Abstract
Purpose
One in five adults with chronic kidney disease (CKD) in the United States (US) suffers from depression. Comorbid depression in adults with CKD is associated with higher morbidity and mortality. This study used US national survey data to examine patterns and predictors of depression treatment among adults with non-dialysis-dependent CKD in the US.
Methods
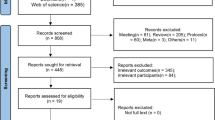
A retrospective, cross-sectional study was conducted using 2014–2015 National Ambulatory Medical Care Survey (NAMCS) data. The final study sample consisted of visits by 9.02 million adults (unweighted n = 262; age ≥ 18 years) with CKD and depression in the US. Depression treatment was defined as antidepressant use with or without psychotherapy. To identify predictors of depression treatment, multivariable logistic regression analysis was conducted adjusting for predisposing, enabling, and need factors.
Results
Approximately half of adults with CKD and depression received depression treatment. Primary care was the main setting of treatment, and the most commonly prescribed antidepressant class was selective serotonin reuptake inhibitors. Adults being seen for treatment of a chronic problem were 3.2 times more likely to receive depression treatment (OR 3.20; 95% CI 1.38–7.21). In addition, there was a 9% higher likelihood of receiving depression treatment for each unit increase in total number of medications (OR 1.09; 95% CI 1.01–1.19). Finally, adults receiving care in the South were 63% less likely to receive depression treatment (OR 0.37; 95% CI 0.15–0.89).
Conclusions
Depression treatment was recorded in approximately half of US ambulatory care visits involving adults with CKD and depression from 2014 to 2015. Further research is warranted to determine how to appropriately manage treatment of depression in adults with CKD.
Similar content being viewed by others
References
Hedayati SS, Minhajuddin AT, Toto RD, Morris DW, Rush AJ (2009) Prevalence of major depressive episode in CKD. Am J Kidney Dis 54(3):424–432. https://doi.org/10.1053/j.ajkd.2009.03.017
Palmer S, Vecchio M, Craig JC, Tonelli M, Johnson DW, Nicolucci A, Pellegrini F, Saglimbene V, Logroscino G, Fishbane S, Strippoli GF (2013) Prevalence of depression in chronic kidney disease: systematic review and meta-analysis of observational studies. Kidney Int 84(1):179–191. https://doi.org/10.1038/ki.2013.77
Lee YJ, Kim MS, Cho S, Kim SR (2013) Association of depression and anxiety with reduced quality of life in patients with predialysis chronic kidney disease. Int J Clin Pract 67(4):363–368. https://doi.org/10.1111/ijcp.12020
D’Onofrio G, Simeoni M, Rizza P, Caroleo M, Capria M, Mazzitello G, Sacco T, Mazzuca E, Panzino MT, Cerantonio A, Segura-Garcia C, Andreucci M, De Fazio P, Fuiano G (2017) Quality of life, clinical outcome, personality and coping in chronic hemodialysis patients. Ren Fail 39(1):45–53. https://doi.org/10.1080/0886022X.2016.1244077
Fischer MJ, Kimmel PL, Greene T, Gassman JJ, Wang X, Brooks DH, Charleston J, Dowie D, Thornley-Brown D, Cooper LA, Bruce MA, Kusek JW, Norris KC, Lash JP, Group AS (2011) Elevated depressive affect is associated with adverse cardiovascular outcomes among African Americans with chronic kidney disease. Kidney Int 80(6):670–678. https://doi.org/10.1038/ki.2011.153
Kop WJ, Seliger SL, Fink JC, Katz R, Odden MC, Fried LF, Rifkin DE, Sarnak MJ, Gottdiener JS (2011) Longitudinal association of depressive symptoms with rapid kidney function decline and adverse clinical renal disease outcomes. Clin J Am Soc Nephrol 6(4):834–844. https://doi.org/10.2215/CJN.03840510
Hedayati SS, Minhajuddin AT, Afshar M, Toto RD, Trivedi MH, Rush AJ (2010) Association between major depressive episodes in patients with chronic kidney disease and initiation of dialysis, hospitalization, or death. JAMA 303(19):1946–1953. https://doi.org/10.1001/jama.2010.619
Palmer SC, Vecchio M, Craig JC, Tonelli M, Johnson DW, Nicolucci A, Pellegrini F, Saglimbene V, Logroscino G, Hedayati SS, Strippoli GF (2013) Association between depression and death in people with CKD: a meta-analysis of cohort studies. Am J Kidney Dis 62(3):493–505. https://doi.org/10.1053/j.ajkd.2013.02.369
Tsai YC, Chiu YW, Hung CC, Hwang SJ, Tsai JC, Wang SL, Lin MY, Chen HC (2012) Association of symptoms of depression with progression of CKD. Am J Kidney Dis 60(1):54–61. https://doi.org/10.1053/j.ajkd.2012.02.325
Chiang HH, Guo HR, Livneh H, Lu MC, Yen ML, Tsai TY (2015) Increased risk of progression to dialysis or death in CKD patients with depressive symptoms: a prospective 3-year follow-up cohort study. J Psychosom Res 79(3):228–232. https://doi.org/10.1016/j.jpsychores.2015.01.009
Hedayati SS, Gregg LP, Carmody T, Jain N, Toups M, Rush AJ, Toto RD, Trivedi MH (2017) Effect of sertraline on depressive symptoms in patients with chronic kidney disease without dialysis dependence: the CAST randomized clinical trial. JAMA 318(19):1876–1890. https://doi.org/10.1001/jama.2017.17131
Walther CP, Shah AA, Winkelmayer WC (2017) Treating depression in patients with advanced CKD: beyond the generalizability frontier. JAMA 318(19):1873–1874. https://doi.org/10.1001/jama.2017.17553
Duarte PS, Miyazaki MC, Blay SL, Sesso R (2009) Cognitive-behavioral group therapy is an effective treatment for major depression in hemodialysis patients. Kidney Int 76(4):414–421. https://doi.org/10.1038/ki.2009.156
Lii YC, Tsay SL, Wang TJ (2007) Group intervention to improve quality of life in haemodialysis patients. J Clin Nurs 16(11C):268–275. https://doi.org/10.1111/j.1365-2702.2007.01963.x
Rocha Augusto C, Krzesinski JM, Warling X, Smelten N, Etienne AM (2011) [The role of psychological interventions in dialysis: an exploratory study]. Nephrol Ther 7(4):211–218. https://doi.org/10.1016/j.nephro.2010.12.006
National Centers for Disease Control and Prevention: National Center for Health Statistics. Ambulatory Health Care Data
Survey NAMC (2014) Data documentation. ftp://ftp.cdc.gov/pub/Health_Statistics/NCHS/Dataset_Documentation/NAMCS/doc2014.pdf. Accessed 4 June 2018
Survey NAMC (2015) Data documentation. ftp://ftp.cdc.gov/pub/Health_Statistics/NCHS/Dataset_Documentation/NAMCS/doc2015.pdf. Accessed 4 June 2018
Zenlea IS, Milliren CE, Mednick L, Rhodes ET (2014) Depression screening in adolescents in the United States: a national study of ambulatory office-based practice. Acad Pediatr 14(2):186–191. https://doi.org/10.1016/j.acap.2013.11.006
Hing E, Schappert SM, Burt CW, Shimizu IM (2005) Effects of form length and item format on response patterns and estimates of physician office and hospital outpatient department visits. National Ambulatory Medical Care Survey and National Hospital Ambulatory Medical Care Survey, 2001. Vital Health Stat 2(139):1–32
Anderson JG, Bartkus DE (1973) Choice of medical care: a behavioral model of health and illness behavior. J Health Soc Behav 14(4):348–362
CDC (2015) Reliability of estimates. https://www.cdc.gov/nchs/ahcd/ahcd_estimation_reliability.htm. Accessed 4 June 2018
Fischer MJ, Xie D, Jordan N, Kop WJ, Krousel-Wood M, Kurella Tamura M, Kusek JW, Ford V, Rosen LK, Strauss L, Teal VL, Yaffe K, Powe NR, Lash JP, Investigators CSG (2012) Factors associated with depressive symptoms and use of antidepressant medications among participants in the Chronic Renal Insufficiency Cohort (CRIC) and Hispanic-CRIC Studies. Am J Kidney Dis 60(1):27–38. https://doi.org/10.1053/j.ajkd.2011.12.033
Nagler EV, Webster AC, Vanholder R, Zoccali C (2012) Antidepressants for depression in stage 3–5 chronic kidney disease: a systematic review of pharmacokinetics, efficacy and safety with recommendations by European Renal Best Practice (ERBP). Nephrol Dial Transplant 27(10):3736–3745. https://doi.org/10.1093/ndt/gfs295
Glassman AH, O’Connor CM, Califf RM, Swedberg K, Schwartz P, Bigger JT Jr, Krishnan KR, van Zyl LT, Swenson JR, Finkel MS, Landau C, Shapiro PA, Pepine CJ, Mardekian J, Harrison WM, Barton D, McLvor M (2002) Sertraline antidepressant heart attack randomized trial. Sertraline treatment of major depression in patients with acute MI or unstable angina. JAMA 288(6):701–709
Cohen LM, Tessier EG, Germain MJ, Levy NB (2004) Update on psychotropic medication use in renal disease. Psychosomatics 45(1):34–48. https://doi.org/10.1176/appi.psy.45.1.34
Levy NB, Blumenfield M, Beasley CM Jr, Dubey AK, Solomon RJ, Todd R, Goodman A, Bergstrom RR (1996) Fluoxetine in depressed patients with renal failure and in depressed patients with normal kidney function. Gen Hosp Psychiatry 18(1):8–13
Atalay H, Solak Y, Biyik M, Biyik Z, Yeksan M, Uguz F, Guney I, Tonbul HZ, Turk S (2010) Sertraline treatment is associated with an improvement in depression and health-related quality of life in chronic peritoneal dialysis patients. Int Urol Nephrol 42(2):527–536. https://doi.org/10.1007/s11255-009-9686-y
Kamo T, Horikawa N, Tsuruta Y, Miyasita M, Hatakeyama H, Maebashi Y (2004) Efficacy and pharmacokinetics of fluvoxamine maleate in patients with mild depression undergoing hemodialysis. Psychiatry Clin Neurosci 58(2):133–137
Kalender B, Ozdemir AC, Yalug I, Dervisoglu E (2007) Antidepressant treatment increases quality of life in patients with chronic renal failure. Ren Fail 29(7):817–822. https://doi.org/10.1080/08860220701573517
Kennedy SH, Craven JL, Rodin GM (1989) Major depression in renal dialysis patients: an open trial of antidepressant therapy. J Clin Psychiatry 50(2):60–63
Lee SK, Lee HS, Lee TB, Kim DH, Koo JR, Kim YK, Son BK (2004) The effects of antidepressant treatment on serum cytokines and nutritional status in hemodialysis patients. J Korean Med Sci 19(3):384–389. https://doi.org/10.3346/jkms.2004.19.3.384
Koo JR, Yoon JY, Joo MH, Lee HS, Oh JE, Kim SG, Seo JW, Lee YK, Kim HJ, Noh JW, Lee SK, Son BK (2005) Treatment of depression and effect of antidepression treatment on nutritional status in chronic hemodialysis patients. Am J Med Sci 329(1):1–5
Turk S, Atalay H, Altintepe L, Guney I, Okudan N, Tonbul HZ, Gokbel H, Kucur R, Yeksan M, Yildiz A (2006) Treatment with antidepressive drugs improved quality of life in chronic hemodialysis patients. Clin Nephrol 65(2):113–118
Blumenfield M, Levy NB, Spinowitz B, Charytan C, Beasley CM Jr, Dubey AK, Solomon RJ, Todd R, Goodman A, Bergstrom RF (1997) Fluoxetine in depressed patients on dialysis. Int J Psychiatry Med 27(1):71–80
Wuerth D, Finkelstein SH, Kliger AS, Finkelstein FO (2003) Chronic peritoneal dialysis patients diagnosed with clinical depression: results of pharmacologic therapy. Semin Dial 16(6):424–427
Palmer SC, Natale P, Ruospo M, Saglimbene VM, Rabindranath KS, Craig JC, Strippoli GF (2016) Antidepressants for treating depression in adults with end-stage kidney disease treated with dialysis. Cochrane Database Syst Rev. https://doi.org/10.1002/14651858.CD004541.pub3
Shirazian S, Grant CD, Aina O, Mattana J, Khorassani F, Ricardo AC (2017) Depression in chronic kidney disease and end-stage renal disease: similarities and differences in diagnosis, epidemiology, and management. Kidney Int Rep 2(1):94–107. https://doi.org/10.1016/j.ekir.2016.09.005
Cohen SD, Norris L, Acquaviva K, Peterson RA, Kimmel PL (2007) Screening, diagnosis, and treatment of depression in patients with end-stage renal disease. Clin J Am Soc Nephrol 2(6):1332–1342. https://doi.org/10.2215/CJN.03951106
Hedayati SS, Yalamanchili V, Finkelstein FO (2012) A practical approach to the treatment of depression in patients with chronic kidney disease and end-stage renal disease. Kidney Int 81(3):247–255. https://doi.org/10.1038/ki.2011.358
Doyle GD, Laher M, Kelly JG, Byrne MM, Clarkson A, Zussman BD (1989) The pharmacokinetics of paroxetine in renal impairment. Acta Psychiatr Scand Suppl 350:89–90
Eyler RF, Unruh ML, Quinn DK, Vilay AM (2015) Psychotherapeutic agents in end-stage renal disease. Semin Dial 28(4):417–426. https://doi.org/10.1111/sdi.12370
Anttila SA, Leinonen EV (2001) A review of the pharmacological and clinical profile of mirtazapine. CNS Drug Rev 7(3):249–264
Marin H, Menza MA (2005) The management of fatigue in depressed patients. Essent Psychopharmacol 6(4):185–192
Foley KF, DeSanty KP, Kast RE (2006) Bupropion: pharmacology and therapeutic applications. Expert Rev Neurother 6(9):1249–1265. https://doi.org/10.1586/14737175.6.9.1249
Angermann CE, Gelbrich G, Stork S, Gunold H, Edelmann F, Wachter R, Schunkert H, Graf T, Kindermann I, Haass M, Blankenberg S, Pankuweit S, Prettin C, Gottwik M, Bohm M, Faller H, Deckert J, Ertl G, Investigators M-HS, Committee M (2016) Effect of escitalopram on all-cause mortality and hospitalization in patients with heart failure and depression: the MOOD-HF randomized clinical trial. JAMA 315(24):2683–2693. https://doi.org/10.1001/jama.2016.7635
O’Connor CM, Jiang W, Kuchibhatla M, Silva SG, Cuffe MS, Callwood DD, Zakhary B, Stough WG, Arias RM, Rivelli SK, Krishnan R, Investigators S-C (2010) Safety and efficacy of sertraline for depression in patients with heart failure: results of the SADHART-CHF (sertraline against depression and heart disease in chronic heart failure) trial. J Am Coll Cardiol 56(9):692–699. https://doi.org/10.1016/j.jacc.2010.03.068
Cipriani A, Furukawa TA, Salanti G, Geddes JR, Higgins JP, Churchill R, Watanabe N, Nakagawa A, Omori IM, McGuire H, Tansella M, Barbui C (2009) Comparative efficacy and acceptability of 12 new-generation antidepressants: a multiple-treatments meta-analysis. Lancet 373(9665):746–758. https://doi.org/10.1016/S0140-6736(09)60046-5
Hedayati SS, Daniel DM, Cohen S, Comstock B, Cukor D, Diaz-Linhart Y, Dember LM, Dubovsky A, Greene T, Grote N, Heagerty P, Katon W, Kimmel PL, Kutner N, Linke L, Quinn D, Rue T, Trivedi MH, Unruh M, Weisbord S, Young BA, Mehrotra R (2016) Rationale and design of A trial of sertraline vs. cognitive behavioral therapy for end-stage renal disease patients with depression (ASCEND). Contemp Clin Trials 47:1–11. https://doi.org/10.1016/j.cct.2015.11.020
Blane D, Williams C, Morrison J, Wilson A, Mercer S (2013) Cognitive behavioural therapy: why primary care should have it all. Br J Gen Pract 63(607):103–104. https://doi.org/10.3399/bjgp13X663235
Chiu YW, Teitelbaum I, Misra M, de Leon EM, Adzize T, Mehrotra R (2009) Pill burden, adherence, hyperphosphatemia, and quality of life in maintenance dialysis patients. Clin J Am Soc Nephrol 4(6):1089–1096. https://doi.org/10.2215/CJN.00290109
Bhattacharjee S, Axon DR, Goldstone L, Lee JK (2018) Patterns and predictors of depression treatment among stroke survivors with depression in ambulatory settings in the United States. J Stroke Cerebrovasc Dis 27(3):563–567. https://doi.org/10.1016/j.jstrokecerebrovasdis.2017.09.047
Funding
This research did not receive any grants from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
For this type of study, formal consent is not required.
Rights and permissions
About this article
Cite this article
Vadiei, N., Bhattacharjee, S. Patterns and predictors of depression treatment among adults with chronic kidney disease and depression in ambulatory care settings in the United States. Int Urol Nephrol 51, 303–309 (2019). https://doi.org/10.1007/s11255-018-2034-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-018-2034-3