Abstract
Large vessel vasculitis (LVV) is the most common form of primary vasculitis comprising of giant cell arteritis (GCA), Takayasu’s arteritis (TAK) and idiopathic aortitis. Early diagnosis and treatment of LVV are paramount to reduce the risk of ischemic complications such as visual loss and strokes, vascular stenosis and occlusion, and aortic aneurysm formation. Use of imaging modalities [ultrasound (US), magnetic resonance imaging (MRI), computed tomography (CT) and [18F]-fluorodeoxyglucose positron emission tomography (PET)] has steadily increased to enable assessment of cranial and extracranial arteries, as well as the aorta. These imaging modalities are less invasive, more sensitive and readily available compared to temporal artery biopsy (TAB). Modern imaging methods have changed the role of TAB in diagnosing GCA and have replaced diagnostic angiography. Over the last two decades, several studies have evaluated the use of US, MRI, CT and PET in LVV. However, these various imaging tools are not yet uniformly used in routine clinical practice and controversy exists as to which imaging modality best provides meaningful assessments of disease activity and damage in LVV. In January 2018, evidence-based recommendations for the use of imaging modalities in LVV were published. The aim of this review is to summarize the current evidence of imaging in patients with or suspected of having LVV, and to highlight the clinical implications of the EULAR recommendations.


Similar content being viewed by others
References
Smeeth L, Cook C, Hall AJ (2006) Incidence of diagnosed Polymyalgia rheumatica and temporal arteritis in the United Kingdom, 1990–2001. Ann Rheum Dis 65:1093–1098
Lawrence RC, Felson DT, Helmick CG et al (2008) Estimates of the prevalence of arthritis and other rheumatic conditions in the United States. Part II. Arthritis Rheum 58:26–35
Salvarani C, Pipitone N, Versari A et al (2012) Clinical features of Polymyalgia rheumatica and giant cell arteritis. Nat Rev Rheumatol 8:509–521
Direskeneli H (2017) Clinical assessment in Takayasu’s arteritis: major challenges and controversies. Clin Exp Rheumatol 35(Suppl. 103):189–193
Boes C (2007) Bayard Horton’s clinicopathological description of giant cell (temporal) arteritis. Cephalalgia 27(1):68–75
Hall S, Persellin S, Lie JT et al (1983) The therapeutic impact of temporal artery biopsy. Lancet 2:1217–1220
Mukhtyar C, Guillevin L, Cid MC et al (2009) EULAR recommendations for the management of large vessel vasculitis. Ann Rheum Dis 68:318–323
Hunder GG, Bloch DA, Michel BA et al (1990) The American College of Rheumatology 1990 criteria for the classification of giant cell arteritis. Arthritis Rheum 33:1122–1128
Luqmani R, Lee E, Singh S et al (2016) The role of ultrasound compared to biopsy of Temporal Arteries in the Diagnosis and Treatment of Giant Cell Arteritis (TABUL): a diagnostic accuracy and cost-effectiveness study. Health Technol Assess 20:1–238
Prieto-González S, Arguis P, Cid MC (2015) Imaging in systemic vasculitis. Curr Opin Rheumatol 27:53–62
Monti S, Floris A, Ponte C et al (2018) The use of ultrasound to assess giant cell arteritis: review of the current evidence and practical guide for the rheumatologist. Rheumatology (Oxford) 57(2):227–235
Brack A, Martinez-Taboada V, Stanson A et al (1999) Disease pattern in cranial and large-vessel giant cell arteritis. Arthritis Rheum 42:311–317
Schmidt WA, Seifert A, Gromnica-Ihle E et al (2008) Ultrasound of proximal upper extremity arteries to increase the diagnostic yield in large-vessel giant cell arteritis. Rheumatology 47:96–101
Patil P, Williams M, Maw WW et al (2015) Fast track pathway reduces sight loss in giant cell arteritis: results of a longitudinal observational cohort study. Clin Exp Rheumatol 33(2 Suppl. 89): S-103-6. Epub 2015 May 26
Diamantopoulos AP, Haugeberg G, Lindland A et al (2016) The fast-track ultrasound clinic for early diagnosis of giant cell arteritis significantly reduces permanent visual impairment: towards a more effective strategy to improve clinical outcome in giant cell arteritis? Rheumatology 55:66–70
Dejaco C, Duftner C, Buttgereit F et al (2017) The spectrum of giant cell arteritis and Polymyalgia rheumatica: revisiting the concept of the disease. Rheumatology 56:506–515
Arend WP, Michel BA, Bloch DA et al (1990) The American College of Rheumatology 1990 criteria for the classification of Takayasu arteritis. Arthritis Rheum 33:1129–1134
Schmidt WA (2014) Role of ultrasound in the understanding and management of vasculitis. Ther Adv Musculoskelet Dis 6:39–47
Cinar I, Wang H, Stone JR (2017) Clinically isolated aortitis: pitfalls, progress, and possibilities. Cardiovasc Pathol 29:23–32
Dejaco C, Ramiro S, Duftner C et al (2018) Ann Rheum Dis 77:636–643
Duftner C, Dejaco C, Sepriano A et al (2018) Imaging in diagnosis, outcome prediction and monitoring of large vessel vasculitis: a systematic literature review and metaanalysis informing the EULAR recommendations. RMD Open 4:e000612. https://doi.org/10.1136/rmdopen-2017-000612
Salvarani C, Cimino L, Macchioni P et al (2005) Risk factors for visual loss in an Italian population-based cohort of patients with giant cell arteritis. Arthritis Rheum 53:293–297
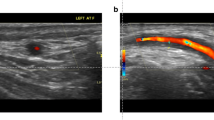
Schmidt WA, Kraft HE, Vorpahl K et al (1997) Color duplex ultrasonography in the diagnosis of temporal arteritis. N Engl J Med 337:1336–1342
Karahaliou M, Vaiopoulos G, Papaspyrou S et al (2006) Colour duplex sonography of temporal arteries before decision for biopsy: a prospective study in 55 patients with suspected giant cell arteritis. Arthritis Res Ther 8:R116
Hauenstein C, Reinhard M, Geiger J et al (2012) Effects of early corticosteroid treatment on magnetic resonance imaging and ultrasonography findings in giant cell arteritis. Rheumatology 51:1999–2003
De Miguel E, Castillo C, Rodríguez A et al (2009) Learning and reliability of colour Doppler ultrasound in giant cell arteritis. Clin Exp Rheumatol 27(S53):8
Chrysidis S, Duftner C, Dejaco C et al (2018) Definitions and reliability assessment of elementary ultrasound lesions in giant cell arteritis: a study from the OMERACT Large Vessel Vasculitis Ultrasound Working Group. Rheumatology 57(2):227–235
Aschwanden M, Kesten F, Stern M et al (2010) Vascular involvement in patients with giant cell arteritis determined by duplex sonography of 2 × 11 arterial regions. Ann Rheum Dis 69:1356–1359
De Miguel E, Roxo A, Castillo C et al (2012) The utility and sensitivity of colour Doppler ultrasound in monitoring changes in giant cell arteritis. Clin Exp Rheumatol 30:S34–S38
Habib HM, Essa AA, Hassan AA (2012) Color duplex ultrasonography of temporal arteries: role in diagnosis and follow-up of suspected cases of temporal arteritis. Clin Rheumatol 31:231–237
Pérez López J, Solans Laqué R, Bosch Gil JA et al (2009) Colour-duplex ultrasonography of the temporal and ophthalmic arteries in the diagnosis and follow-up of giant cell arteritis. Clin Exp Rheumatol 27:S77–S82
Pfadenhauer K, Weber H (2003) Duplex sonography of the temporal and occipital artery in the diagnosis of temporal arteritis. A prospective study. J Rheumatol 30:2177–2181
Salvarani C, Silingardi M, Ghirarduzzi A et al (2002) Is duplex ultrasonography useful for the diagnosis of giant-cell arteritis? Ann Intern Med 137:232–238
Schmidt WA, Moll A, Seifert A et al (2008) Prognosis of large-vessel giant cell arteritis. Rheumatology 47:1406–1408
Schmidt WA, Natusch A, Möller DE et al (2002) Involvement of peripheral arteries in giant cell arteritis: a color Doppler sonography study. Clin Exp Rheumatol 20:309–318
Reinhard M, Schmidt D, Hetzel A (2004) Color-coded sonography in suspected temporal arteritis-experiences after 83 cases. Rheumatol Int 24:340–346
Romera-Villegas A, Vila-Coll R, Poca-Dias V et al (2004) The role of color duplex sonography in the diagnosis of giant cell arteritis. J Ultrasound Med 23:1493–1498
Aschwanden M, Daikeler T, Kesten F et al (2015) Temporal artery compression sign—a novel ultrasound finding for the diagnosis of giant cell arteritis. Clin Exp Rheumatol 33(2 Suppl. 89):S-113-5. Epub 2015 May 26
Aschwanden M, Imfeld S, Staub D et al (2015) The ultrasound compression sign to diagnose temporal giant cell arteritis shows an excellent interobserver agreement. Clin Exp Rheumatol 33:S-113
Karassa FB, Matsagas MI, Schmidt WA et al (2005) Meta-analysis: test performance of ultrasonography for giant-cell arteritis. Ann Intern Med 142:359–369
Ball EL, Walsh SR, Tang TY et al (2010) Role of ultrasonography in the diagnosis of temporal arteritis. Br J Surg 97:1765–1771
Arida A, Kyprianou M, Kanakis M et al (2010) The diagnostic value of ultrasonography-derived edema of the temporal artery wall in giant cell arteritis: a second meta-analysis. BMC Musculoskelet Disord 11:44
Nesher G, Shemesh D, Mates M et al (2002) The predictive value of the halo sign in color Doppler ultrasonography of the temporal arteries for diagnosing giant cell arteritis. J Rheumatol 29:1224–1226
Pfadenhauer K, Weber H (2006) Ultrasonography of the temporal, periorbital and carotid arteries in the diagnosis of giant cell arteritis and its neuroophthalmological complications. Ultraschall Med 27:329–335
Diamantopoulos AP, Haugeberg G, Hetland H et al (2014) Diagnostic value of color Doppler ultrasonography of temporal arteries and large vessels in giant cell arteritis: a consecutive case series. Arthritis Care Res 66:113–119
Gunawardene AR, Chant H (2014) Facial nerve injury during temporal artery biopsy. Ann R Coll Surg Engl 96:257–260
Bley TA, Reinhard M, Hauenstein C et al (2008) Comparison of duplex sonography and high-resolution magnetic resonance imaging in the diagnosis of giant cell (temporal) arteritis. Arthritis Rheum 58:2574–2578
Lariviere D, Benali K, Coustet B et al (2016) Positron emission tomography and computed tomography angiography for the diagnosis of giant cell arteritis: a real-life prospective study. Medicine 95:e4146
Nielsen BD, Hansen IT, Kramer S et al (2018) Simple dichotomous assessment of cranial artery inflammation by conventional 18F-FDG PET/CT shows high accuracy for the diagnosis of giant cell arteritis: a case–control study. Eur J Nucl Med Mol Imaging. https://doi.org/10.1007/s00259-018-4106-0
Muratore F, Kermani TA, Crowson CS et al (2015) Large-vessel giant cell arteritis: a cohort study. Rheumatology 54:463–470
Blockmans D, Stroobants S, Maes A et al (2000) Positron emission tomography in giant cell arteritis and Polymyalgia rheumatica: evidence for inflammation of the aortic arch. Am J Med 108:246–249
Blockmans D, Coudyzer W, Vanderschueren S et al (2008) Relationship between fluorodeoxyglucose uptake in the large vessels and late aortic diameter in giant cell arteritis. Rheumatology 47:1179–1184
Nielsen BD, Gormsen LC, Hansen IT et al (2018) Three days of high-dose glucocorticoid treatment attenuates large-vessel 18F-FDG uptake in large-vessel giant cell arteritis but with a limited impact on diagnostic accuracy. Eur J Nucl Med Mol Imaging 45:1119. https://doi.org/10.1007/s00259-018-4021-4
Puppo C, Massollo M, Paparo F et al (2014) Giant cell arteritis: a systematic review of the qualitative and semiquantitative methods to assess vasculitis with 18F-fluorodeoxyglucose positron emission tomography. Biomed Res Int 2014:1–11
Fan W, Zhu J, Li J et al (2016) Ultrasound morphological changes in the carotid wall of Takayasu’s arteritis: monitor of disease progression. Int Angiol 35:586–592
Yamada I, Nakagawa T, Himeno Y et al (2000) Takayasu arteritis: diagnosis with breath-hold contrast-enhanced three-dimensional MR angiography. J Magn Reson Imaging 11:481–487
Sun Y, Ma L, Ji Z et al (2016) Value of whole-body contrast-enhanced magnetic resonance angiography with vessel wall imaging in quantitative assessment of disease activity and follow-up examination in Takayasu’s arteritis. Clin Rheumatol 35:685–693
Yamada I, Nakagawa T, Himeno Y et al (1998) Takayasu arteritis: evaluation of the thoracic aorta with CT angiography. Radiology 209:103–109
García-Martínez A, Arguis P, Prieto-González S et al (2014) Prospective long term follow-up of a cohort of patients with giant cell arteritis screened for aortic structural damage (aneurysm or dilatation). Ann Rheum Dis 73:1826–1832
Robson JC, Kiran A, Maskell J et al (2015) The relative risk of aortic aneurysm in patients with giant cell arteritis compared with the general population of the UK. Ann Rheum Dis 74:129–135
Gülcü A, Gezer NS, Akar S et al (2017) Long-term follow-up of endovascular repair in the management of arterial stenosis caused by Takayasu’s arteritis. Ann Vasc Surg 42:93–100
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical standards
This article does not contain any studies with human participants performed by any of the authors.
Informed consent
Given the nature of this review paper, there was no informed consent required from any participants.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Bardi, M., Diamantopoulos, A.P. EULAR recommendations for the use of imaging in large vessel vasculitis in clinical practice summary. Radiol med 124, 965–972 (2019). https://doi.org/10.1007/s11547-019-01058-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11547-019-01058-0