Abstract
Background
Public safety personnel (PSP) are exposed to potentially psychologically traumatic events (PPTE) far more often than the general public, which increases the risk for various post-traumatic stress injuries (PTSIs). While there are many evidence-based psychological interventions for PTSI, the effectiveness of each intervention for PSP remains unclear.
Objectives
The current study assessed the effectiveness and acceptability of psychological interventions for PTSI among PSPs.
Methods
A systematic review and random-effects meta-analysis were performed on the effectiveness and acceptability of psychotherapies for PTSIs (i.e., symptoms of depression, anxiety, post-traumatic stress disorder) among PSP. The review adhered to the PRISMA reporting guidelines and used standardized mean differences (Cohen’s d), rate ratios (RR), and their 95% confidence intervals (95% CI) to measure pooled effect sizes across studies; negative d values and RR values less than one indicated a reduction in symptoms compared to baseline or control groups. In addition, heterogeneity was quantified using I2, and publication bias was evaluated using Egger’s test.
Results
The analyses included data from eight randomized controlled trials representing 402 PSP (79.4% male, 35.3 years). Psychological interventions included narrative exposure therapy (n = 1), cognitive behavioral therapy (n = 2), eclectic psychotherapy (n = 2), eye-movement desensitization and reprocessing (n = 1), supportive counseling (n = 2), and group critical incident stress debriefing (n = 1). The interventions were associated with statistically significant reductions in symptoms associated with PTSD (d = − 1.23; 95% CI − 1.81, − 0.65; 7 studies; I2 = 81%), anxiety (− 0.76; 95% CI − 1.28, − 0.24; 3 studies; I2 = 47%), and depression (d = − 1.10; 95% CI − 1.62, − 0.58; 5 studies; I2 = 64%). There were smaller but statistically significant improvements at follow-up for symptoms of PTSD (d = − 1.29 [− 2.31, − 0.27]), anxiety (d = − 0.82 [− 1.20, − 0.44]), and depression (d = − 0.46 [− 0.77, − 0.14]). There were no statistically significant differences in dropout rates (RR = 1.00 [0.96, 1.05]), suggesting high acceptability across interventions.
Conclusions
There is preliminary evidence that psychotherapies help treat PTSIs in PSP; however, the shortage of high-quality studies on PSP indicates a need for additional research into treating PTSI among PSP.
Systematic review registration
PROSPERO: CRD42019133534.
Similar content being viewed by others
Introduction
Exposure to potentially psychologically traumatic events (PPTE) can lead to many problematic mental health symptoms associated with various disorders, including but not limited to post-traumatic stress disorder (PTSD). Nearly 10% of Canadians meet the criteria for PTSD at any given time [1, 2]. The onset of PTSD in the general population typically occurs in persons in their mid to late twenties [3]. Women appear at twice the risk for PTSD [4, 5]. PTSD can involve substantial distress and impairment [6]. Nearly 75% of patients with PTSD meet the criteria for one or more comorbid psychiatric disorders [7, 8]. PTSD comorbidities exacerbate impairments to quality of life and functioning and are associated with an increased lifetime risk for attempted suicide [4, 7, 9]. PTSD costs the Canadian economy approximately $50 billion annually [10].
Epidemiologic studies have indicated the risk of developing PTSD and other post-traumatic stress injuries (PTSIs) is higher in populations with greater exposure to PPTEs [11,12,13,14,15,16,17]. For example, among military personnel and veterans exposed to combat-related violence, the lifetime prevalence of PTSD is as high as 31% [18,19,20,21,22,23]. Public safety personnel (PSP) are also exposed to PPTE more frequently than the general population [24,25,26,27,28,29,30]. The term PSP refers to several related occupations with professionals dedicated to maintaining public safety and wellbeing, such as border services officers, correctional workers, firefighters, paramedics, police, and public safety communicators (e.g., call center operators and 911 operators). The increased PPTE exposures among PSP increase their risk for PTSIs [25, 26, 31,32,33,34,35,36], including but not limited to PTSD, major depressive disorder, generalized anxiety disorder, and alcohol use disorder [25, 37]. In addition, PSPs are up to four times more likely to experience suicidal behaviors when compared to the general population [35]. The media has increasingly reported mental health risks for PSP, such as responding to the 2014 Moncton shootings [38].
In 2016, the Ministry of Public Safety and Emergency Preparedness at the University of Regina held a national roundtable on PSP mental health. A subsequent pan-Canadian PSP survey estimated that 44.5% of PSPs screened positive for at least one PTSI associated with PPTEs [25, 37]. Additional risk factors for PTSIs among PSP appear to include increased stigma [39, 40], lowered willingness to receive support [33], and difficulties accessing mental health resources [39,40,41]. The Canadian government has been expanding the scope of tailored mental health programs to serve all PSPs better [42]; however, there are critical knowledge gaps regarding best practices for treating PTSI among PSPs. For example, there is a substantial body of literature on PTSD interventions [43,44,45,46,47,48,49,50,51], but PSP-specific results remain scarce.
There is very limited research on the effectiveness of psychological interventions for PTSIs among PSPs. Previously published reviews have explored peripheral topics that are of relevance. For example, a recent meta-analysis found a positive but non-significant association between different types of training programs and coping skills among PSP populations [52]. A second meta-analysis found modest evidence for time-limited reductions in PTSI following participation in holistic programs that promote resilience, stress, and emotion regulation among at-risk workers [53]. Another systematic review investigated the effectiveness of organizational peer support and crisis-focused psychological interventions designed to mitigate PTSIs among PSP and other PPTE-exposed workers, producing heterogeneous results and precluding a quantitative meta-analysis [54]. No previous reviews or meta-analyses have examined the effectiveness of psychological interventions for PTSIs among PSPs. Therefore, the current study was designed to conduct a systematic review and meta-analysis of the effectiveness and acceptability of psychotherapies for PTSIs among PSPs.
Methods
Protocol and registration
The current study was registered with PROSPERO (CRD42019133534) [55] and reported per the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) [56].
Eligibility criteria
The population-intervention-comparison-outcome-study design (PICOS) model [57] was used to define review eligibility:
-
Population: adult (aged 18 and older) police, paramedics and emergency management technicians, correctional officers, dispatchers, 9-1-1 communication officers, and fire and safety officers.
-
Intervention: any psychological interventions approved by the American Psychological Association to treat PTSD, delivered alone or in combination with medications.
-
Comparison: any comparator condition, such as waitlist controls or no intervention.
-
Outcomes: self-report measures (e.g., symptom scores on psychopathology measures), remission for PTSIs (e.g., PTSD), and objective indices of functioning (e.g., absenteeism, occupational performance ratings).
-
Study design: English-language, peer-reviewed, randomized controlled trials (RCTs) of any duration from any geographic location published since 2008. We had opted to use 2008 to capture research articles published in the past 10 years at the time of the review’s inception to enrich the review with the most recent literature.
Information sources and search
A systematic search of Cochrane Central Register, EMBASE, MEDLINE, PsycINFO, and PubMed was performed from January 1, 2008, to October 8, 2019 (Appendix 1). The search was supplemented by reviewing the reference lists of included studies and searching for ongoing RCTs from trial registries.
Study selection
There were two co-authors (AB and PD) who independently screened all articles by title/abstract and then full texts using Cochrane’s Covidence, a web-based systematic review manager [58]. After removing duplicate citations, the initial screening selection of papers was verified at the title/abstract stage by having multiple reviewers screen 200 reports, with 99% agreement. Finally, all discrepancies were removed by consensus and third-party input (GA).
Data collection process
There were two co-authors (AB and PD) who independently extracted relevant data from the published full-text reports of each included article using Covidence. The data extracted was verified by one other author (AB, PD, or GA).
Data items
The following data items were extracted: sample size, age, sex, comorbidity status, and years of employment in the PSP profession; type and duration of psychological intervention; comparator group; all relevant outcome measures (e.g., symptom scores for PTSD and other PTSI on psychopathology measures); author, design, location, and study duration (i.e., timing of follow-up evaluations).
Risk of bias in individual studies
The Cochrane risk of bias tool for RCTs was used to assess study quality [59]. In brief, the Cochrane risk of bias tool appraises randomization, allocation concealment, blinding, selective reporting, attrition bias, and potential bias from funding. There were two co-authors (AB and PD) who independently appraised each included trial against the risk of bias tool, with discrepancies resolved by consensus.
Summary measures and synthesis of results
All analyses were performed in RStudio using the meta package [60]. Random-effects meta-analysis models were created to pool effect sizes for each psychotherapy's effectiveness and acceptability, and the results were graphed using Forest plots. The specific methods have been previously described [52, 61,62,63,64,65]. The I2 statistic was used to quantify heterogeneity, corresponding to the proportion of total variation (𝜏2) not due to random error [66]. Effect sizes were pooled across RCTs using standardized mean differences (SMD, Cohen’s d) or rate ratios (RRs) and their 95% confidence intervals (CI), depending on whether the data was continuous or categorical. The SMD was the difference in mean symptom severity scores at the end of intervention between groups divided by the standard deviation of the difference between groups. The SMD allowed the pooling of effect sizes across studies that measured the same construct using different scales, as the standardization corrects for between-scale differences. We harmonized the extraction of means and standard deviations for SMD calculations from the respective studies. A negative SMD indicates an improvement in symptom severity relative to the control condition. All confidence intervals containing zero were non-significant, given that an SMD of zero is null. RRs greater than 1 indicated that the result favored the experimental intervention over the control; 95% CIs containing an RR of 1 were non-significant.
Risk of bias across studies
Publication bias from the overrepresentation of studies with positive results was assessed using funnel plots [67] and Egger’s funnel plot symmetry test [68, 69].
Additional analyses
The effect sizes determined from the end-of-intervention were also compared to the end-of-follow-up to determine intervention-time effects.
Results
Study selection
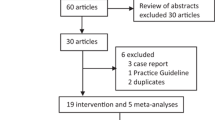
The search strategy identified 1493 unique records. After removing 1427 irrelevant documents during the title/abstract phase, the remaining 66 full-text articles were reviewed. The reviewed articles included 27 that involved an ineligible study design, 13 that used an unsuitable intervention, two from before 2008, and 2 that used incompatible outcomes (i.e., they did not report data compatible with a quantitative meta-analysis). Ultimately, eight RCTs met the inclusion criteria for the current review (Fig. 1). We repeated the PubMed search on August 13th, 2022. However, only one additional article was identified, but this study could not be included in the review as it was not a randomized controlled trial.
Quality assessment
Three RCTs out of the eight [70,71,72] met the criteria for being high quality as per the Cochrane Risk of Bias tool [70,71,72]. The remaining five RCTs met low to moderate quality (Table 6 in Appendix 2). Three RCTs out of the eight were double-blinded, while the remaining five were single- or unblinded [70,71,72]. All but one of the eight RCTs [73] thoroughly reported participant flow and attrition. All eight RCTs adequately randomized participants, but only four concealed intervention allocation [70,71,72, 74]. All eight studies provided their trial registration numbers and study protocols. Three RCTs out of the eight did not disclose funding sources [73,74,75].
Study and participant characteristics
There was considerable diversity in the PSP professions, psychotherapies, and outcome measures across the eight RCTs (Table 1). PSP professions included emergency service personnel, firefighters, and police officers, totalling 402 individuals across studies (79.4% male, mean age 35.3 years). The eight RCTs focused on several different interventions, including narrative exposure therapy (n = 1), cognitive behavioral therapy (n = 2), eclectic psychotherapy (n = 2), eye-movement desensitization and reprocessing (n = 1), supportive counseling (n = 2), and group critical incident stress debriefing (n = 1). Comparator conditions included waitlists (n = 3), psychoeducation only (n = 2), and non-specific supportive interventions (n = 1). Follow-up durations across the eight RCTs ranged from one to 12 months.
Psychotherapy effectiveness for PSP
The included RCTs evidenced reduced PTSD symptom severity at the completion of intervention (d = − 1.23; 95% CI − 1.81, − 0.65; 7 studies; I2 = 81%) and in sustained follow-up (d = − 1.29, 95% CI − 2.31, − 0.27; 6 studies; I2 = 89%; Fig. 2). The interventions appeared effective for reducing PTSD symptoms at intervention completion (RR = 1.81, 95% CI 1.18–2.79; 2 studies; I2 = 0%) that were sustained at follow-up (RR = 2.15, 95% CI 1.13–4.11; I2 = 29%). There were also statistically significant reductions in anxiety symptoms at intervention completion (d = − 0.76; 95% CI − 1.28, − 0.24; 3 studies; I2 = 47%) that were sustained at follow-up (d = − 0.82, 95% CI − 1.20, − 0.44; I2 = 0%; Fig. 3). There were also statistically significant reductions in depressive symptoms at intervention completion (d = − 1.10; 95% CI − 1.62, − 0.58; 5 studies; I2 = 64%) that were sustained at follow-up (d = − 0.46, 95% CI − 0.77, − 0.14; I2 = 15%; Fig. 4). All meta-analytic estimates are summarized in Table 7 in Appendix 3.
Acceptability of psychotherapies
There were no statistically significant differences in retention at intervention completion (RR = 1.00; 95% CI 0.96, 1.05; 8 studies; I2 = 0%) or at follow-up (RR = 1.00, 95% CI 0.95, 1.05; I2 = 0%; Figure 5 in Appendix 4).
Risk of bias across studies
The overall risk of publication bias appears low because all funnel plots were grossly symmetric, and none of the quantitative tests for publication bias reached statistical significance (Figure 6 in Appendix 5).
Additional analyses
The low number of RCTs eligible for inclusion (n = 8) prohibited conducting subgroup and meta-regression analyses.
Discussion
The current study is the first meta-analysis of psychotherapeutic interventions for PTSIs among PSPs. The results supported the effectiveness of narrative exposure therapy, cognitive behavioral therapy, eclectic psychotherapy, eye movement desensitization and reprocessing, and trauma processing therapy for PSPs experiencing PTSD, depression, or anxiety symptoms. For most interventions, the effects were sustained at follow-up, indicating the durability of benefits. Across the studies, there was minimal attrition, supporting the interventions’ acceptability among participating PSPs. The evidence suggests several effective and acceptable psychotherapies for PTSD, depression, and anxiety symptoms among PSP. Ultimately, our current results represent an updated synthesis of the literature on the role of psychological interventions for PTSIs among PSP and can serve as a starting point for more high-quality research that could expand on some initial results.
Ongoing advances in our understanding of PTSD and trauma-focused interventions are occurring alongside increasing recognition that professionals with extensive PPTE exposures (e.g., military, veterans, PSP) are experiencing high levels of PTSI. There are also similarities and occupation-specific needs when managing PPTE sequelae among diverse professional groups. For example, two recent reviews found limited evidence supporting the effectiveness of proactive (e.g., resilience promotion) [53] and post-exposure peer support and crisis-focused psychological interventions (e.g., critical incident stress debriefing, stress management, peer support, psychological first aid, trauma risk management) in mitigating PTSIs among PSP and frontline healthcare personnel [54]. The extant literature for PTSI management among PSP includes multiple therapeutic approaches, study designs (i.e., experimental, observational), and outcome measures (e.g., psychopathology self-report measures, clinician-rated functional assessments, and occupational indices such as absenteeism) [54]. Advancements have been made over the past few decades in understanding and treating symptoms of PTSD. Still, the rising number of professionals repeatedly exposed to PPTE continues to be a serious international public health problem, especially in light of operating during the global COVID-19 pandemic [78]. PPTE exposure is nearly ubiquitous [79, 80]. Nevertheless, individuals with more frequent PPTE exposures are at increased risk for PTSIs [81]. For example, approximately 20% of the two million troops deployed to Iraq may have required intervention for PTSD, whereas the population prevalence of PTSD among the deployed troops is less than 10% [82].
Most studies with PPTE-exposed participants have focused on military and veteran populations. There are fewer studies exploring PSP. Accordingly, results from military and veterans are often extrapolated to PSP. There is evidence that first-line PPTE-focused interventions (e.g., cognitive processing therapy, prolonged exposure therapy) produce clinically meaningful improvements for military personnel with PTSD; however, non-response rates among military personnel appear much higher than in civilians [83]. In addition, military participants in PTSD intervention studies who initially respond to intervention report poorer long-term follow-up outcomes than civilian participants [84]. Overall attrition rates appear similar between military and civilian participants receiving intervention for PTSD; however, particular subgroups, such as persons with PTSD related to combat or assault, tend to have poorer intervention outcomes, and are more likely to drop out of follow-up [84]. The relatively lower response to interventions for PTSIs among military and veteran populations, coupled with the near absence of RCT evidence with PSP, underscores the need for additional research and intervention development for people repeatedly exposed to PPTE. The knowledge base regarding PPTE exposures and PTSIs is rapidly expanding with novel research and public priorities to support PSP.
Limitations
As with any review, the current work has limitations that contextualize the present results’ generalizability and provide future research directions. First, the eligibility criteria limited the included research results to RCTs to minimize bias from confounding variables. High-quality psychotherapy trials are scarce due to inherent methodological challenges such as patient selection, outcome criteria, lack of controls, and difficulty with blinding [85,86,87]. Only three of the eight RCTs included in the current meta-analysis met the high-quality criteria per the Cochrane Risk of Bias tool [70,71,72]. Pooling outcomes across potentially heterogeneous populations may have violated meta-analytic assumptions; however, most heterogeneity indices were low, supporting the decision to pool interventions and outcomes across studies. Given the variable trial quality across studies, estimations of intervention effectiveness may have been inflated. Publication bias was low, but restricting the search strategy to English-language articles published after 2008 may have excluded relevant studies. Finally, few studies provided measurements of long-term outcomes, the longest of which was at 12 months of follow-up, limiting assessments of sustained impact. PSPs who receive intervention are very likely to be re-exposed to numerous subsequent PPTE, which suggests the impact of any single intervention may be offset by one or more new PTSI, which necessarily hampers interpretations of sustained intervention impact.
Future studies
There is a need for ongoing research on PTSIs among PSP [23, 88]. The current review focused on RCTs, but non-RCT designs remain a potentially valuable source of information for advancing the state of knowledge on PTSIs among PSPs. For example, a non-randomized study by Berking and colleagues found evidence that police officers who received manualized emotion regulation training demonstrated superior skill application and improved subject mental health ratings [89]. Additional randomized and non-randomized trials are needed to inform further intervention modalities and delivery models that may be particularly beneficial for PSP, such as internet-based cognitive behavior therapy [31, 42].
Conclusions
There is preliminary evidence that psychotherapies help treat PTSIs in PSP; however, the shortage of high-quality studies justifies a need for additional studies investigating the intervention of PTSIs among PSP.
Availability of data and materials
Data will be made available upon request on ResearchGate and Mendeley.
References
Kennedy SH, Lam RW, McIntyre RS, Tourjman SV, Bhat V, Blier P, et al. Canadian Network for Mood and Anxiety Treatments (CANMAT) 2016 clinical guidelines for the management of adults with major depressive disorder. Can J Psychiatry Rev Can Psychiatr. 2016;61:540–60.
Katzman MA, Bleau P, Blier P, Chokka P, Kjernisted K, Van Ameringen M. Canadian clinical practice guidelines for the management of anxiety, posttraumatic stress and obsessive-compulsive disorders. BMC Psychiatry. 2014;14:S1.
Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the national comorbidity survey replication. Arch Gen Psychiatry. 2005;62:593–602.
Pietrzak RH, Goldstein RB, Southwick SM, Grant BF. Prevalence and Axis I comorbidity of full and partial posttraumatic stress disorder in the United States: results from Wave 2 of the National Epidemiologic Survey on Alcohol and Related Conditions. J Anxiety Disord. 2011;25:456–65.
Stein MB, Walker JR, Hazen AL, Forde DR. Full and partial posttraumatic stress disorder: findings from a community survey. Am J Psychiatry. 1997;154:1114–9.
Westphal M, Olfson M, Gameroff MJ, Wickramaratne P, Pilowsky DJ, Neugebauer R, et al. Functional impairment in adults with past posttraumatic stress disorder: findings from primary care. Depress Anxiety. 2011;28:686–95.
Kessler RC, Chiu WT, Demler O, Walters EE. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the national comorbidity survey replication. Arch Gen Psychiatry. 2005;62:617–27.
Van Ameringen M, Mancini C, Patterson B, Boyle MH. Post-traumatic stress disorder in Canada. CNS Neurosci Ther. 2008;14:171–81.
Ginzburg K, Ein-Dor T, Solomon Z. Comorbidity of posttraumatic stress disorder, anxiety and depression: a 20-year longitudinal study of war veterans. J Affect Disord. 2010;123:249–57.
Anxiety and depression cost the Canadian economy almost $50 billion a year. Glob. News. Available from: https://globalnews.ca/news/2917922/anxiety-and-depression-cost-the-canadian-economy-almost-50-billion-a-year/. Cited 2019 Oct 4.
Felitti VJ, Anda RF, Nordenberg D, Williamson DF, Spitz AM, Edwards V, et al. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. The Adverse Childhood Experiences (ACE) Study. Am J Prev Med. 1998;14:245–58.
Felitti VJ, Anda RF, Nordenberg D, Williamson DF, Spitz AM, Edwards V, et al. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: the Adverse Childhood Experiences (ACE) Study. Am J Prev Med. 2019;56:774–86.
Atwoli L, Platt JM, Basu A, Williams DR, Stein DJ, Koenen KC. Associations between lifetime potentially traumatic events and chronic physical conditions in the South African Stress and Health Survey: a cross-sectional study. BMC Psychiatry. 2016;16:214.
Conversano C, Carmassi C, Bertelloni CA, Marchi L, Micheloni T, Carbone MG, et al. Potentially traumatic events, post-traumatic stress disorder and post-traumatic stress spectrum in patients with fibromyalgia. Clin Exp Rheumatol. 2019;37(Suppl 116):39–43.
Forman-Hoffman VL, Bose J, Batts KR, Glasheen C, Hirsch E, Karg RS, et al. Correlates of lifetime exposure to one or more potentially traumatic events and subsequent posttraumatic stress among adults in the United States: results from the mental health surveillance study, 2008-2012. In: CBHSQ Data Rev. Rockville: Substance Abuse and Mental Health Services Administration (US); 2012. Available from: http://www.ncbi.nlm.nih.gov/books/NBK390285/. Cited 2019 Sep 10.
Forman-Hoffman V, Batts K, Bose J, Glasheen C, Hirsch E, Yu F, et al. Correlates of exposure to potentially traumatic experiences: results from a national household survey. Psychol Trauma Theory Res Pract Policy. 2019;11(3):360–7.
Overstreet C, Berenz EC, Sheerin C, Amstadter AB, Canino G, Silberg J. Potentially traumatic events, posttraumatic stress disorder, and depression among adults in Puerto Rico. Front Psychol. 2016;7 Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4815006/. Cited 2019 Sep 10.
Cardona RA, Ritchie EC. U.S. military enlisted accession mental health screening: history and current practice. Mil Med. 2007;172:31–5.
Vun E, Turner S, Sareen J, Mota N, Afifi TO, El-Gabalawy R. Prevalence of comorbid chronic pain and mental health conditions in Canadian Armed Forces active personnel: analysis of a cross-sectional survey. CMAJ Open. 2018;6:E528–36.
Thompson JM, VanTil LD, Zamorski MA, Garber B, Dursun S, Fikretoglu D, et al. Mental health of Canadian Armed Forces Veterans: review of population studies. J Mil Veteran Fam Health. 2016;2:70–86.
Rebeira M, Grootendorst P, Coyte P. Factors associated with mental health in Canadian Veterans. J Mil Veteran Fam Health. 2017; Available from: https://jmvfh.utpjournals.press/doi/abs/10.3138/jmvfh.4098. Cited 2019 Oct 4.
Oster C, Morello A, Venning A, Redpath P, Lawn S. The health and wellbeing needs of veterans: a rapid review. BMC Psychiatry. 2017;17 Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5747125/. Cited 2019 Oct 4.
Williamson V, Stevelink SAM, Greenberg K, Greenberg N. Prevalence of mental health disorders in elderly U.S. military veterans: a meta-analysis and systematic review. Am J Geriatr Psychiatry Off J Am Assoc Geriatr Psychiatry. 2018;26:534–45.
Groll D. Understanding the prevalence of mental health disorders in provincial correctional officers - a national study. 2018. Available from: http://webapps.cihr-irsc.gc.ca/decisions/p/project_details.html?applId=392622&lang=en. Cited 2019 Oct 4.
Carleton RN, Afifi TO, Turner S, Taillieu T, Duranceau S, LeBouthillier DM, et al. Mental disorder symptoms among public safety personnel in Canada. Can J Psychiatry Rev Can Psychiatr. 2018;63:54–64.
Turner S, Taillieu T, Carleton RN, Sareen J, Afifi TO. Association between a history of child abuse and suicidal ideation, plans and attempts among Canadian public safety personnel: a cross-sectional survey. CMAJ Open. 2018;6:E463–70.
Carleton N. Pan Canadian public safety personnel: ongoing knowledge translation and strategic development. 2018. Available from: http://webapps.cihr-irsc.gc.ca/decisions/p/project_details.html?applId=392550&lang=en. Cited 2019 Oct 4.
Garb HN, Wood JM, Baker M. The Lackland Behavioral Questionnaire: the use of biographical data and statistical prediction rules for public safety screening. Psychol Assess. 2018;30:1039–48.
Suyama J, Rittenberger JC, Patterson PD, Hostler D. Comparison of public safety provider injury rates. Prehospital Emerg Care Off J Natl Assoc EMS Physicians Natl Assoc State EMS Dir. 2009;13:451–5.
Sloan IH, Rozensky RH, Kaplan L, Saunders SM. A shooting incident in an elementary school: effects of worker stress on public safety, mental health, and medical personnel. J Trauma Stress. 1994;7:565–74.
Carleton N, Beshai S. Peer support and crisis-focused psychological intervention programs in Canadian First Responders: blue paper: University of Regina; 2016. Available from: https://www.justiceandsafety.ca/rsu_docs/blue_paper_full_web_final_production_aug_16_2016.pdf. Cited 2019 Oct 4
Carleton RN, Afifi TO, Taillieu T, Turner S, El-Gabalawy R, Sareen J, et al. Anxiety-related psychopathology and chronic pain comorbidity among public safety personnel. J Anxiety Disord. 2018;55:48–55.
Carleton RN, Afifi TO, Turner S, Taillieu T, Vaughan AD, Anderson GS, et al. Mental health training, attitudes toward support, and screening positive for mental disorders. Cogn Behav Ther. 2019:1–19.
Carleton RN, Korol S, Mason JE, Hozempa K, Anderson GS, Jones NA, et al. A longitudinal assessment of the road to mental readiness training among municipal police. Cogn Behav Ther. 2018;47:508–28.
Stanley IH, Hom MA, Joiner TE. A systematic review of suicidal thoughts and behaviors among police officers, firefighters, EMTs, and paramedics. Clin Psychol Rev. 2016;44:25–44.
Alavi N. Delivering online cognitive behavioural therapy (iCBT) to address mental health challenges in correctional officers and other public safety personnel. 2018. Available from: http://webapps.cihr-irsc.gc.ca/decisions/p/project_details.html?applId=392550&lang=en. Cited 2019 Oct 4.
Ricciardelli R, Carleton RN, Mitchell M, Barnim N, Bahji A, Groll D. Correctional work, wellbeing, and mental health disorders. Adv Correct J. 2019;8:53–69.
CBC News. 3 RCMP officers dead, 2 wounded in Moncton, N.B., shooting: CBC; 2014. Available from: https://www.cbc.ca/news/canada/new-brunswick/moncton-shootings-3-rcmp-officers-dead-2-wounded-1.2665359. Cited 2019 Oct 4
Ricciardelli R. “Risk it out, risk it out”: occupational and organizational stresses in rural policing. Police Q. 2018;21:415–39.
Ricciardelli R, Power N, Medeiros DS. Correctional officers in Canada: interpreting workplace violence. Crim Justice Rev. 2018;43:458–76.
Ricciardelli R. Understanding the impact of prison work on the mental health of Correctional Officers employed by Correctional Services Canada: Beginning a longitudinal study. 2018. Available from: http://webapps.cihr-irsc.gc.ca/decisions/p/project_details.html?applId=392540&lang=en. Cited 2019 Oct 4.
Supporting Canada’s public safety personnel: an action plan on post-traumatic stress injuries. 2019. Available from: https://www.publicsafety.gc.ca/cnt/rsrcs/pblctns/2019-ctn-pln-ptsi/index-en.aspx. Cited 2019 Sep 10.
Bisson J, Andrew M. Psychological treatment of post-traumatic stress disorder (PTSD). Cochrane Database Syst Rev. 2007:CD003388.
Bisson J, Andrew M. Psychological treatment of post-traumatic stress disorder (PTSD). Cochrane Database Syst Rev. 2005:CD003388.
Bisson JI, Roberts NP, Andrew M, Cooper R, Lewis C. Psychological therapies for chronic post-traumatic stress disorder (PTSD) in adults. Cochrane Database Syst Rev. 2013; Available from: https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD003388.pub4/full. Cited 2019 Nov 4.
Hetrick SE, Purcell R, Garner B, Parslow R. Combined pharmacotherapy and psychological therapies for post traumatic stress disorder (PTSD). Cochrane Database Syst Rev. 2010:CD007316.
Lawrence S, Silva MD, Henley R. Sports and games for post-traumatic stress disorder (PTSD). Cochrane Database Syst Rev. 2010; Available from: http://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD007171.pub2/full?highlightAbstract=withdrawn%7Cptsd. Cited 2019 Oct 13.
Lewis C, Roberts NP, Bethell A, Robertson L, Bisson JI. Internet-based cognitive and behavioural therapies for post-traumatic stress disorder (PTSD) in adults. Cochrane Database Syst Rev. 2018; Available from: https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD011710.pub2/full. Cited 2019 Nov 4.
Rose SC, Bisson J, Churchill R, Wessely S. Psychological debriefing for preventing post traumatic stress disorder (PTSD). Cochrane Database Syst Rev. 2002; Available from: http://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD000560/full. Cited 2019 Nov 5.
Sin J, Spain D, Furuta M, Murrells T, Norman I. Psychological interventions for post-traumatic stress disorder (PTSD) in people with severe mental illness. Cochrane Database Syst Rev. 2017; Available from: http://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD011464.pub2/full?highlightAbstract=withdrawn%7Cptsd. Cited 2019 Oct 13.
Stein DJ, Ipser JC, Seedat S, Sager C, Amos T. Pharmacotherapy for post traumatic stress disorder (PTSD). Cochrane Database Syst Rev. 2006; Available from: http://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD002795.pub2/full?highlightAbstract=withdrawn%7Cptsd. Cited 2019 Oct 13.
Di Nota P, Kasurak E, Bahji A, Groll D, Anderson G. Coping among public safety personnel: a systematic review and meta-analysis. Stress Health. 2021; Available from: https://onlinelibrary.wiley.com/doi/abs/10.1002/smi.3039. Cited 2021 Mar 9.
Di Nota PM, Bahji A, Groll D, Carleton RN, Anderson GS. Proactive psychological programs designed to mitigate posttraumatic stress injuries among at-risk workers: a systematic review and meta-analysis. Syst Rev. 2021;10:126.
Anderson GS, Di Nota PM, Groll D, Carleton RN. Peer support and crisis-focused psychological interventions designed to mitigate post-traumatic stress injuries among public safety and frontline healthcare personnel: a systematic review. Int J Environ Res Public Health. 2020;17(20):E7645.
National Institute for Health Research. PROSPERO international prospective register of systematic reviews. 2019. Available from: http://www.crd.york.ac.uk/PROSPERO/display_record.asp?ID=CRD42014006602.
Hutton B, Salanti G, Caldwell DM, Chaimani A, Schmid CH, Cameron C, et al. The PRISMA extension statement for reporting of systematic reviews incorporating network meta-analyses of health care interventions: checklist and explanations. Ann Intern Med. 2015;162:777–84 American College of Physicians.
Methley AM, Campbell S, Chew-Graham C, McNally R, Cheraghi-Sohi S. PICO, PICOS and SPIDER: a comparison study of specificity and sensitivity in three search tools for qualitative systematic reviews. BMC Health Serv Res. 2014;14 Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4310146/. Cited 2019 Apr 9.
Veritas Health Innovation. Covidence systematic review software. Melbourne; 2019.
Higgins JPT, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928.
Schwarzer G. meta: an R package for meta-analysis. USA: R; 2007. Available from: https://cran.r-project.org/web/packages/meta/meta.pdf. Cited 2019 Nov 3
Bahji A, Wong J, Khalid-Khan S. Psychotherapy for borderline personality disorder in adolescents: systematic review and meta-analysis. Eur Psychiatry. 2019;56:S30.
Bahji A, Forsyth A, Groll D, Hawken ER. Efficacy of 3,4-methylenedioxymethamphetamine (MDMA)-assisted psychotherapy for posttraumatic stress disorder: a systematic review and meta-analysis. Prog Neuropsychopharmacol Biol Psychiatry. 2020;96:109735.
Wong J, Bahji A, Khalid-Khan S. Psychotherapies for adolescents with subclinical and borderline personality disorder: a systematic review and meta-analysis. Can J Psychiatry. 2020;65:5–15 SAGE Publications Inc.
Bahji A, Cheng B, Gray S, Stuart H. Mortality among people with opioid use disorder: a systematic review and meta-analysis. J Addict Med. 2020;14:e118.
Bahji A, Carlone D, Altomare J. Acceptability and efficacy of naltrexone for criminal justice-involved individuals with opioid use disorder: a systematic review and meta-analysis. Addiction. 2020;115:1413–25.
Higgins JPT, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21:1539–58.
Duval S, Tweedie R. Trim and fill: a simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. Biometrics. 2000;56:455–63.
Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics. 1994;50:1088–101.
Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315:629–34.
Mithoefer MC, Mithoefer AT, Feduccia AA, Jerome L, Wagner M, Wymer J, et al. 3,4-methylenedioxymethamphetamine (MDMA)-assisted psychotherapy for post-traumatic stress disorder in military veterans, firefighters, and police officers: a randomised, double-blind, dose-response, phase 2 clinical trial. Lancet Psychiatry. 2018;5:486–97.
Bryant RA, Kenny L, Rawson N, Cahill C, Joscelyne A, Garber B, et al. Efficacy of exposure-based cognitive behaviour therapy for post-traumatic stress disorder in emergency service personnel: a randomised clinical trial. Psychol Med. 2019;49:1565–73.
Gersons BPR, Schnyder U. Learning from traumatic experiences with brief eclectic psychotherapy for PTSD. Eur J Psychotraumatol. 2013;4:21369 Taylor & Francis.
Chongruksa D, Parinyapol P, Sawatsri S, Pansomboon C. Efficacy of eclectic group counseling in addressing stress among Thai police officers in terrorist situations. Couns Psychol Q. 2012;25:83–96 Routledge.
Tuckey MR, Scott JE. Group critical incident stress debriefing with emergency services personnel: a randomized controlled trial. Anxiety Stress Coping. 2014;27:38–54 Routledge.
Jarero I, Amaya C, Givaudan M, Miranda A. EMDR individual protocol for paraprofessional use: a randomized controlled trial with first responders. J EMDR Pract Res. 2013;7:55–64.
Alghamdi M, Hunt N, Thomas S. The effectiveness of narrative exposure therapy with traumatised firefighters in Saudi Arabia: a randomized controlled study. Behav Res Ther. 2015;66:64–71.
Miller JK, Peart A, Soffia M. Can police be trained in trauma processing to minimise PTSD symptoms? Feasibility and proof of concept with a newly recruited UK police population. Police J, 2020:93(4):310–31.
Vujanovic AA, Lebeaut A, Leonard S. Exploring the impact of the COVID-19 pandemic on the mental health of first responders. Cogn Behav Ther. 2021;50(4):320–35.
Perrin M, Vandeleur CL, Castelao E, Rothen S, Glaus J, Vollenweider P, et al. Determinants of the development of post-traumatic stress disorder, in the general population. Soc Psychiatry Psychiatr Epidemiol. 2014;49:447–57.
Kilpatrick DG, Resnick HS, Milanak ME, Miller MW, Keyes KM, Friedman MJ. National estimates of exposure to traumatic events and PTSD prevalence using DSM-IV and DSM-5 criteria. J Trauma Stress. 2013;26:537–47.
American Psychiatric Association. DSM-V: diagnostic and statistical manual of mental disorders. 5th ed. Arlington: American Psychiatric Association; 2013. Available from: https://psychiatryonline.org/doi/book/10.1176/appi.books.9780890425596. Cited 2019 Jan 22
Steenkamp MM, Litz BT. Psychotherapy for military-related posttraumatic stress disorder: Review of the evidence. Clin Psychol Rev. 2013;33:45–53.
Steenkamp MM, Litz BT, Hoge CW, Marmar CR. Psychotherapy for military-related PTSD: a review of randomized clinical trials. JAMA. 2015;314:489–500.
Straud CL, Siev J, Messer S, Zalta AK. Examining military population and trauma type as moderators of treatment outcome for first-line psychotherapies for PTSD: a meta-analysis. J Anxiety Disord. 2019;67:102133.
Shean G. Limitations of randomized control designs in psychotherapy research. Adv Psychiatry. 2014; Available from: https://www.hindawi.com/journals/apsy/2014/561452/. Cited 2019 Dec 8.
Smith EG, Mathur A. Blinding in psychotherapy plus medication trials. Am J Psychiatry. 2006;163:1295.
Rifkin A. Randomized controlled trials and psychotherapy research. Am J Psychiatry. 2007;164:7–8.
Sareen J, Cox BJ, Afifi TO, Stein MB, Belik S-L, Meadows G, et al. Combat and peacekeeping operations in relation to prevalence of mental disorders and perceived need for mental health care: findings from a large representative sample of military personnel. Arch Gen Psychiatry. 2007;64:843–52.
Berking M, Meier C, Wupperman P. Enhancing emotion-regulation skills in police officers: results of a pilot controlled study. Behav Ther. 2010;41:329–39.
Acknowledgements
The authors would like to acknowledge Dr. Vivien Lee, Dr. Don McCreary, and Dr. Dan Bilsker for their thoughtful reviews of the current manuscript. Helen Dragatsi helped to secure funding for this project. Paula M. Di Nota is now a post-doctoral fellow at the University of Toronto Mississauga.
Funding
This research is supported by funds from WorkSafeBC (RS2019-SP13 Anderson).
Author information
Authors and Affiliations
Contributions
All authors contributed to the conceptualization of this project. Dr. Bahji registered the review protocol with PROSPERO, conducted the literature review, and wrote the initial draft, coordinating revisions from the co-authors. Dr. Di Nota supported the literature review, serving as the second reviewer. Dr. Anderson secured funding. Drs. Groll and Carleton provided additional supervision, methodological support, and feedback throughout revisions. The author(s) read and approved the final manuscript.
Authors’ information
Dr. Groll is an Associate Professor of Psychiatry at Queen’s University and the Scientific Director at the Canadian Institutes of Military and Veteran Health Research. Dr. Carleton is a Professor of Psychology at the University of Regina. Finally, Dr. Anderson is the Dean of the Faculty of Science at Thompson Rivers University.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable (systematic review).
Consent for publication
Not applicable (systematic review).
Competing interests
Dr. Bahji is a recipient of the 2020 Friends of Matt Newell Endowment in Substance Abuse through the University of Calgary Cumming School of Medicine.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendices
Appendix 1
Search strategy
Appendix 2
Table 6
Appendix 3
Table 7
Appendix 4
Figure 5
Appendix 5
Figure 6
Funnel plots for publication bias in meta-analyses for the effectiveness of psychotherapies for A PTSD symptom severity after intervention and follow-up; B PTSD remission after the intervention and in follow-up; C anxiety symptom severity after intervention and follow-up; D depression symptom severity after the intervention and in follow-up; E retention in intervention at the primary trial endpoint and F retention in intervention at extended follow-up
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Bahji, A., Di Nota, P.M., Groll, D. et al. Psychological interventions for post-traumatic stress injuries among public safety personnel: a systematic review and meta-analysis. Syst Rev 11, 255 (2022). https://doi.org/10.1186/s13643-022-02112-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13643-022-02112-1