Abstract
Research has demonstrated that first responders may develop psychological trauma/ posttraumatic stress disorder (PTSD) in the performance of their duties. Often overlooked in these studies of police, firefighters, and paramedics is an additional group of providers in this health care delivery system: the trauma surgeons, who receive the victims transported by the first responders. Although limited in scope, the research literature does identify the presence of PTSD in trauma surgeons. These studies have repeatedly cited the need for further information about psychological trauma for trauma surgeons. This paper addresses that need with a brief overview of psychological trauma, where surgeons may encounter victims, and how to cope with its aftermath.
Similar content being viewed by others
References
Flannery RB Jr. The violent person: professional risk management strategies for safety and care. American Mental Health Foundation: New York; 2009.
Flannery RB Jr. Treating psychological trauma in first responders: a multi-modal paradigm. Psychiatry Q. 2015;86:261–7.
Wilson LC. A systematic review of probable posttraumatic stress disorder in first responders following man-made mass violence. Psychiatry Res. 2015;229:21–6.
Haugen PT, McCrillis AM, Smid GE, et al. Mental health stigma and barriers to healthcare for first responders: a systematic review and meta-analysis. J Psychiatr Res. 2017;94:218–29.
Lewis-Schroeder NF, Kieran K, Murphy BL, Wolff JD, Robinson MA, Kaufman ML. Conceptualization, assessment, and treatment of traumatic stress in first responders: a review of critical issues. Harv Rev Psychiatry. 2018;26:216–27.
Bezabh YH, Abebe SM, Fanta T, et al. Prevalence and associated factors of posttraumatic disorder among emergency responders of Addis Ababa fire and emergency control and prevention service authority, Ethiopia: Institution-based cross-sectional study. BMJ Open. 2018;8(7):e020705. https://doi.org/10.1136/bmjopen-2017-020705.
Kim JI, Park H, Kim J-H. The mediation effect of PTSD, perceived job stress, and resilience on the relationship between trauma exposure and development of depression and alcohol use in Korean firefighters: a cross-sectional study. J Affect Disord. 2018;229:450–5.
Patel AM, Ingalls NK, Mansour MA, et al. Collateral damage: the effect of patient complications on the surgeon’s psyche. Surgery. 2010;48:824–8.
Pinto A, Faiz O, Vincent C, et al. Surgical complications and their implications for surgeons’ well-being. Br J Surg. 2013;100:1748–55.
Warren AM, Jones AL, Shafi S, Roden-Foreman K, Bennett MM, Foreman ML. Does caring for trauma patients lead to psychological stress in surgeons? J Trauma Acute Care Surg. 2013;75:179–84.
Pinto A, Faiz O, Bicknell C, et al. Acute traumatic stress among surgeons after major medical complications. Am J Surg. 2014;4:642–7.
Thompson CV, Naumann DN, Fellows JL, Bowley DM, Suggett N. Post-traumatic stress disorder amongst surgical trainees: an unrecognized risk? Surgeon. 2017;15:123–30.
Havron WS 3rd, Safcsak K, Corsa J, et al. Psychological effect of a mass casualty event on genera; surgery residents. J Surg Edu. 2017;74:74–80.
Han K, Bohnen JD, Peponis T, Martinez M, Nandan A, Yeh DD, et al. The surgeon as second victim? Results of the Boston intraoperative adverse events surgeons’ attitude (BISA) study. J Am Coll Surg. 2017;224:1048–56.
Luftman K, Aydelotte J, Rix K, Ali S, Houck K, Coopwood TB, et al. PTSD in those who care for the injured. Injury. 2017;48:293–6.
Biggs S, Waggett HB, Shabbir J. Impact of surgical complications on the operating surgeon. Colorectal Dis. 2020. https://doi.org/10.1111/codi.15021.
Kent J, Thornton M, Fong A, Hall E, Fitzgibbons S, Sava J. Acute provider stress in high stakes medical care: implications for trauma surgeons. J Trauma Acute Care Surg. 2020;88:440–5.
Flannery RB Jr. Posttraumatic stress disorder: the victim’s guide to healing and recovery. 2nd ed. American Mental Health Foundation: New York; 2012.
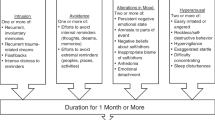
American Psychiatric Association. The diagnostic and statistical manual of mental disorders (DSM-5). Fifth ed. Washington, DC: American Psychiatric Association Press; 2013.
Alarcon LH, Germain A, Clontz AS, Roach E, Nicholas DH, Zenati MS, et al. Predictors of acute posttraumatic stress disorder following civilian trauma: highest incidence and severity of symptoms after assault. J Trauma Acute Care Surg. 2012;72:629–35.
Latz D, Bergermann A, Jungnitsch J, Grassmann JP, Schiffner E, Gahr B, et al. Characteristics of victims of violence in the A&E department and analysis of acceptance of medico-legal expertize center after its implementation vs. multi-year consolidation. Z Orthop Unfall. 2019;157:426–33.
Sink EL, Hyman JE, Matheny T, Georgopoulos G, Kleinman P. Child abuse: the role of the orthopedic surgeon in nonaccidental trauma. Clin Orthop Relat Res. 2011;469:790–7.
Hull AM, Lowe T, Finlay PM. The psychological impact of maxillofacial trauma: an overview of reactions to trauma. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2003;95:515–20.
Guth AA, Pachter L. Domestic violence and the trauma surgeon. Am J Surg. 2000;179:134–40.
Bhandari M, Dosanjh S, Tornetta P 3rd, et al. Musculoskeletal manifestations of physical abuse after intimate partner violence. J Trauma. 2006;61:1473–9.
Callaway DW. A review of the landscape: Challenges and gaps in trauma response to civilian high threat mass casualty incidents. J Trauma Acute Care Surg. 2018;84(6S Suppl 1):S21–7.
Yadav SK, Shrestha S. A study on posttraumatic experience of road traffic accident afflicted maxillofacial trauma patient at tertiary hospital. J Nat Sci Biol Med. 2017;8:40–5.
Copanitsanou P, Drakoutos E, Kechagias V. Posttraumatic stress, depressive emotions, and satisfaction with life after a road accident. Orthop Nurs. 2018;37:43–53.
Percy DB, Streith L, Wong L, et al. Mental toughness in surgeons: is there room for improvement? Can J Surg. 2019;62:482–7.
Arora S, Sevdalis N, Nestel D, Tierney T, Woloshynowych M, Kneebone R. Managing intraoperative stress: what do surgeons want from a crisis training program? Am J Surg. 2009;197:537–43.
Robinson C, Lawless R, Zarzaur B, et al. Physiologic stress among surgeons who take in-house call. Am J Surg. 2019;218:1181–4.
Foa EB, Rothbaum BO. Treating the trauma of rape: cognitive behavioral therapy for PTSD. New York: Guilford Press; 1998.
Shapiro F. Eve movement desensitization and reprocessing: basic principles, protocols, and procedures. New York: Guilford Press; 1999.
Flannery RB Jr. The assaulted staff action program: coping with the psychological aftermath of violence. American Mental Health Foundation: New York; 2012.
Flannery RB Jr. The assaulted staff action program: thirty-year program analysis. Psychiatry Q. 2020;91:1011–5. https://doi.org/10.1007/s11126-020-09785-8.
Fernadez-Moure J, Pascual JL, Martin ND, et al. Emergency response teams in and outside of medicine-structurally crafted to be worlds apart. J Trauma Acute Care Surg. 2019;86:134–40.
Flannery RB Jr. Becoming stress-resistant through the project SMART program. American Mental Health Foundation: New York; 2012.
Vaillant G. Adaptation to life. Boston: Little Brown; 1977.
Author Statement
The author has no conflicts of interest nor grant funding sources to cite for this paper.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The author declares no conflicts of interest.
Human and Animal Standard and Informed Consent
This is a review of the literature article only. There were no human subjects and therefore no need for an IRB review, nor informed consent, nor committee involvement, and no need to obtain consent to publish. Similarly, there were no animals involved in this review with no need to discuss and present a statement and review of animal welfare in this project.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Flannery, R.B. Psychological Trauma and the Trauma Surgeon. Psychiatr Q 93, 27–33 (2022). https://doi.org/10.1007/s11126-020-09862-y
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11126-020-09862-y