Abstract
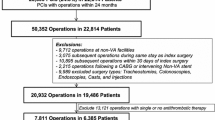
The objective of this study was to determine 3-month cumulative incidence of peri-procedural thromboembolism (TE) including graft occlusion, and peri-procedural bleeding for chronically anticoagulated vascular bypass graft (BG) patients requiring temporary warfarin interruption for an invasive procedure. Appropriate peri-procedural management of patients receiving chronic warfarin therapy to preserve lower extremity arterial BG patency is unknown. In a protocol driven, cohort study design, all BG patients referred to the Mayo Clinic Thrombophilia Center for peri-procedural anticoagulation (1997–2007) were followed forward in time to estimate the 3-month cumulative incidence of TE and bleeding. Decisions to provide “bridging” low molecular weight heparin (LMWH) were individualized based on estimated risk of TE and bleeding. There were 78 BG patients (69 ± 10 years; 38 % women), of whom 73 % had a distal autogenous and 53 % had prosthetic BG; 45 % received antiplatelet therapy. Peri-procedural LMWH was prescribed for 77 % of patients and did not vary by BG distal anastomosis location or type. The 3-month cumulative incidence of TE was 5.1 % (95 % CI 1.4–12.6), including two BG occlusions, one DVT, and one myocardial infarction. Major bleeding occurred in 1 patient (1.28 %, 95 % CI 0.0–6.94). One patient died due to heart failure. TE and bleeding did not differ by bridging status. The 3-month cumulative incidence of TE among BG patients in whom warfarin is temporarily interrupted for an invasive procedure may be higher than in other “bridging” populations (atrial fibrillation, prosthetic heart valve, venous thromboembolism). This finding underscores the often tenuous nature of distal bypass grafts necessitating an aggressive approach to peri-procedural anticoagulation management.

Similar content being viewed by others
References
Dutch Bypass Oral anticoagulants or Aspirin (BOA) Study Group (2000) Efficacy of oral anticoagulants compared with aspirin after infrainguinal bypass surgery (the Dutch bypass oral anticoagulants or aspirin study): a randomized trial. Lancet 355:346–351
Sarac TP, Huber TS, Back MR et al (1998) Warfarin improves the outcome of infrainguinal vein bypass grafting at high risk for failure. J Vasc Surg 28:446–457
Sobel M, Verhaeghe R (2008) Antithrombotic therapy for peripheral artery occlusive disease: American college of chest physicians evidence-based clinical practice guidelines (8th edition). Chest 133:815S–843S
Ansell J, Hirsh J, Hylek E, Jacobson A, Crowther M, Palareti G (2008) Pharmacology and management of the vitamin K antagonists: American college of chest physicians evidence-based clinical practice guidelines (8th edition). Chest 133:160S–198S
Douketis JD, Berger PB, Dunn AS (2008) The perioperative management of antithrombotic therapy: American college of chest physicians evidence-based clinical practice guidelines (8th edition). Chest 133:299S–339S
Daniels PR, McBane RD, Litin SC et al (2009) Peri-procedural anticoagulation management of mechanical prosthetic heart valve patients. Thromb Res 124:300–305
Kovacs MJ, Kearon C, Rodger M et al (2004) Single-arm study of bridging therapy with low-molecular-weight heparin for patients at risk of arterial embolism who require temporary interruption of warfarin. Circulation 110:1658–1663
Wysokinski WE, McBane RD, Daniels PR et al (2008) periprocedural anticoagulation management of patients with nonvalvular atrial fibrillation. Mayo Clin Proc 83:639–645
Spyropoulos AC, Turpie AG, Dunn AS et al (2006) Clinical outcomes with unfractionated heparin or low-molecular-weight heparin as bridging therapy in patients on long-term oral anticoagulants: the REGIMEN registry. J Thromb Haemost 4:1246–1252
McBane RD, Wysokinski WE, Daniels PR et al (2010) Periprocedural anticoagulation management of patients with venous thromboembolism. Arterioscler Thromb Vasc Biol 30:442–448
Dunn AS, Spyropoulos AC, Turpie AG (2007) Bridging therapy in patients on long-term oral anticoagulants who require surgery: the Prospective Peri-operative Enoxaparin Cohort Trial (PROSPECT). J Thromb Haemost 5:2211–2218
Douketis JD, Foster GA, Crowther MA et al (2000) Clinical risk factors and timing of recurrent venous thromboembolism during the initial 3 months of anticoagulant therapy. Arch Intern Med 160:3431–3436
Thatipelli MR, Pellikka PA, McBane RD et al (2007) Prognostic value of ankle-brachial index and dobutamine stress echocardiography for cardiovascular morbidity and all-cause mortality in patients with peripheral arterial disease. J Vasc Surg 46:62–70
Gillum RF, Fortmann SP, Prineas RJ, Kottke TE (1984) International diagnostic criteria for acute myocardial infarction and acute stroke. Am Heart J 108:150–158
Schulman S, Kearon C (2005) Definition of major bleeding in clinical investigations of antihemostatic medicinal products in non-surgical patients. J Thromb Haemost 3:692–694
Pomposelli FB, LoGerfo FW (2005) The autogenous vein. In: Rutherford RB, Cronenwett JL, Gloviczki P, Johnston KW, Krupski WC, Ouriel K, Sidawy AN (eds) Rutherford Vascular Surgery, 6th edn. Elsevier Saunders, Philadelphia, pp 695–715
Xu L, Greisler HP (2005) Prosthetic grafts. In: Rutherford RB, Cronenwett JL, Gloviczki P, Johnston KW, Krupski WC, Ouriel K, Sidawy AN (eds) Rutherford Vascular Surgery, 6th edn. Elsevier Saunders, Philadelphia, pp 723–740
Wengerter KR, Veith FJ, Gupta SK et al (1991) Prospective randomized multicenter comparison of in situ and reversed vein infrapopliteal bypasses. J Vasc Surg 13:189–197
Watelet J, Soury P, Menard JF et al (1997) Femoropopliteal bypass: in situ or reversed vein grafts? ten-year results of a randomized prospective study. Ann Vasc Surg 11(5):510–519
Moody AP, Edwards PR, Harris PL (1992) In situ versus reversed femoropopliteal vein grafts: long-term follow-up of a prospective, randomized trial. Br J Surg 79:750–752
Veith FJ, Gupta SK, Ascer E et al (1986) Six-year prospective multicenter randomized comparison of autologous saphenous vein and expanded polytetrafluoroethylene grafts in infrainguinal arterial reconstructions. J Vasc Surg 3:104–114
Klinkert P, Schepers A, Burger DH, van Bockel JH, Breslau PJ (2003) Vein versus polytetrafluoroethylene in above-knee femoropopliteal bypass grafting: five-year results of a randomized controlled trial. J Vasc Surg 37:149–155
Johnson WC, Lee KK (2000) A comparative evaluation of polytetrafluoroethylene, umbilical vein, and saphenous vein bypass grafts for femoral-popliteal above-knee revascularization: a prospective randomized Department of Veterans Affairs Cooperative Study. J Vasc Surg 32:268–277
Hirsch AT, Haskal ZJ, Hertzer NR et al (2006) American Association for Vascular Surgery, Society for Vascular Surgery, Society for Cardiovascular Angiography and Interventions, Society for Vascular Medicine and Biology, Society of Interventional Radiology, ACC/AHA Task Force on Practice Guidelines Writing Committee to Develop Guidelines for the Management of Patients With Peripheral Arterial Disease, American Association of Cardiovascular and Pulmonary Rehabilitation, National Heart, Lung, and Blood Institute, Society for Vascular Nursing, TransAtlantic Inter-Society Consensus, Vascular Disease Foundation. Circulation 113:e463–e654
de Vries SO, Hunink MG (1997) Results of aortic bifurcation grafts for aortoiliac occlusive disease: a meta-analysis. J Vasc Surg 26:558–569
McBane RD 2nd, Karnicki K, Miller RS, Owen WG (2004) The impact of peripheral arterial disease on circulating platelets. Thromb Res 113:137–145
Madsen EH, Gehr NR, Johannesen NL, Schmidt EB, Kristensen SR (2011) Platelet response to aspirin and clopidogrel in patients with peripheral atherosclerosis. Platelets 22(7):537–546 (Epub 2011 May 19)
Acknowledgments
Funded, in part, by grants from the Centers for Disease Control and Prevention (DD00235), US Public Health Service, and by Mayo Foundation.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Attaya, H., Wysokinski, W.E., Bower, T. et al. Three-month cumulative incidence of thromboembolism and bleeding after periprocedural anticoagulation management of arterial vascular bypass patients. J Thromb Thrombolysis 35, 100–106 (2013). https://doi.org/10.1007/s11239-012-0787-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11239-012-0787-6