Abstract
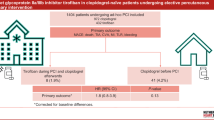
The long-term pharmacodynamic effects of Ticagrelor versus Clopidogrel in patients undergoing early percutaneous coronary intervention (PCI) after fibrinolytic therapy is unknown. From May 2014 to August 2016, 212 patients undergoing PCI within 24 h of Tenecteplase (TNK), Aspirin, and Clopidogrel for ST-elevated myocardial infarction (STEMI) were randomized at four Canadian sites to receive additional Clopidogrel or Ticagrelor initiated prior to PCI. The platelet reactivity units (PRU) were measured with the VerifyNow Assay before study drug administration (baseline), at 4 and 24 h post PCI, and follow-up appointment. A mixed-model analysis with time as the repeated measure and drug as the between-subjects factor was calculated using 2 separate 1 × 4 ANOVAs, with students t-tests used to compare drugs within each time point. Complete clinical follow-up data (median 115.0 days; IQR 80.3–168.8) was available in 50 patients (23.6%) randomized to either Clopidogrel (n = 23) or Ticagrelor (n = 27). Analyses revealed significant decreases in PRU from baseline to 4 h (261.4 vs. 71.7; Mdiff = − 189.7; p < 0.001) to 24 h (71.7 vs. 27.7; Mdiff = − 44.0; p < 0.001) to end of follow-up (27.7 vs.17.9; Mdiff = − 9.9. p = 0.016) for those randomized to Ticagrelor and significant decreases in PRU only from baseline to 4 h (271.3 vs. 200.8; Mdiff = − 70.5, p = < 0.001) in patients receiving Clopidogrel, and a significantly greater proportion of patients with adequate platelet inhibition (PRU < 208) on long-term follow-up (Clopidogrel, 82.6% vs. Ticagrelor, 100.0%; p = 0.038). Our results demonstrate that in patients undergoing PCI within 24 h of fibrinolysis for STEMI, Ticagrelor provides prolonged platelet inhibition compared with Clopidogrel.



Similar content being viewed by others
References
O’Gara PT, Kushner FG, Ascheim DD et al (2013) 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: a report of the American college of cardiology foundation/american heart association task force on practice guidelines. J Am Coll Cardiol. https://doi.org/10.1016/j.jacc.2012.11.019
Hsia RY, Shen YC (2016) Percutaneous coronary intervention in the United States: risk factors for untimely access. Health Serv Res 51:592–609. https://doi.org/10.1111/1475-6773.12335
Alexopoulos D, Perperis A, Koniari I et al (2015) Ticagrelor versus high dose clopidogrel in ST-segment elevation myocardial infarction patients with high platelet reactivity post fibrinolysis. J Thromb Thrombolysis 40:261–267. https://doi.org/10.1007/s11239-015-1183-9
Storey RF, Angiolillo DJ, Patil SB et al (2010) Inhibitory effects of ticagrelor compared with clopidogrel on platelet function in patients with acute coronary syndromes: the PLATO (PLATelet inhibition and patient Outcomes) PLATELET substudy. J Am Coll Cardiol 56:1456–1462. https://doi.org/10.1016/j.jacc.2010.03.100
Gurbel PA, Bliden KP, Butler K et al (2009) Randomized double-blind assessment of the ONSET and OFFSET of the antiplatelet effects of ticagrelor versus clopidogrel in patients with stable coronary artery disease: the ONSET/OFFSET study. Circulation 120:2577–2585. https://doi.org/10.1161/CIRCULATIONAHA.109.912550
Rittenhouse DR, Shortell SM, Fisher ES (2009) Ticagrelor versus clopidogrel in patients with acute coronary syndromes. N Engl J Med. https://doi.org/10.1056/NEJMoa0904327
Dehghani P, Lavoie A, Lavi S et al (2017) Effects of ticagrelor versus clopidogrel on platelet function in fibrinolytic-treated STEMI patients undergoing early PCI. Am Heart J. https://doi.org/10.1016/j.ahj.2017.07.013
Hochholzer W, Ruff CT, Mesa RA et al (2014) Variability of individual platelet reactivity over time in patients treated with clopidogrel: insights from the ELEVATE-TIMI 56 trial. J Am Coll Cardiol 64:361–368. https://doi.org/10.1016/j.jacc.2014.03.051
Gorog DA, Otsui K, Inoue N (2015) Usefulness of platelet function tests to predict bleeding with antithrombotic medications. Cardiol Rev 23:323–327. https://doi.org/10.1097/crd.0000000000000072
Aradi D, Kirtane A, Bonello L et al (2015) Bleeding and stent thrombosis on P2Y 12 -inhibitors: collaborative analysis on the role of platelet reactivity for risk stratification after percutaneous coronary intervention. Eur Heart J 36:1762–1771. https://doi.org/10.1093/eurheartj/ehv104
Alexopoulos D, Xanthopoulou I, Gkizas V et al (2012) Randomized assessment of ticagrelor versus prasugrel antiplatelet effects in patients with ST-segment-elevation myocardial infarction. Circ Cardiovasc Interv 5:797–804. https://doi.org/10.1161/CIRCINTERVENTIONS.112.972323
Perl L, Zemer-Wassercug N, Rechavia E et al (2015) Comparison of platelet inhibition by prasugrel versus ticagrelor over time in patients with acute myocardial infarction. J Thromb Thrombolysis 39:1–7. https://doi.org/10.1007/s11239-014-1119-9
Angiolillo DJ, Curzen N, Gurbel P et al (2014) Pharmacodynamic evaluation of switching from ticagrelor to prasugrel in patients with stable coronary artery disease: results of the swap-2 study (switching anti platelet-2). J Am Coll Cardiol 63:1500–1509. https://doi.org/10.1016/j.jacc.2013.11.032
Laine M, Gaubert M, Frere C et al (2015) COMparison of Platelet reactivity following prAsugrel and ticagrelor loading dose in ST-segment elevation myocardial infarctION patients: the COMPASSION study. Platelets 26:570–572. https://doi.org/10.3109/09537104.2014.959914
Alexopoulos D, Gkizas V, Patsilinakos S et al (2013) Double versus standard loading dose of ticagrelor: onset of antiplatelet action in patients with stemi undergoing primary PCI. J Am Coll Cardiol 62:940–941. https://doi.org/10.1016/j.jacc.2013.05.021
Kirtane AJ, Parikh PB, Stuckey TD et al (2015) Is there an ideal level of platelet P2Y12-receptor inhibition in patients undergoing percutaneous coronary intervention? “window” Analysis from the ADAPT-DES study (Assessment of Dual AntiPlatelet Therapy with Drug-Eluting Stents). JACC Cardiovasc Interv 8:1978–1987. https://doi.org/10.1016/j.jcin.2015.08.032
Gurbel PA, Bliden KP, Butler K et al (2010) Response to ticagrelor in clopidogrel nonresponders and responders and effect of switching therapies: the RESPOND study. Circulation 121:1188–1199. https://doi.org/10.1161/CIRCULATIONAHA.109.919456
Alexopoulos D, Galati A, Xanthopoulou I et al (2012) Ticagrelor versus prasugrel in acute coronary syndrome patients with high on-clopidogrel platelet reactivity following percutaneous coronary intervention: a pharmacodynamic study. J Am Coll Cardiol 60:193–199. https://doi.org/10.1016/j.jacc.2012.03.050
Wu H, Qian J, Sun A et al (2012) Association of CYP2C19 genotype with periprocedural myocardial infarction after uneventful stent implantation in Chinese patients receiving clopidogrel pretreatment. Circ J. https://doi.org/10.1253/circj.CJ-12-0635
Sinhal AR, Aylward PE (2013) New antiplatelet agents and the role of platelet function testing in acute coronary syndromes. Clin Ther 35:1064–1068. https://doi.org/10.1016/j.clinthera.2013.07.429
Siller-Matula JM, Trenk D, Schrör K et al (2013) Response variability to P2Y12 receptor inhibitors: expectations and reality. JACC Cardiovasc Interv 6:1111–1128. https://doi.org/10.1016/j.jcin.2013.06.011
Alexopoulos D, Xanthopoulou I, Storey RF et al (2014) Platelet reactivity during ticagrelor maintenance therapy: a patient-level data meta-analysis. Am Heart J 168:530–536. https://doi.org/10.1016/j.ahj.2014.06.026
Funding
This study was made possible by funding provided by AstraZeneca.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Andrew Yang, Quin Pon, Jennifer Crawford, Sebastian Harenberg, Sheila Kelly, and Shamir R. Mehta have no conflicts of interest. Payam Dehghani has received significant research grant, and modest speaking honoraria from Astra Zeneca. Andrea Lavoie has received modest speaking honoraria from Astra Zeneca. Rodney Zimmermann has has received modest speaking honoraria from Astra Zeneca. Jeff Booker has received modest speaking honoraria from Astra Zeneca. Shahar Lavi has received significant research grant from Astra Zeneca. Warren J Cantor has participated in advisory boards and has received modest speaking honoraria. Akshay Bagai has received modest honoraria for speaking/consulting from Astra Zeneca. Shaun Goodman reports significant research grant support and modest speaker/consulting honoraria from AstraZeneca, Bayer, Bristol-Myers Squibb/Sanofi, Daiichi-Sankyo, and Lilly. Asim Cheema has received significant research grant from Astra Zeneca.
Ethical approval
The study complied with the Declaration of Helsinki and with International Conference on Harmonization/Good Clinical Practice guidelines, and was approved by local ethics board of all the participating institutions.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Yang, A., Pon, Q., Lavoie, A. et al. Long-term pharmacodynamic effects of Ticagrelor versus Clopidogrel in fibrinolytic-treated STEMI patients undergoing early PCI. J Thromb Thrombolysis 45, 225–233 (2018). https://doi.org/10.1007/s11239-017-1581-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11239-017-1581-2