Abstract
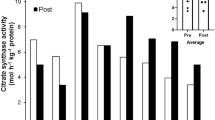
The most frequently reported symptom of exposure to high altitude is loss of body mass and decreased performance which has been attributed to altered protein metabolism affecting skeletal muscles mass. The present study explores the mechanism of chronic hypobaric hypoxia mediated skeletal muscle wasting by evaluating changes in protein turnover and various proteolytic pathways. Male Sprague–Dawley rats weighing about 200 g were exposed to hypobaric hypoxia (7,620 m) for different durations of exposure. Physical performance of rats was measured by treadmill running experiments. Protein synthesis, protein degradation rates were determined by 14C-Leucine incorporation and tyrosine release, respectively. Chymotrypsin-like enzyme activity of the ubiquitin–proteasome pathway and calpains were studied fluorimetrically as well as using western blots. Declined physical performance by more than 20%, in terms of time taken in exhaustion on treadmill, following chronic hypobaric hypoxia was observed. Compared to 1.5-fold increase in protein synthesis, the increase in protein degradation was much higher (five-folds), which consequently resulted in skeletal muscle mass loss. Myofibrillar protein level declined from 46.79 ± 1.49 mg/g tissue at sea level to 37.36 ± 1.153 (P < 0.05) at high altitude. However, the reduction in sarcoplasmic proteins was less as compared to myofibrillar protein. Upregulation of Ub-proteasome pathway (five-fold over control) and calpains (three-fold) has been found to be important factors for the enhanced protein degradation rate. The study provided strong evidences suggesting that elevated protein turnover rate lead to skeletal muscle atrophy under chronic hypobaric hypoxia via ubiquitin–proteasome pathway and calpains.








Similar content being viewed by others
References
Fulco CS, Friedlander AL, Muza SR, Rock PB, Robinson S, Lammi E, Baker R, Fulco CJ, Lewis SF, Cymerman A (2002) Energy intake deficit and physical performance at altitude. Aviat Space Environ Med 73:758–765
Bharadwaj H, Prasad J, Pramanik SN, Kishnani S, Zachariah T, Chaudhary KL, Sridharan K, Srivastava KK (2000) Effect of prolonged exposure to high altitude on skeletal muscles of Indian soldiers. Def Sci J 50:167–176
Macdonald JH, Oliver SJ, Hillyer K, Sanders S, Smith Z, Williams C, Yates D, Ginnever H, Scanlon E, Roberts E, Murphy D, Lawley J, Chichester E (2009) Body composition at high altitude: a randomized placebo-controlled trial of dietary carbohydrate supplementation. Am J Clin Nutr 90:1193–1202
Sridharan K, Mukherjee AK, Grover SK, Kumaria MML, Arora BS, Rai RM (1987) Assessment of nutritional status and physical work capacity of road construction workers at altitude of 2150–2750 m on two different ration scales. Nutr Rep Int 35:1269–1277
Brouns F (1992) Nutritional aspects of health and performance at lowland and altitude. Int J Sports Med 13:S100–S106
Schols AM (2002) Pulmonary cachexia. Int J Cardiol 85:101–110
Hoppeler H, Vogt M (2001) Muscle tissue adaptations to hypoxia. J Exp Biol 204:3133–3139
Hoppeler H, Kleinert E, Schlegel C, Claassen H, Howald H, Kayar SR, Cerretelli P (1990) Muscular exercise at high altitude. II. Morphological adaptation of skeletal muscle to chronic hypoxia. Int J Sports Med 11:S3–S9
Martinelli M, Winterhalder R, Cerretelli P, Howald H, Hoppeler H (1990) Muscle lipofuscin content and satellite cell volume is increased after high altitude exposure in humans. Experientia 46:672–676
Kung-tung C, Yu-yawn C, Huey-june W, Chen-kang C, Wen-tsung L, Yen-yuan L, Chieh-chung L, Rong-sen Y, Jung-charng L (2008) Decreased anaerobic performance and hormone adaptation after expedition to Peak Lenin. Chin Med J 121:2229–2233
Bigard AX, Douce P, Merino D, Lienhard F, Guezennec CY (1996) Changes in dietary protein intake fail to prevent decrease in muscle growth induced by severe hypoxia in rats. J Appl Physiol 80:208–215
Preedy VR, Smith DM, Sugden PH (1985) The effects of 6 hr hypoxia on protein synthesis in rat tissue in vivo & in vitro. Biochem J 228:179–185
Preedy VR, Sugden PH (1989) The effects of fasting or hypoxia on rates of protein synthesis in vivo in subcellular fractions of rat heart and gastrocnemius muscle. Biochem J 257:519–527
Iioka TK, Sugito K, Moriya T, Kuriyama T (2002) Effects of insulin like growth factor on nitrogen balance during hypoxic exposure. Eur Respir J 20:293–299
Vigano A, Ripamonti M, Palma SD, Capitanio D, Vasso M, Wait R, Lundby C, Cerretelli P, Gelfi C (2008) Proteins modulation in human skeletal muscle in the early phase of adaptation to hypobaric hypoxia. Proteomics 8:4668–4679
Imoberdorf R, Garlick PJ, McNurlan MA, Casella GA, Marini JC, Turgay M, Bartsch P, Ballmer PE (2006) Skeletal muscle protein synthesis after active or passive ascent to high altitude. Med Sci Sports Exerc 38:1082–1087
Holm L, Haslund ML, Robach P, van Hall G, Calbet JA, Saltin B, Lundby C (2010) Skeletal muscle myofibrillar and sarcoplasmic protein synthesis rates are affected differently by altitude-induced hypoxia in native lowlanders. PLoS ONE 20:e15606
Rennie MJ (1985) Muscle protein turnover and the wasting due to injury and disease. Br Med Bull 41:257–264
Cai D, Lee KK, Li M, Tang MK, Chan KM (2004) Ubiquitin expression is upregulated in human and rat skeletal muscles during aging. Arch Biochem Biophys 425:42–50
Reid MB (2005) Response of the ubiquitin–proteasome pathway to changes in muscle activity. Am J Physiol Regul Integr Comp Physiol 288:R1423–R1431
Mammucari C, Milan G, Romanello V, Masiero E, Rudolf R, Piccolo PD, Burden SJ, Lisi RD, Sandri C, Zhao J, Goldberg AL, Schiaffino S, Sandri M (2007) FoxO3 controls autophagy in skeletal muscle in vivo. Cell Metab 6:458–471
Attaix D, Mosoni L, Dardevet D, Combaret L, Mirand PP, Grizard J (2005) Altered responses in skeletal muscle protein turnover during aging in anabolic and catabolic periods. Int J Biochem Cell Biol 37:2098–2114
Enns DL, Raastad T, Ugelstad I, Belcastro AN (2007) Calpain/calpastatin activities and substrate depletion patterns during hindlimb unweighting and reweighting in skeletal muscle. Eur J Appl Physiol 100:445–455
Dardevet D, Sornet C, Vary T, Grizard J (1996) Phosphotidylinositol 3-kinase and p70 S6 kinase participate in the regulation of protein turnover in skeletal muscle by insulin and insulin-like growth factor I. Endocrinology 137:4089–4094
Vary TC, Dardevet D, Grizard J, Voisin L, Buffiere C, Denis P, Breuille D, Obled C (1998) Differential regulation of skeletal muscle protein turnover by insulin and IGF-1 after bacteremia. Am J Physiol Endocrinol Metab 275:E584–E593
Ventrucci G, Mello MAR, Marcondes G (2004) Proteasome activity is altered in skeletal muscle tissue of tumour-bearing rats fed a leucine-rich diet. Endocr Relat Cancer 11:887–895
Waalkes TP, Udenfriend S (1957) A fluorimetric method for the estimation of tyrosine in plasma and tissues. J Lab Clin Med 50:733–736
Hepple RT, Qin M, Nakamoto H, Goto S (2008) Caloric restriction optimizes the proteasome activity. Am J Physiol Regul Integr Comp Physiol 295:R1231–R1237
Mastrocola R, Reffo P, Penna F, Tomasinelli CE, Boccuzzi G, Baccino FM, Aragno M, Costelli P (2008) Muscle wasting in diabetic and in tumor bearing rats: role of oxidative stress. Free Radic Biol Med 44:584–593
Oron U (1990) Proteolytic enzyme activity in rat hind limb muscle in fetus and during post natal development. Int J Dev Biol 34:457–460
Lowry OH, Rosebrough NJ, Farr AL, Randall RJ (1951) Protein measurement with the folin phenol reagent. J Biol Chem 193:265–275
Koopman R, Gehrig SM, Leger B, Walrand S, Murphy KT, Lynch GS (2010) Cellular mechanisms underlying temporal changes in skeletal muscle protein synthesis and breakdown during chronic β-adrenoceptor stimulation in mice. J Physiol 588:4811–4823
Kvamme E, Torgner IA, Svenneby G (1985) Glutaminase from mammalian tissue. Methods Enzymol 113:241–244
Elliott WH (1955) Glutamine synthesis. In: Colowick SP, Kaplan NO (eds) Methods enzymol II. pp 337–339
Cathcart R, Schwiers E, Ames BN (1983) Detection of pico mole levels of hyderoperoxides using fluorescent dichlorofluoroscein assay. Anal Biochem 134:111–116
Buege JA, Aust SD (1978) Microsomal lipid peroxidation. Methods Enzymol 52:302–310
Dutta A, Ray K, Singh VK, Vats P, Singh SN, Singh SB (2008) L-carnitine supplementation attenuates intermittent hypoxia-induced oxidative stress and delays muscle fatigue in rats. Exp Physiol 93:1139–1146
Tisdale MJ (2005) The Ub-proteasome pathway as a therapeutic target for muscle wasting. J Support Oncol 3:209–217
Howald H, Pette D, Simoneau JA, Uber A, Hoppeler H, Cerretelli P (1990) Effect of chronic hypoxia on muscle enzyme activities. Int J Sports Med S10–S14
Vats P, Mukherjee AK, Kumria MM, Singh SN, Patil SK, Rangnathan S, Sridharan K (1999) Changes in activity levels of glutamine synthetase, glutaminase and glycogen synthetase in rats subjected to hypoxic stress. Int J Biometeorol 42:205–209
Shang F, Gong Taylor A (1997) Activity of ubiquitin-dependent pathway in response to oxidative stress. Ubiquitin-activating enzyme is transiently up-regulated. J Biol Chem 272:23086–23093
Fernandes R, Ramalho J, Pereira P (2006) Oxidative stress upregulates ubiquitin proteasome pathway in retinal endothelial cells. Mol Vis 12:1526–1535
Hermann J, Gulati R, Napoli C, Woodrum LLO, Porcel MR, Sica V, Simari RD, Ciechanover A, Lerman A (2003) Oxidative stress-related increase in ubiquitination in early coronary atherogenesis. FASEB 17:1730–1732
Gomes M, Maria CC, Tisdale MJ (2002) Induction of protein catabolism and the ubiquitin proteasome pathway by mild oxidative stress. Cancer Lett 180:69–74
Sagi SKS, Patir H, Mishra C, Pradhan G, Mastoori SR, Ilavazhagan G (2008) Role of oxidative stress and NFkB in hypoxia induced pulmonary edema. Exp Biol Med 233:1088–1098
Marfella R, Amico MD, Filippo CD, Baldi A, Siniscalchi M, Sasso FC, Portoghese M, Carbonara O, Crescenzi B, Sangiuolo P, Nicoletti GF, Rossiello R, Ferraraccio F, Cacciapuoti F, Verza M, Coppola L, Rossi F, Paolisso G (2006) Increased activity of the ubiquitin-proteasome system in patients with symptomatic carotid disease is associated with enhanced inflammation and may destabilize the atherosclerotic plaque: effects of rosiglitazone treatment. JACC 47:2444–2455
Acknowledgments
This study was supported and funded by the Defence Research and Development organization, Ministry of Defence, Government of India. The authors are grateful to the Director, Defence Institute of Physiology and Allied Sciences, Delhi for providing facilities to carry out these investigations.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Chaudhary, P., Suryakumar, G., Prasad, R. et al. Chronic hypobaric hypoxia mediated skeletal muscle atrophy: role of ubiquitin–proteasome pathway and calpains. Mol Cell Biochem 364, 101–113 (2012). https://doi.org/10.1007/s11010-011-1210-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11010-011-1210-x