM FE and RU showed no significant change (p>0.05). Only post-surgery grip strength was reported.
Midcarpal arthrodesis
The weighted mean of all patient reported and functional outcomes improved after midcarpal arthrodesis (p<0.01) (Fig. 6). The difference between pre-and postoperative VAS score, DASH score and grip strength was clinically relevant.
Radiocarpal arthrodesis
The weighted mean VAS score, ROM FE decreased and the grip strength increased after radiocarpal arthrodesis (p<0.01) (Fig. 7). The improvement between pre- and postoperative VAS score and grip strength were both considered clinically relevant. Furthermore, the ROM RU showed no significant change after surgery (p=1.00). There were no preoperative DASH scores reported.
Total arthrodesis
There was only one study that reported the postoperative DASH score of patients after total arthrodesis (45.2 ±22.01). There are no other patient reported and functional outcomes available.
Sub-analysis
Finally, the sub-analysis of patient reported and functional outcomes for patients with SNAC or SLAC grade II undergoing proximal row carpectomy or midcarpal arthrodesis are presented in Fig. 8. Weighted mean VAS and DASH score improved (p<0.01) after both procedures and improvements were also clinically relevant. Weighted mean ROM improved significantly more after proximal row carpectomy (p<0.02) in 25 patients. Preoperative results for the grip strength were not reported. ROM and grip strength did not differ after midcarpal arthrodesis (p>0.05).
Pre- and postoperative weighted mean (with standard deviation) of patient reported and functional outcome measures for patients suffering from SNAC and SLAC grade II who underwent proximal row carpectomy or midcarpal arthrodesis. Number of patients on which the mean is calculated is depicted in the base of each bar
The pooled pre- and postoperative data of the sub-analysis for the four and five included studies for proximal row carpectomy and midcarpal arthrodesis respectively can be found in Additional Table S5.
Discussion
This systematic review critically appraises the available evidence of functional and patient reported outcomes for the most common surgical interventions for posttraumatic osteoarthritis of the wrist. The included main interventions were denervation, proximal row carpectomy, midcarpal arthrodesis, radiocarpal arthrodesis, total wrist arthrodesis, total wrist arthroplasty and excisional radiocarpal interposition arthroplasty. A plethora of different techniques are available for each of the main interventions. For example, in midcarpal arthrodeses, two, three or four different carpal bones can be fused. Moreover, the fixation technique for fusion differs from K-wire fixation to screw fixation to plate and screw fixation. Given the large heterogeneity in surgical techniques and the low patient numbers in most series, we pooled the different techniques of each of the stated main interventions. As a result of this systematic review, specific considerations related to various treatments of posttraumatic osteoarthritis of the wrist were identified.
In the included studies covering denervation, patients underwent either a total denervation or a partial denervation of the wrist. A previously performed systematic review by Smeraglia et al. concluded that both partial and total wrist denervation are safe and reliable procedures that provide substantial pain relief and preserve wrist motion [71]. In addition, both Boeckstyns et al. and Schmidt showed pain relief in over 70% of the patients with both non- and posttraumatic osteoarthritis [10, 72]. However, our review revealed no decrease in pain scores after denervation. The ROM in FE and RU did decrease in contrast to previous studies. The contrasting VAS and ROM scores between our study and the previously mentioned studies could be due to our strict selection of high quality studies which included posttraumatic patients only. For instance, many of the studies included in the review of Smeraglia, Boeckstyns and Schmidt were of low quality with a significant number of patients included with other pathologies than posttraumatic osteoarthritis. For example, denervations were performed in patients with Kienbock’s disease, patients with residual pain after partial arthrodesis, idiopathic wrist pain or after sprains of the wrist joint. The reported outcome measurements were not separately reported for the posttraumatic patient cohorts and therefore not included in the current review. Swärd et al. already indicated that posterior and anterior interosseous nerve denervation may not suffice in patients with SNAC/SLAC, since the posterior and anterior interosseous nerve innervate two-thirds of the central part of the joint while the pathological changes due to SNAC/SLAC (even in lower grades) are situated at the radial site of the joint [73]. In contrast to prior studies and based on the results of this review, some reluctance should be advised when considering denervation for patients with posttraumatic osteoarthritis of the wrist.
Both proximal row carpectomy and midcarpal arthrodesis are advocated in patients with SLAC or SNAC grade II. Even though proximal row carpectomy is unsuitable for patients with SNAC or SLAC grade III due to the involvement of the midcarpal joint [74], results from these patients or patients with unspecified SNAC or SLAC grade are often included in meta-analysis and systematic reviews. Including these patients can have an effect on the patient reported and functional outcomes, therefore, we only included patients with SNAC and SLAC grade II. Previous meta-analyses and systematic reviews reported that patient reported and functional outcomes were approximately the same after proximal row carpectomy and midcarpal arthrodesis [13, 15, 74,75,76]. If a significant difference was found between the two procedures such as in the study of Amer et al., then this difference in favour of proximal row carpectomy was very small (grip strength difference: 1.52%; VAS score difference: 3.0%) ) and not clinically relevant [75]. In order to preserve more grip strength after a PRC, some authors advocate to combine proximal row carpectomy with a resurfacing capitate pyrocarbon implant in order to maintain carpal height [77]. Although a number of series have been published combining proximal row carpectomy with resurfacing capitate pyrocarbon implant, only the study of Szalery et al. met the inclusion criteria of this review.
The subgroup analysis of patients with SLAC or SNAC grade II in this study showed that VAS and DASH scores improved after both procedures.
The FE ROM only improved after proximal row carpectomy. It should be noted that the midcarpal arthrodesis group includes a plethora of different carpal bone fusions by different techniques ranging from four-corner arthrodesis to limited carpal fusion techniques. Although ideally preferable, the existing literature is too scarce and absolute patient numbers are too small to perform a subgroup analysis for each specific technique. Therefore, one should be cautious when interpreting this subgroup analysis as other series found preferable results of limited carpal fusion over proximal row carpectomy [78]. In addition, we were not able to compare the follow-up between the surgical procedures since the exact follow-up of all included patients is not known. However, since some studies suggest that the subjective and functional outcomes after proximal row carpectomy stay stable over time [79, 80], we still think it is a relevant comparison. In our opinion, we prefer a proximal row carpectomy over a midcarpal arthrodesis for patients with a SNAC or SLAC grade II due to a more favourable expected FE ROM. Other results were hard to interpret due to limitations such as small patient numbers and missing data. More comparative research is needed to provide a more definitive conclusion between these surgical procedures.
A radiocarpal arthrodesis is an excellent procedure to reduce pain and improve grip strength in patients with wrist osteoarthritis secondary to a distal radius fracture. Inherent to the procedure, FE ROM is compromised after radiocarpal arthrodesis. In contrast, both FE and RU ROM improve significantly after total wrist arthroplasty. There is insufficient data on grip strength after total wrist arthroplasty. The findings of this review suggest that favorable functional and patient reported outcomes can be expected after a total wrist arthroplasty in comparison to radiocarpal arthrodesis. Although mid-term survival rates of 93-94% in recent series of Reigstad et al. and Holzbauer et al. seem promising [28, 29], long-term outcomes are still unclear. Nevertheless, total wrist arthroplasty could be a safe and reliable option in an older patient population with posttraumatic wrist osteoarthritis.
Several limitations are apparent in this study. First, we found that high quality studies are scarce. Also, the absolute patient numbers that could be included in the systematic review are low, even after pooling all eligible studies. Next, the included studies have a notable heterogeneity in terms of patient characteristics and surgical interventions. For example, the analyzed midcarpal arthrodesis group consisted of different fusions performed with different implants, each having its own theoretical advantages and disadvantages. The heterogeneous patient characteristics make it even more difficult to compare each of the main categorized interventions as it could lead to a potential risk of bias. Lastly, we have to recognize that there is no uniform method to assess patient reported and functional outcomes in current literature and that outcome measures were collected in many ways. This heterogeneity in reporting could also add to a potential risk of bias. More high quality studies and more standardized reporting of patient reported and functional outcomes or the use of national or international registries in wrist surgery would greatly benefit the understanding of the effect of surgeries performed today. This would make it easier to combine the results of smaller (cohort) studies and compare the different surgeries.
Conclusion
In this systematic review, we performed a thorough, high quality critical appraisal of the available literature regarding the surgical treatment of posttraumatic radiocarpal osteoarthritis. We found that high quality studies are scarce, and when selecting these studies, absolute patient numbers are small. Therefore, some restraint is needed evaluating these results. Evidence of this review did not support the indication for denervation in this particular patient population any more. In patients with SLAC/SNAC II, proximal row carpectomy might be favorable to a midcarpal arthrodesis solely based on better FE ROM of the radiocarpal joint after proximal row carpectomy. Other results were hard to interpret due to limitations such as small patient numbers and missing data. More comparative research is needed to provide a more definitive conclusion between these surgical procedures. In terms of radiocarpal mobility, total wrist arthroplasty might be preferred to radioscapholunate arthrodesis in specific patients with osteoarthritis after a distal radius fracture. The displayed results can help clinicians select the best surgical treatment for each patient and manage the patient’s expectations.
Availability of data and materials
All data generated or analysed during this study are included in this published article and its supplementary information files.
Abbreviations
- DASH:
-
Disability of Arm, Shoulder and Hand
- FE:
-
flexion/extension
- MINORS:
-
Methodological Index for Non-Randomized Studies
- PRISMA:
-
Preferred Reporting Items for Systematic review and Meta-Analyses
- ROM:
-
Range of motion
- RU:
-
radial/ulnar deviation
- SLAC:
-
scapholunate advanced collapse
- SNAC:
-
scaphoid nonunion advanced collapse
- VAS:
-
Visual Analogue Scale
References
Cayci C, Carlsen BT. Osteoarthritis of the wrist. Plast Reconstr Surg. 2014;133(3):605–15.
Feydy A, Pluot E, Guerini H, Drapé JL. Osteoarthritis of the wrist and hand, and spine. Radiol Clin North Am. 2009;47(4):723–59.
Talwalkar SC, Hayton MJ, Stanley JK. Wrist osteoarthritis. Scand J Surg. 2008;97(4):305–9.
Andersson JK, Hagert E, Brittberg M. Cartilage Injuries and Posttraumatic Osteoarthritis in the Wrist: A Review. Cartilage. 2021;13(1_suppl):156s–68s.
Watson HK, Ballet FL. The SLAC wrist: Scapholunate advanced collapse pattern of degenerative arthritis. J Hand Surg. 1984;9(3):358–65.
Shah CM, Stern PJ. Scapholunate advanced collapse (SLAC) and scaphoid nonunion advanced collapse (SNAC) wrist arthritis. Curr Rev Musculoskelet Med. 2013;6(1):9–17.
Adams BD. Surgical management of the arthritic wrist. Instr Course Lect. 2004;53:41–5.
Weiss KE, Rodner CM. Osteoarthritis of the Wrist. J Hand Surg. 2007;32(5):725–46.
Laulan J, Marteau E, Bacle G. Wrist osteoarthritis. Orthop Traumatol Surg Res. 2015;101(1 Suppl):S1-9.
Boeckstyns MEH. Functional outcomes after salvage procedures for the destroyed wrist: an overview. J Hand Surg Eur. 2020;45(1):19–27.
Adams JE. Surgical management of osteoarthritis of the hand and wrist. J Hand Ther. 2022;35(3):418–27.
Berber O, Gidwani S, Garagnani L, Spiteri M, Riley N, McNab I, et al. Salvage of the Failed Total Wrist Arthroplasty: A Systematic Review. J Wrist Surg. 2020;9(5):446–56.
Ahmadi AR, Duraku LS, van der Oest MJW, Hundepool CA, Selles RW, Zuidam JM. The never-ending battle between proximal row carpectomy and four corner arthrodesis: A systematic review and meta-analysis for the final verdict. J Plast Reconstr Aesthet Surg. 2022;75(2):711–21.
Berber O, Garagnani L, Gidwani S. Systematic Review of Total Wrist Arthroplasty and Arthrodesis in Wrist Arthritis. J Wrist Surg. 2018;7(5):424–40.
Chammas PE, Hadouiri N, Chammas M, Ramos-Pascual S, Stirling P, Nover L, et al. Proximal row carpectomy generates better mid- to long-term outcomes than four-corner arthrodesis for post-traumatic wrist arthritis: A meta-analysis. Orthop Traumatol Surg Res. 2022;108(7):103373.
Page MJ, Moher D, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. PRISMA 2020 explanation and elaboration: updated guidance and exemplars for reporting systematic reviews. BMJ. 2021;372:n160.
Slim K, Nini E, Forestier D, Kwiatkowski F, Panis Y, Chipponi J. Methodological index for non-randomized studies (minors): development and validation of a new instrument. ANZ J Surg. 2003;73(9):712–6.
Kompoliti E, Prodromou M, Karantanas AH. SLAC and SNAC Wrist: The Top Five Things That General Radiologists Need to Know. Tomography. 2021;7(4):488–503.
Randall DJ, Zhang Y, Li H, Hubbard JC, Kazmers NH. Establishing the Minimal Clinically Important Difference and Substantial Clinical Benefit for the Pain Visual Analog Scale in a Postoperative Hand Surgery Population. J Hand Surg. 2022;47(7):645–53.
Gummesson C, Atroshi I, Ekdahl C. The disabilities of the arm, shoulder and hand (DASH) outcome questionnaire: longitudinal construct validity and measuring self-rated health change after surgery. BMC Musculoskelet Disord. 2003;4:11.
Kim JK, Park MG, Shin SJ. What is the minimum clinically important difference in grip strength? Clin Orthop Relat Res. 2014;472(8):2536–41.
Radu CA, Schachner M, Tränkle M, Germann G, Sauerbier M. Functional results after wrist denervation. Handchir Mikrochir Plast Chir. 2010;42(5):279–86.
Rothe M, Rudolf K, Partecke B. Long-term results following denervation of the wrist in patients with stages II and III SLAC-/SNAC-wrist. Handchirurgie, Mikrochirurgie, Plastische Chirurgie: Organ der Deutschsprachigen Arbeitsgemeinschaft fur Handchirurgie: Organ der Deutschsprachigen Arbeitsgemeinschaft fur Mikrochirurgie der Peripheren Nerven und Gefasse: Organ der. 2006;38(4):261–6.
Schweizer A, von Känel O, Kammer E, Meuli-Simmen C. Long-term follow-up evaluation of denervation of the wrist. The Journal of hand surgery. 2006;31(4):559–64.
Weinstein LP, Berger RA. Analgesic benefit, functional outcome, and patient satisfaction after partial wrist denervation. The Journal of hand surgery. 2002;27(5):833–9.
Pequignot J, Lussiez B, Allieu Y. A adaptive proximal scaphoid implant. Chirurgie de la Main. 2000;19(5):276–85.
Szalay G, Stigler B, Kraus R, Böhringer G, Schnettler R. Proximal row carpectomy and replacement of the proximal pole of the capitate by means of a pyrocarbon cap (RCPI) in advanced carpal collapse. Handchirurgie, Mikrochirurgie, Plastische Chirurgie: Organ der Deutschsprachigen Arbeitsgemeinschaft fur Handchirurgie: Organ der Deutschsprachigen Arbeitsgemeinschaft fur Mikrochirurgie der Peripheren Nerven und Gefasse: Organ der. 2011;44(1):17–22.
Holzbauer M, Mihalic JA, Pollak M, Froschauer SM. Total Wrist Arthroplasty for Posttraumatic Wrist Osteoarthritis: A Cohort Study Comparing Three Indications. Life (Basel). 2022;12(5):617.
Reigstad O, Lutken T, Grimsgaard C, Bolstad B, Thorkildsen R, Rokkum M. Promising one- to six-year results with the Motec wrist arthroplasty in patients with post-traumatic osteoarthritis. J Bone and Joint Surgery - Series B. 2012;94(11):1540–5.
Aita MA, Nakano EK, Schaffhausser HdL, Fukushima WY, Fujiki EN. Randomized clinical trial between proximal row carpectomy and the four-corner fusion for patients with stage II SNAC. Rev Bras de Ortop. 2016;51:574–82.
Cohen MS, Kozin SH. Degenerative arthritis of the wrist: proximal row carpectomy versus scaphoid excision and four-corner arthrodesis. J Hand Surg. 2001;26(1):94–104.
Jebson PJ, Hayes EP, Engber WD. Proximal row carpectomy: a minimum 10-year follow-up study. J Hand Surg. 2003;28(4):561–9.
Nagelvoort RWK, Kon M, Schuurman AH. Proximal row carpectomy: a worthwhile salvage procedure. Scand J Plast Reconstr Surg Hand Surg. 2002;36(5):289–99.
Pogliacomi F, Marenghi L, Corradi M, Pedrazzini A, Ceccarelli F. Proximal row carpectomy in the third millenium: is it still a valid indication? Acta Biomed. 2014;85(3):243–51.
Salomon GD, Eaton RG. Proximal row carpectomy with partial capitate resection. J Hand Surg. 1996;21(1):2–8.
De Smet L, Degreef I, Truyen J, Robijns F. Outcome of two salvage procedures for posttraumatic osteoarthritis of the wrist: Arthrodesis or proximal row carpectomy. Acta Chirurgica Belgica. 2005;105(6):626–30.
Streich NA, Martini AK, Daecke W. Proximal row carpectomy: an adequate procedure in carpal collapse. Int Orthop. 2008;32(1):85–9.
Abdelaziz AM, Aldahshan W, Elsherief FAH, Wahd Y, Soliman HAG, El Behairy HF, et al. Scaphoid excision with lunatocapitate fusion for the treatment of scaphoid nonunion with advanced collapsed wrist. Int Orthop. 2020;44(6):1153–7.
Calandruccio JH, Gelberman RH, Duncan SF, Goldfarb CA, Pae R, Gramig W. Capitolunate arthrodesis with scaphoid and triquetrum excision. J Hand Surg. 2000;25(5):824–32.
Cha S-M, Shin H-D, Kim K-C. Clinical and radiological outcomes of scaphoidectomy and 4-corner fusion in scapholunate advanced collapse at 5 and 10 years. Ann Plast Surg. 2013;71(2):166–9.
Chung KC, Watt AJ, Kotsis SV. A prospective outcomes study of four-corner wrist arthrodesis using a circular limited wrist fusion plate for stage II scapholunate advanced collapse wrist deformity. Plast Reconstr Surg. 2006;118(2):433–42.
Le Corre A, Ardouin L, Loubersac T, Gaisne E, Bellemère P. Retrospective study of two fixation methods for 4-corner fusion: Shape-memory staple vs. dorsal circular plate. Chir Main. 2015;34(6):300–6.
Dimitrios G, Athanasios K, Ageliki K, Spiridon S. Capitolunate arthrodesis maintaining carpal height for the treatment of SNAC wrist. J Hand Surg (European Volume). 2010;35(3):198–201.
Durand A, Harisboure A, Nurbel B, Lawane M, Grenier de Cardenal D, Giraud B, et al. Capitolunate arthrodesis with tension band wire in wrist arthritis: twenty cases with four year follow-up. Revue de Chirurgie Orthopedique et Reparatrice de l'Appareil Moteur. 2007;93(1):37-45.
Ferreres A, Garcia-Elias M, Plaza R. Long-term results of lunocapitate arthrodesis with scaphoid excision for SLAC and SNAC wrists. J Hand Surg Eur. 2009;34(5):603–8.
Ghargozloo D, Tomarchio A, Ballerini M, Saccalani E, Grazioli G, Chitoni G. High results and lower cost in four-bone arthrodesis with retrograde screws. Med Glas (Zenica). 2022;19(1):75–8.
Hernekamp J, Reinecke A, Neubrech F, Bickert B, Kneser U, Kremer T. Four-corner fusion: comparison of patient satisfaction and functional outcome of conventional K-wire technique vs a new locking plate. Arch Orthop Trauma Surg. 2016;136:571–8.
Huang HK, Wu CH, Huang YC, Yin CY, Hung WC, Wang JP. Lateral Approach for Scaphoid Excision and Capitolunate Arthrodesis in the Treatment of Scapholunate Advanced Collapse and Scaphoid Nonunion Advanced Collapse Wrists: A Case Series. Orthopaedic Surgery. 2021;15(1):347–54.
Kendall CB, Brown TR, Millon SJ, Rudisill LE Jr, Sanders JL, Tanner SL. Results of four-corner arthrodesis using dorsal circular plate fixation. The Journal of hand surgery. 2005;30(5):903–7.
Khan SK, Ali SM, McKee A, Jones JW. Outcomes of four-corner arthrodesis using the Hubcap circular plate. Hand Surg. 2013;18(2):215–20.
Maire N, Facca S, Gouzou S, Liverneaux P. Midcarpal fusion using break-away compression screw. Chirurgie de la Main. 2011;31(1):24–9.
Mantovani G, Mathoulin C, Fukushima W, Cho A, Aita M, Argintar E. Four corner arthrodesis limited to the centre using a scaphoid one piece graft and a dorsal circular plate. Journal of Hand Surgery (European Volume). 2010;35(1):38–42.
Schindelar LE, Wang ML, Bednar JM, Miller AJ. Lunatocapitate and triquetrohamate arthrodeses for degenerative arthritis of the wrist: a midterm follow-up. Hand (New York, NY). 2022;18(2):15589447211066351.
De Smet L, Degreef I, Robijns F, Truyen J, Deprez P. Salvage procedures for degenerative osteoarthritis of the wrist due to advanced carpal collapse. Acta orthopaedica belgica. 2006;72(5):535.
De Smet L, Deprez P, Duerinckx J, Degreef I. Outcome of four-corner arthrodesis for advanced carpal collapse: circular plate versus traditional techniques. Acta Orthopædica Belgica. 2009;75(3):323.
Tielemans A, Van Innis F, Troussel S, Detrembleur C, Libouton X, Lequint T. Effect of four-corner fusion with locking plate without bone graft on functional recovery of the wrist: New treatment guidelines. Hand Surg Rehabil. 2017;36(3):186–91.
Undurraga S, Au K, Dobransky J, Gammon B. Scaphoid Excision and Bicolumnar Carpal Fusion with Retrograde Headless Screws. J Wrist Surg. 2021;10(3):201–7.
Winkler F, Borisch N, Rath B, Grifka J, Heers G. Mittelfristige Ergebnisse nach Skaphoidresektion und mediokarpaler Teilarthrodese unter Verwendung von K-Drähten bei fortgeschrittenem karpalen Kollaps. Zeitschrift für Orthopädie und Unfallchirurgie. 2010;148(03):332–7.
Yao YC, Wang JP, Huang TF, Chang MC, Huang YC. Lunocapitate fusion with scaphoid excision for the treatment of scaphoid nonunion advanced collapse or scapho-lunate advanced collapse wrist. J Chin Med Assoc. 2017;80(2):117–20.
Bach AW, Almquist EE, Newman DM. Proximal row fusion as a solution for radiocarpal arthritis. J Hand Surg Am. 1991;16(3):424–31.
Beyermann K, Prommersberger KJ, Lanz U. Radioscapholunate fusion following comminuted fractures of the distal radius. European Journal of Trauma. 2000;26(4):169–75.
Degeorge B, Dagneaux L, Montoya-Faivre D, Dautel G, Dap F, Coulet B, et al. Radioscapholunate fusion for posttraumatic osteoarthritis with consecutive excision of the distal scaphoid and the triquetrum: A comparative study. Hand Surg Rehabil. 2020;39(5):375–82.
Garcia-Elias M, Lluch AL, Ferreres A. Partial Arthrodesis for the Treatment of Radiocarpal Osteoarthritis. Journal of the American Society for Surgery of the Hand. 2005;5(2):100–8.
Inoue G, Tamura Y. Radiolunate and radioscapholunate arthrodesis. Archives of Orthopaedic and Trauma Surgery. 1992;111(6):333–5.
Kilgus M, Weishaupt D, Künzi W, Meyer VE. Radioscapholunate fusion: long-term results. Handchir Mikrochir Plast Chir. 2003;35(5):317–22.
Quadlbauer S, Leixnering M, Jurkowitsch J, Hausner T, Pezzei C. Volar Radioscapholunate Arthrodesis and Distal Scaphoidectomy After Malunited Distal Radius Fractures. J Hand Surg Am. 2017;42(9):754.e1-.e8.
Tomaino MM, Miller RJ, Cole I, Burton RI. Scapholunate advanced collapse wrist: proximal row carpectomy or limited wrist arthrodesis with scaphoid excision? J Hand Surg Am. 1994;19(1):134–42.
Yajima H, Tamai S, Ono H. Partial radiocarpal arthrodesis. J Jpn Orthop Assoc. 1994;68(10):847–53.
Yajima H, Kobata Y, Shigematsu K, Kawamura K, Takakura Y. Radiocarpal arthrodesis for osteoarthritis following fractures of the distal radius. Hand Surg. 2004;09(02):203–9. https://doi.org/10.1142/S0218810404002297.
Singh HP, Dias JJ, Phadnis J, Bain G. Comparison of the clinical and functional outcomes following 3- and 4-corner fusions. J Hand Surg Am. 2015;40(6):1117–23.
Smeraglia F, Basso MA, Famiglietti G, Eckersley R, Bernasconi A, Balato G. Partial wrist denervation versus total wrist denervation: A systematic review of the literature. Hand Surg Rehabil. 2020;39(6):487–91.
Schmidt I. Functional Outcomes After Salvage Procedures for Wrist Trauma and Arthritis (Four-Corner Fusion, Proximal Row Carpectomy, Total Wrist Arthroplasty, Total Wrist Fusion, Wrist Denervation): A Review of Literature. The Open Orthopaedics Journal. 2019;13(1):217–31.
Swärd EM, Franko MA, Wilcke MK. The effects of partial wrist denervation in wrist osteoarthritis: patient-reported outcomes and objective function. J Hand Surg Eur. 2022;47(8):798–804.
Reyniers P, van Beek N, De Schrijver F, Goeminne S. Proximal row carpectomy versus four-corner arthrodesis in the treatment of SLAC and SNAC wrist: meta-analysis and literature review. Hand Surg Rehabil. 2023;42(3):194–202.
Amer KM, Thomson JE, Vosbikian MM, Ahmed I. Four-Corner Arthrodesis Versus Proximal Row Carpectomy for Scapholunate Advanced Collapse: A Systematic Literature Review and Meta-analysis. Ann Plast Surg. 2020;85(6):699–703.
Mulford JS, Ceulemans LJ, Nam D, Axelrod TS. Proximal row carpectomy vs four corner fusion for scapholunate (Slac) or scaphoid nonunion advanced collapse (Snac) wrists: a systematic review of outcomes. J Hand Surg Eur. 2009;34(2):256–63.
De Vitis R, Passiatore M, Cilli V, Pamelin E, Velluto C, Ceravolo I, et al. Secondary Wrist Arthritis in Active Workers: Does Capitate Pyrocarbon Resurfacing (RCPI) Improve Proximal Row Carpectomy? A Retrospective Cohort Study. J Hand Surg Asian Pac. 2021;26(4):625–34.
Gvozdenovic R, Schioedt MA, Solgaard L, Vadstrup LS, Soee NH. Limited intercarpal fusion versus proximal row carpectomy in the treatment of SLAC or SNAC wrist results after 3.5 years. J Orthop Surg Res. 2023;18(1):681.
Richou J, Chuinard C, Moineau G, Hanouz N, Hu W, Le Nen D. Proximal row carpectomy: long-term results. Chir Main. 2010;29(1):10–5.
Ali MH, Rizzo M, Shin AY, Moran SL. Long-term outcomes of proximal row carpectomy: a minimum of 15-year follow-up. Hand (N Y). 2012;7(1):72–8.
Acknowledgements
Not applicable.
Funding
The authors received no financial support for the research, authorship, and/or publication of this article.
Author information
Authors and Affiliations
Contributions
J.A.E. Gruisen, P.M.J. Schormans and I.M. Punt conducted the literature review and took lead in writing the manuscript under the supervision of P.F.W. Hannemann. I.M. Punt set up the literature database. S.M.J. van Kuijk advised on and checked the used statistical method and interpretation of the results. All authors discussed the results and contributed to the final manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was reported according to Preferred Reporting Items for Systematic review and Meta-Analyses (PRISMA). The study protocol has been registered in the PROSPERO database (CRD42017080427). No ethical approval was needed for this systematic review.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Gruisen, J.A.E., Schormans, P.M.J., Punt, I.M. et al. Patient reported and functional outcome measures after surgical salvage procedures for posttraumatic radiocarpal osteoarthritis – a systematic review. BMC Musculoskelet Disord 25, 453 (2024). https://doi.org/10.1186/s12891-024-07527-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12891-024-07527-6