Abstract
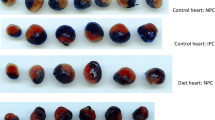
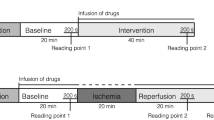
The mechanisms of the adverse effects of free fatty acids on the ischemic-reperfused myocardium are not fully understood. Long-chain fatty acids, including palmitate, uncouple oxidative phosphorylation and should therefore promote the formation of oxygen-derived free radicals, with consequent adverse effects. Conversely, the antianginal agent trimetazidine (TMZ), known to inhibit cardiac fatty acid oxidation, could hypothetically lessen the formation of reactive oxygen species (ROS) and thus improve reperfusion mechanical function. Isolated perfused rat hearts underwent 30 min of total global ischemia followed by 30 min of reperfusion. Hearts were perfused with glucose 5.5 mmol/l or palmitate 1.5 mmol/l with or without TMZ (100 μmol/l). Ascorbyl free radical (AFR) release during perfusion periods was measured by electron spin resonance as a marker of oxidative stress. Post-ischemic recovery in the palmitate group of heart was lower than in the glucose group with a marked rise in diastolic tension and reduction in left ventricular developed pressure (Glucose: 85 ± 11 mmHg; Palmitate: 10 ± 6 mmHg; p < 0.001). TMZ decreased diastolic tension in both glucose- and in palmitate-perfused hearts. Release of AFR within the first minute of reperfusion was greater in palmitate-perfused hearts and in hearts perfused with either substrate, this marker of oxidative stress was decreased by TMZ (expressed in arbitrary units/ml; respectively: 8.49 ± 1.24 vs. 1.06 ± 0.70 p < 0.05; 12.47 ± 2.49 vs. 3.37 ± 1.29 p < 0.05). Palmitate increased the formation of ROS and reperfusion contracture. TMZ, a potential inhibitor of palmitate-induced mitochondrial uncoupling, decreased the formation of free radicals and improved postischemic mechanical dysfunction. The novel conclusion is that adverse effects of fatty acids on ischemic-reperfusion injury may be mediated, at least in part, by oxygen-derived free radicals.
Similar content being viewed by others
References
Bing RJ, Siegel A, Ungar I, Gilbert M: Metabolism of the human heart II. Studies on fat, ketone and amino acid metabolism. Am J Med 16: 504–515, 1954
Opie LH, Evans JR, Shipp JC: Effect of fasting on glucose and palmitate metabolism of perfused rat heart. Am J Physiol 205: 1203–1208, 1963
De Leiris J, Opie LH, Lubbe WF: Effects of free fatty acid and enzyme release in experimental glucose on myocardial infarction. Nature 253: 746–747, 1975
Opie LH: Effect of fatty acids on contractility and rhythm of the heart. Nature 227: 1055–1056, 1970
Ferrari R: Factors influencing the metabolic and functional alterations induced by ischemia and reperfusion. In: R. Ferrari et al. (eds). Myocardial Ischemia and Lipid Metabolism. Plenum Press, New York, 1983, pp 135–137
Oliver MF, Kurien VA, Greenwood TW: Relation between serum-free-fatty acids and arrhythmias and death after acute myocardial infarction. Lancet 1(7545): 710–714, 1968
Lopaschuk GD, Wambolt RB, Barr RL: An imbalance between glycolysis and glucose oxidation is a possible explanation for the detrimental effects of high levels of fatty acids during aerobic reperfusion of ischemic hearts. J Pharmacol Exp Ther 264: 135–144, 1993
Maupoil V, Rochette L: Evaluation of free radical and lipid peroxide formation during global ischemia and reperfusion in isolated perfused rat heart. Cardiovasc Drugs Ther 2: 615–621, 1988
Bolli R: Oxygen-derived free radicals and myocardial reperfusion injury: an overview. Cardiovasc Drugs Ther 5: 249–268, 1991
Bernier M, Hearse DJ, Manning AS: Reperfusion-induced arrhythmias and oxygen-derived free radicals. Studies with “anti-free radical” interventions and a free radical-generating system in the isolated perfused rat heart. Circ Res 58: 331–340, 1986
Vergely C, Maupoil V, Benderitter M, Rochette L: Influence of the severity of myocardial ischemia on the intensity of ascorbyl free radical release and on postischemic recovery during reperfusion. Free Radic Biol Med 24: 470–479, 1998
Cantor PF, Lucien A, Kozak R, Lopaschuk, GD: The antianginal drug trimetazidine shifts cardiac energy metabolism from fatty acid oxidation to glucose oxidation by inhibiting mitochondrial long-chain 3-ketoacyl coenzyme A thiolase. Circ Res 86: 580–588, 2000
Monteiro P, Duarte Al, Goncalves LM, Moreno A, Providencia LA: Protective effect of trimetazidine on myocardial mitochondrial function in an ex-vivo model of global myocardial ischemia. Eur J Pharmacol 503: 123–128, 2004
Watts JA, Maiorano PC: Trace amounts of albumin protect against ischemia and reperfusion injury in isolated rat hearts. J Mol Cell Cardiol 31: 1653–1662, 1999
Buettner GR, Jurkiewicz BA: Ascorbate free radical as a marker of oxidative stress: an EPR study. Free Radic Biol Med 14: 49–55, 1993
Lesnefsky EJ, Chen Q, Moghaddas S, Hassan MO, Tandler B, Hoppel CL: Blockade of electron transport during ischemia protects cardiac mitochondria. J Biol Chem 279: 47961–47967, 2004
Lopaschuk GD, Barr R, Thomas PD, Dyck JR: Beneficial effects of trimetazidine in ex vivo working ischemic hearts are due to a stimulation of glucose oxidation secondary to inhibition of long-chain 3-ketoacyl coenzyme a thiolase. Circ Res 93: 26–32, 2003
Pantos C, Bescond-Jacquet A, Tzeis S, Paizis I, Mourouzis I, Moraitis P, Malliopoulou V, Politi ED, Karageorgiou H, Varonos D, Cokkinos DV: TMZ protects isolated rat hearts against ischemia-reperfusion injury in an experimental timing – dependent manner. Basic Res Cardiol 100: 154–160, 2005
Tritto I, Wang P, Kuppusamy P, Giraldez R, Zweier JL, Ambrosio G: The anti-anginal drug trimetazidine reduces neutrophil-mediated cardiac reperfusion injury. J Cardiovasc Pharmacol 46: 89–98, 2005
Maupoil V, Rochette L, Tabard A, Clauser P, Harpey C: Direct measurement of free radical generation in isolated rat heart by electron paramagnetic resonance spectroscopy: effect of trimetazidine. Adv Exp Med Biol 264: 373–376, 1990
Guarnieri C, Muscari C: Anti oxy-radical properties of trimetazidine. Res Commun Chem Pathol Pharmacol 64: 215–225, 1989
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Gambert, S., Vergely, C., Filomenko, R. et al. Adverse effects of free fatty acid associated with increased oxidative stress in postischemic isolated rat hearts. Mol Cell Biochem 283, 147–152 (2006). https://doi.org/10.1007/s11010-006-2518-9
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1007/s11010-006-2518-9