Abstract
Purpose of the review
The two main forms of large-vessel vasculitis (LVV) are giant cell arteritis (GCA) and Takayasu’s arteritis (TAK). Vascular imaging can characterize disease activity and disease extent in LVV. This review critically analyzes the clinical utility of vascular imaging in LVV and highlights how imaging may be incorporated into the management and study of these conditions.
Recent findings
There are multiple imaging modalities available to assess LVV including ultrasonography, CT angiography (CTA), magnetic resonance angiography (MRA), and 18F-fluorodeoxyglucose (FDG) positron emission tomography (PET). As these techniques are refined, imaging may be increasingly useful to evaluate the cranial arteries and the aorta and its primary branches. In addition, vascular imaging may be useful to monitor disease activity and may have prognostic value to predict future clinical events.
Summary
There are strengths and weaknesses associated with vascular imaging that should be considered when evaluating patients with LVV. Vascular imaging will likely play an increasingly important role in the clinical management of patients and the conduct of research in LVV and may ultimately be incorporated as outcome measures in clinical trials in these conditions.



Similar content being viewed by others
References and Recommended Reading
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Jennette JC, Falk RJ, Bacon PA, Basu N, Cid MC, Ferrario F, et al. 2012 revised International Chapel Hill Consensus Conference Nomenclature of Vasculitides. Arthritis Rheum. 2013;65(1):1–11. https://doi.org/10.1002/art.37715.
Hunder GG, Arend WP, Bloch DA, Calabrese LH, Fauci AS, Fries JF, et al. The American College of Rheumatology 1990 criteria for the classification of vasculitis. Arthritis Rheum. 1990;33(8):1065–7.
Hunder GG, Bloch DA, Michel BA, Stevens MB, Arend WP, Calabrese LH, et al. The American College of Rheumatology 1990 criteria for the classification of giant cell arteritis. Arthritis Rheum. 1990;33(8):1122–8.
Arend WP, Michel BA, Bloch DA, Hunder GG, Calabrese LH, Edworthy SM, et al. The American College of Rheumatology 1990 criteria for the classification of Takayasu arteritis. Arthritis Rheum. 1990;33(8):1129–34.
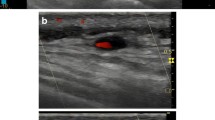
Chrysidis S, Duftner C, Dejaco C, Schafer VS, Ramiro S, Carrara G, et al. Definitions and reliability assessment of elementary ultrasound lesions in giant cell arteritis: a study from the OMERACT Large Vessel Vasculitis Ultrasound Working Group. RMD Open. 2018;4(1):e000598. https://doi.org/10.1136/rmdopen-2017-000598.
Aschwanden M, Imfeld S, Staub D, Baldi T, Walker UA, Berger CT et al. The ultrasound compression sign to diagnose temporal giant cell arteritis shows an excellent interobserver agreement. Clin Exp Rheumatol. 2015;33(2 Suppl 89):S-113-5.
Monti S, Floris A, Ponte C, Schmidt WA, Diamantopoulos AP, Pereira C, et al. The use of ultrasound to assess giant cell arteritis: review of the current evidence and practical guide for the rheumatologist. Rheumatology (Oxford). 2018;57(2):227–35. https://doi.org/10.1093/rheumatology/kex173.
Schmidt WA, Kraft HE, Vorpahl K, Volker L, Gromnica-Ihle EJ. Color duplex ultrasonography in the diagnosis of temporal arteritis. N Engl J Med. 1997;337(19):1336–42. https://doi.org/10.1056/NEJM199711063371902.
Arida A, Kyprianou M, Kanakis M, Sfikakis PP. The diagnostic value of ultrasonography-derived edema of the temporal artery wall in giant cell arteritis: a second meta-analysis. BMC Musculoskelet Disord. 2010;11:44. https://doi.org/10.1186/1471-2474-11-44.
Maldini C, Depinay-Dhellemmes C, Tra TT, Chauveau M, Allanore Y, Gossec L, et al. Limited value of temporal artery ultrasonography examinations for diagnosis of giant cell arteritis: analysis of 77 subjects. J Rheumatol. 2010;37(11):2326–30. https://doi.org/10.3899/jrheum.100353.
Luqmani R, Lee E, Singh S, Gillett M, Schmidt WA, Bradburn M, et al. The role of ultrasound compared to biopsy of temporal arteries in the diagnosis and treatment of giant cell arteritis (TABUL): a diagnostic accuracy and cost-effectiveness study. Health Technol Assess. 2016;20(90):1–238. https://doi.org/10.3310/hta20900. This study compared ultrasound to temporal artery biopsy in giant cell arteritis in a large cohort of patients.
Salvarani C, Silingardi M, Ghirarduzzi A, Lo Scocco G, Macchioni P, Bajocchi G, et al. Is duplex ultrasonography useful for the diagnosis of giant-cell arteritis? Ann Intern Med. 2002;137(4):232–8.
Karassa FB, Matsagas MI, Schmidt WA, Ioannidis JP. Meta-analysis: test performance of ultrasonography for giant-cell arteritis. Ann Intern Med. 2005;142(5):359–69.
Ball EL, Walsh SR, Tang TY, Gohil R, Clarke JM. Role of ultrasonography in the diagnosis of temporal arteritis. Br J Surg. 2010;97(12):1765–71. https://doi.org/10.1002/bjs.7252.
Schmidt WA, Gromnica-Ihle E. Incidence of temporal arteritis in patients with polymyalgia rheumatica: a prospective study using colour Doppler ultrasonography of the temporal arteries. Rheumatology (Oxford). 2002;41(1):46–52.
Diamantopoulos AP, Haugeberg G, Lindland A, Myklebust G. The fast-track ultrasound clinic for early diagnosis of giant cell arteritis significantly reduces permanent visual impairment: towards a more effective strategy to improve clinical outcome in giant cell arteritis? Rheumatology (Oxford). 2016;55(1):66–70. https://doi.org/10.1093/rheumatology/kev289.
Patil P, Williams M, Maw WW, Achilleos K, Elsideeg S, Dejaco C et al. Fast track pathway reduces sight loss in giant cell arteritis: results of a longitudinal observational cohort study. Clin Exp Rheumatol. 2015;33(2 Suppl 89):S-103-6.
Rheaume M, Rebello R, Pagnoux C, Carette S, Clements-Baker M, Cohen-Hallaleh V, et al. High-resolution magnetic resonance imaging of scalp arteries for the diagnosis of giant cell arteritis: results of a prospective cohort study. Arthritis Rheumatol. 2017;69(1):161–8. https://doi.org/10.1002/art.39824. This is a large study evaluating use of high-resolution MRI to evaluate cranial arteries in patients with suspected giant cell arteritis.
Bley TA, Uhl M, Carew J, Markl M, Schmidt D, Peter HH, et al. Diagnostic value of high-resolution MR imaging in giant cell arteritis. AJNR Am J Neuroradiol. 2007;28(9):1722–7. https://doi.org/10.3174/ajnr.A0638.
Geiger J, Bley T, Uhl M, Frydrychowicz A, Langer M, Markl M. Diagnostic value of T2-weighted imaging for the detection of superficial cranial artery inflammation in giant cell arteritis. J Magn Reson Imaging. 2010;31(2):470–4. https://doi.org/10.1002/jmri.22047.
Klink T, Geiger J, Both M, Ness T, Heinzelmann S, Reinhard M, et al. Giant cell arteritis: diagnostic accuracy of MR imaging of superficial cranial arteries in initial diagnosis-results from a multicenter trial. Radiology. 2014;273(3):844–52. https://doi.org/10.1148/radiol.14140056.
Craven A, Robson J, Ponte C, Grayson PC, Suppiah R, Judge A, et al. ACR/EULAR-endorsed study to develop Diagnostic and Classification Criteria for Vasculitis (DCVAS). Clin Exp Nephrol. 2013;17(5):619–21. https://doi.org/10.1007/s10157-013-0854-0.
Dejaco C, Ramiro S, Duftner C, Besson FL, Bley TA, Blockmans D, et al. EULAR recommendations for the use of imaging in large vessel vasculitis in clinical practice. Ann Rheum Dis. 2018;77(5):636–43. https://doi.org/10.1136/annrheumdis-2017-212649. This paper discusses guidelines proposed by EULAR for use of early imaging tests in patients with suspected giant cell arteritis or Takayasu’s arteritis.
Conway R, Smyth AE, Kavanagh RG, O'Donohoe RL, Purcell Y, Heffernan EJ, et al. Diagnostic utility of computed tomographic angiography in giant-cell arteritis. Stroke. 2018;49(9):2233–6. https://doi.org/10.1161/STROKEAHA.118.021995.
Sammel A HE, Schembri G, Nguyen K, Brewer J, Schrieber L, Janssen B, Youssef P, Fraser C, Bailey E, Bailey D, Roach P, Laurent R. The diagnostic accuracy of PET/CT scan of the head, neck and thorax compared with temporal artery biopsy in patients newly suspected of having GCA [abstract]. Arthritis Rheumatol. 2018; 70 (suppl 10).
Nielsen BD THI, Keller KK, Therkildsen P, Hauge EM, Gormsen LC. FDG PET/CT Visualization of inflammation in temporal and maxillary arteries in treatment-naive GCA patients [abstract]. Arthritis Rheumatol. 2017; 69 (suppl 10).
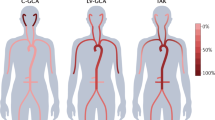
Grayson PC, Maksimowicz-McKinnon K, Clark TM, Tomasson G, Cuthbertson D, Carette S, et al. Distribution of arterial lesions in Takayasu’s arteritis and giant cell arteritis. Ann Rheum Dis. 2012;71(8):1329–34. https://doi.org/10.1136/annrheumdis-2011-200795.
Soriano A, Pazzola G, Boiardi L, Casali M, Muratore F, Pipitone N, et al. Distribution patterns of 18F-fluorodeoxyglucose in large vessels of Takayasu’s and giant cell arteritis using positron emission tomography. Clin Exp Rheumatol. 2018;36(Suppl 111(2)):99–106.
Grayson PC. Lumpers and splitters: ongoing issues in the classification of large vessel vasculitis. J Rheumatol. 2015;42(2):149–51. https://doi.org/10.3899/jrheum.141376.
Grayson PC, Tomasson G, Cuthbertson D, Carette S, Hoffman GS, Khalidi NA, et al. Association of vascular physical examination findings and arteriographic lesions in large vessel vasculitis. J Rheumatol. 2012;39(2):303–9. https://doi.org/10.3899/jrheum.110652.
Furuta S, Cousins C, Chaudhry A, Jayne D. Clinical features and radiological findings in large vessel vasculitis: are Takayasu arteritis and giant cell arteritis 2 different diseases or a single entity? J Rheumatol. 2015;42(2):300–8. https://doi.org/10.3899/jrheum.140562.
Slart R, Writing g, Reviewer g, Members of EC, Members of EI, Inflammation, et al. FDG-PET/CT(A) imaging in large vessel vasculitis and polymyalgia rheumatica: joint procedural recommendation of the EANM, SNMMI, and the PET Interest Group (PIG), and endorsed by the ASNC. Eur J Nucl Med Mol Imaging. 2018;45(7):1250–69. https://doi.org/10.1007/s00259-018-3973-8. This paper outlines recommendations for use of FDG-PET in large-vessel vasculitis.
Lariviere D, Benali K, Coustet B, Pasi N, Hyafil F, Klein I, et al. Positron emission tomography and computed tomography angiography for the diagnosis of giant cell arteritis: a real-life prospective study. Medicine (Baltimore). 2016;95(30):e4146. https://doi.org/10.1097/MD.0000000000004146.
Yamada I, Nakagawa T, Himeno Y, Numano F, Shibuya H. Takayasu arteritis: evaluation of the thoracic aorta with CT angiography. Radiology. 1998;209(1):103–9. https://doi.org/10.1148/radiology.209.1.9769819.
Sparks AR, Johnson PL, Meyer MC. Imaging of abdominal aortic aneurysms. Am Fam Physician. 2002;65(8):1565–70.
Yamada I, Nakagawa T, Himeno Y, Kobayashi Y, Numano F, Shibuya H. Takayasu arteritis: diagnosis with breath-hold contrast-enhanced three-dimensional MR angiography. J Magn Reson Imaging. 2000;11(5):481–7.
Meller J, Grabbe E, Becker W, Vosshenrich R. Value of F-18 FDG hybrid camera PET and MRI in early takayasu aortitis. Eur Radiol. 2003;13(2):400–5. https://doi.org/10.1007/s00330-002-1518-8.
Tedeschi E, Caranci F, Giordano F, Angelini V, Cocozza S, Brunetti A. Gadolinium retention in the body: what we know and what we can do. Radiol Med. 2017;122(8):589–600. https://doi.org/10.1007/s11547-017-0757-3.
Ramalho M, Ramalho J, Burke LM, Semelka RC. Gadolinium retention and toxicity-an update. Adv Chronic Kidney Dis. 2017;24(3):138–46. https://doi.org/10.1053/j.ackd.2017.03.004.
Besson FL, de Boysson H, Parienti JJ, Bouvard G, Bienvenu B, Agostini D. Towards an optimal semiquantitative approach in giant cell arteritis: an (18)F-FDG PET/CT case-control study. Eur J Nucl Med Mol Imaging. 2014;41(1):155–66. https://doi.org/10.1007/s00259-013-2545-1.
Prieto-Gonzalez S, Depetris M, Garcia-Martinez A, Espigol-Frigole G, Tavera-Bahillo I, Corbera-Bellata M, et al. Positron emission tomography assessment of large vessel inflammation in patients with newly diagnosed, biopsy-proven giant cell arteritis: a prospective, case-control study. Ann Rheum Dis. 2014;73(7):1388–92. https://doi.org/10.1136/annrheumdis-2013-204572.
Lehmann P, Buchtala S, Achajew N, Haerle P, Ehrenstein B, Lighvani H, et al. 18F-FDG PET as a diagnostic procedure in large vessel vasculitis-a controlled, blinded re-examination of routine PET scans. Clin Rheumatol. 2011;30(1):37–42. https://doi.org/10.1007/s10067-010-1598-9.
Fuchs M, Briel M, Daikeler T, Walker UA, Rasch H, Berg S, et al. The impact of 18F-FDG PET on the management of patients with suspected large vessel vasculitis. Eur J Nucl Med Mol Imaging. 2012;39(2):344–53. https://doi.org/10.1007/s00259-011-1967-x.
Hautzel H, Sander O, Heinzel A, Schneider M, Muller HW. Assessment of large-vessel involvement in giant cell arteritis with 18F-FDG PET: introducing an ROC-analysis-based cutoff ratio. J Nucl Med. 2008;49(7):1107–13. https://doi.org/10.2967/jnumed.108.051920.
Walter MA, Melzer RA, Schindler C, Muller-Brand J, Tyndall A, Nitzsche EU. The value of [18F]FDG-PET in the diagnosis of large-vessel vasculitis and the assessment of activity and extent of disease. Eur J Nucl Med Mol Imaging. 2005;32(6):674–81. https://doi.org/10.1007/s00259-004-1757-9.
Meller J, Strutz F, Siefker U, Scheel A, Sahlmann CO, Lehmann K, et al. Early diagnosis and follow-up of aortitis with [(18)F]FDG PET and MRI. Eur J Nucl Med Mol Imaging. 2003;30(5):730–6. https://doi.org/10.1007/s00259-003-1144-y.
Henes JC, Muller M, Krieger J, Balletshofer B, Pfannenberg AC, Kanz L, et al. [18F] FDG-PET/CT as a new and sensitive imaging method for the diagnosis of large vessel vasculitis. Clin Exp Rheumatol. 2008;26(3 Suppl 49):S47–52.
Lee YH, Choi SJ, Ji JD, Song GG. Diagnostic accuracy of 18F-FDG PET or PET/CT for large vessel vasculitis : a meta-analysis. Z Rheumatol. 2016;75(9):924–31. https://doi.org/10.1007/s00393-015-1674-2.
Grayson PC, Alehashemi S, Bagheri AA, Civelek AC, Cupps TR, Kaplan MJ, et al. (18) F-Fluorodeoxyglucose-positron emission tomography as an imaging biomarker in a prospective, longitudinal cohort of patients with large vessel vasculitis. Arthritis Rheumatol. 2018;70(3):439–49. https://doi.org/10.1002/art.40379.
Prieto-Pena D, Martinez-Rodriguez I, Loricera J, Banzo I, Calderon-Goercke M, Calvo-Rio V, et al. Predictors of positive (18)F-FDG PET/CT-scan for large vessel vasculitis in patients with persistent polymyalgia rheumatica. Semin Arthritis Rheum. 2018. https://doi.org/10.1016/j.semarthrit.2018.05.007.
Schinkel AF, van den Oord SC, van der Steen AF, van Laar JA, Sijbrands EJ. Utility of contrast-enhanced ultrasound for the assessment of the carotid artery wall in patients with Takayasu or giant cell arteritis. Eur Heart J Cardiovasc Imaging. 2014;15(5):541–6. https://doi.org/10.1093/ehjci/jet243.
Dikkes A, Aschwanden M, Imfeld S, Glatz K, Messerli J, Staub D, et al. Takayasu arteritis: active or not, that's the question. Rheumatology (Oxford). 2017;56(10):1818–9. https://doi.org/10.1093/rheumatology/kex213.
Germano G, Macchioni P, Possemato N, Boiardi L, Nicolini A, Casali M, et al. Contrast-enhanced ultrasound of the carotid artery in patients with large vessel vasculitis: correlation with positron emission tomography findings. Arthritis Care Res. 2017;69(1):143–9. https://doi.org/10.1002/acr.22906.
Herlin B, Baud JM, Chadenat ML, Pico F. Contrast-enhanced ultrasonography in Takayasu arteritis: watching and monitoring the arterial inflammation. BMJ Case Rep 2015;2015. doi:https://doi.org/10.1136/bcr-2015-211094.
Schmidt WA. Ultrasound in the diagnosis and management of giant cell arteritis. Rheumatology (Oxford). 2018;57(suppl_2):ii22–31. https://doi.org/10.1093/rheumatology/kex461.
Prieto-Gonzalez S, Garcia-Martinez A, Tavera-Bahillo I, Hernandez-Rodriguez J, Gutierrez-Chacoff J, Alba MA, et al. Effect of glucocorticoid treatment on computed tomography angiography detected large-vessel inflammation in giant-cell arteritis. A prospective, longitudinal study. Medicine (Baltimore). 2015;94(5):e486. https://doi.org/10.1097/MD.0000000000000486.
Quinn KA, Ahlman MA, Malayeri AA, Marko J, Civelek AC, Rosenblum JS, et al. Comparison of magnetic resonance angiography and (18)F-fluorodeoxyglucose positron emission tomography in large-vessel vasculitis. Ann Rheum Dis. 2018;77(8):1165–71. https://doi.org/10.1136/annrheumdis-2018-213102. This study compares use of MRA and FDG-PET in the assessment of large-vessel vasculitis. Many patients in this study had evidence of disease activity on both MRA and PET imaging during periods of clinical remission.
Barra L, Kanji T, Malette J, Pagnoux C, CanVasc. Imaging modalities for the diagnosis and disease activity assessment of Takayasu’s arteritis: a systematic review and meta-analysis. Autoimmun Rev. 2018;17(2):175–87. https://doi.org/10.1016/j.autrev.2017.11.021.
Blockmans D, Bley T, Schmidt W. Imaging for large-vessel vasculitis. Curr Opin Rheumatol. 2009;21(1):19–28. https://doi.org/10.1097/BOR.0b013e32831cec7b.
Blockmans D, de Ceuninck L, Vanderschueren S, Knockaert D, Mortelmans L, Bobbaers H. Repetitive 18F-fluorodeoxyglucose positron emission tomography in giant cell arteritis: a prospective study of 35 patients. Arthritis Rheum. 2006;55(1):131–7. https://doi.org/10.1002/art.21699.
Both M, Ahmadi-Simab K, Reuter M, Dourvos O, Fritzer E, Ullrich S, et al. MRI and FDG-PET in the assessment of inflammatory aortic arch syndrome in complicated courses of giant cell arteritis. Ann Rheum Dis. 2008;67(7):1030–3. https://doi.org/10.1136/ard.2007.082123.
Lee KH, Cho A, Choi YJ, Lee SW, Ha YJ, Jung SJ, et al. The role of (18) F-fluorodeoxyglucose-positron emission tomography in the assessment of disease activity in patients with takayasu arteritis. Arthritis Rheum. 2012;64(3):866–75. https://doi.org/10.1002/art.33413.
Soussan M, Nicolas P, Schramm C, Katsahian S, Pop G, Fain O, et al. Management of large-vessel vasculitis with FDG-PET: a systematic literature review and meta-analysis. Medicine (Baltimore). 2015;94(14):e622. https://doi.org/10.1097/MD.0000000000000622.
Scheel AK, Meller J, Vosshenrich R, Kohlhoff E, Siefker U, Muller GA, et al. Diagnosis and follow up of aortitis in the elderly. Ann Rheum Dis. 2004;63(11):1507–10. https://doi.org/10.1136/ard.2003.015651.
Newman KA, Ahlman MA, Hughes M, Malayeri AA, Pratt D, Grayson PC. Diagnosis of giant cell arteritis in an asymptomatic patient. Arthritis Rheumatol. 2016;68(5):1135. https://doi.org/10.1002/art.39517.
Misra R, Danda D, Rajappa SM, Ghosh A, Gupta R, Mahendranath KM, et al. Development and initial validation of the Indian Takayasu Clinical Activity Score (ITAS2010). Rheumatology (Oxford). 2013;52(10):1795–801. https://doi.org/10.1093/rheumatology/ket128.
Reichenbach S, Adler S, Bonel H, Cullmann JL, Kuchen S, Butikofer L, et al. Magnetic resonance angiography in giant cell arteritis: results of a randomized controlled trial of tocilizumab in giant cell arteritis. Rheumatology (Oxford). 2018;57(6):982–6. https://doi.org/10.1093/rheumatology/key015.
Arnaud L, Haroche J, Malek Z, Archambaud F, Gambotti L, Grimon G, et al. Is (18)F-fluorodeoxyglucose positron emission tomography scanning a reliable way to assess disease activity in Takayasu arteritis? Arthritis Rheum. 2009;60(4):1193–200. https://doi.org/10.1002/art.24416.
Kerr GS, Hallahan CW, Giordano J, Leavitt RY, Fauci AS, Rottem M, et al. Takayasu arteritis. Ann Intern Med. 1994;120(11):919–29.
Ostberg G. Morphological changes in the large arteries in polymyalgia arteritica. Acta Med Scand Suppl. 1972;533:135–59.
Banerjee S QK, Gribbons KB, Rosenblum JS, Civelek A, Novakovich E, Bagheri A, Merkel PA, Ahlman MA, Grayson PC. Effect of specific treatments on clinical, serologic, and imaging assessments of disease activity in large-vessel vasculitis [abstract]. Arthritis Rheumatol. 2018; 70 (suppl 10).
Dellavedova L, Carletto M, Faggioli P, Sciascera A, Del Sole A, Mazzone A, et al. The prognostic value of baseline (18)F-FDG PET/CT in steroid-naive large-vessel vasculitis: introduction of volume-based parameters. Eur J Nucl Med Mol Imaging. 2016;43(2):340–8. https://doi.org/10.1007/s00259-015-3148-9.
Nuenninghoff DM, Hunder GG, Christianson TJ, McClelland RL, Matteson EL. Incidence and predictors of large-artery complication (aortic aneurysm, aortic dissection, and/or large-artery stenosis) in patients with giant cell arteritis: a population-based study over 50 years. Arthritis Rheum. 2003;48(12):3522–31. https://doi.org/10.1002/art.11353.
de Boysson H, Daumas A, Vautier M, Parienti JJ, Liozon E, Lambert M, et al. Large-vessel involvement and aortic dilation in giant-cell arteritis. A multicenter study of 549 patients. Autoimmun Rev. 2018;17(4):391–8. https://doi.org/10.1016/j.autrev.2017.11.029.
Nielsen BD, Gormsen LC, Hansen IT, Keller KK, Therkildsen P, Hauge EM. Three days of high-dose glucocorticoid treatment attenuates large-vessel 18F-FDG uptake in large-vessel giant cell arteritis but with a limited impact on diagnostic accuracy. Eur J Nucl Med Mol Imaging. 2018;45(7):1119–28. https://doi.org/10.1007/s00259-018-4021-4.
Lee VS, Martin DJ, Krinsky GA, Rofsky NM. Gadolinium-enhanced MR angiography: artifacts and pitfalls. AJR Am J Roentgenol. 2000;175(1):197–205. https://doi.org/10.2214/ajr.175.1.1750197.
Youngstein T, Tombetti E, Mukherjee J, Barwick TD, Al-Nahhas A, Humphreys E, et al. FDG uptake by prosthetic arterial grafts in large vessel vasculitis is not specific for active disease. JACC Cardiovasc Imaging. 2017;10(9):1042–52. https://doi.org/10.1016/j.jcmg.2016.09.027.
Berger CT, Sommer G, Aschwanden M, Staub D, Rottenburger C, Daikeler T. The clinical benefit of imaging in the diagnosis and treatment of giant cell arteritis. Swiss Med Wkly. 2018;148:w14661. https://doi.org/10.4414/smw.2018.14661.
Aydin SZ, Yilmaz N, Akar S, Aksu K, Kamali S, Yucel E, et al. Assessment of disease activity and progression in Takayasu’s arteritis with Disease Extent Index-Takayasu. Rheumatology (Oxford). 2010;49(10):1889–93. https://doi.org/10.1093/rheumatology/keq171.
Nakagomi D, Cousins C, Sznajd J, Furuta S, Mohammad AJ, Luqmani R, et al. Development of a score for assessment of radiologic damage in large-vessel vasculitis (Combined Arteritis Damage Score, CARDS). Clin Exp Rheumatol. 2017;35(Suppl 103(1)):139–45.
Tombetti E, Godi C, Ambrosi A, Doyle F, Jacobs A, Kiprianos AP, et al. Novel angiographic scores for evaluation of large vessel vasculitis. Sci Rep. 2018;8(1):15979. https://doi.org/10.1038/s41598-018-34395-7.
Jiemy WF, Heeringa P, Kamps J, van der Laken CJ, Slart R, Brouwer E. Positron emission tomography (PET) and single photon emission computed tomography (SPECT) imaging of macrophages in large vessel vasculitis: current status and future prospects. Autoimmun Rev. 2018;17(7):715–26. https://doi.org/10.1016/j.autrev.2018.02.006.
Funding
This research was supported through the Intramural Research Program at the National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Vasculitis
Rights and permissions
About this article
Cite this article
Quinn, K.A., Grayson, P.C. The Role of Vascular Imaging to Advance Clinical Care and Research in Large-Vessel Vasculitis. Curr Treat Options in Rheum 5, 20–35 (2019). https://doi.org/10.1007/s40674-019-00114-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40674-019-00114-0