Abstract
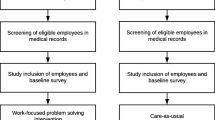
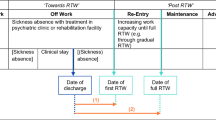
Purpose Common mental disorders (CMDs) are a major cause of sick leave. Return-to-work (RTW) interventions providing mechanisms that support the participation and collaboration of the different stakeholders appear promising in these circumstances. The Therapeutic Return-to-Work (TRW) Program offers such mechanisms designed to enable affected workers to fully reintegrate into their jobs on a sustainable basis. This study evaluated the feasibility of implementing this program for workers with CMDs, within a specialized mental health hospital. Methods The study was conducted using a multiple case design and three main data sources: (1) the worker’s medical file, (2) the log completed by the clinicians, and (3) individual interviews with stakeholders. Data were analyzed using a qualitative approach. Results Twelve workers between 32 and 60 years old, mostly women with complex mental health profiles working in large enterprises, participated in this study. Three main observations were made regarding the TRW Program implementation: (1) eight cases were characterized by complete or virtually complete implementation; (2) no explanatory factor could be identified for the different implementation levels; (3) eight cases achieved RTW success (RTW to the original job or another job), which appears partially attributable to the high level of program implementation. Conclusions: The TRW Program seems highly promising for supporting the return to work of workers with CMDs. However, studies identifying the factors likely to influence the implementation process in different health service contexts and specifying the scope and nature of the program’s actual impact on RTW outcomes should be conducted before larger-scale implementation takes place.


Similar content being viewed by others
References
Mental Health Commission of Canada. Supporting workplace mental health. Ottawa: Health Canada; 2016.
Dewa, CS., McDaid, D., Sultan-Taïeb, H. (2011) Epidemiological and economic aspects inherent in mental disorders (Aspects épidémiologiques et économiques inhérents aux troubles mentaux.) In: Corbière, M., Durand, MJ., editors. From mental disorder to incapacity at work: A transdisciplinary perspective that aims to better understand this problem and to offer avenues for intervention (Du Trouble Mental à l’Incapacité au Travail: Une perspective transdisciplinaire qui vise à mieux saisir cette problématique et à offrir des pistes d’intervention.), QC: Presses de l’Université du Québec, Québec (PUQ) 5–40
Mental Health Commission of Canada - MHCC. (2017) Reducing employment barriers for people living with a mental illness: Using evidence-based practices to build Canada’s mental health and employment policy framework (Réduction des obstacles à l’emploi pour les personnes ayant un problème de santé mentale: Recours à des pratiques fondées sur des données probantes pour établir le cadre stratégique canadien sur la santé mentale et l’emploi.) MHCC, Ottawa
Sairanen S, Matzanke D, Smeall D. The business case: collaborating to help employees maintain their mental well-being. Healthc Pap. 2011;11:78–84.
Roelen CAM, Norder G, Koopmans PC, et al. Employees sick-listed with mental disorders: who returns to work and when? J Occup Rehabil. 2012;22:409–17.
Zaidel CS, Ethiraj RK, Berenji M, Gaspar FW. Health care expenditures and length of disability across medical conditions. J Occup Environ Med. 2018;60:631–6.
James SL, Abate D, Abate KH, et al. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. The Lancet. 2018;392:1789–858.
World Health Organization. (2017) Depression and other common mental disorders: global health estimates. https://apps.who.int/iris/handle/10665/254610. Accessed 1 July 2020.
Borg V, Andersen MN, Kolte IV, Andersen MF. White paper on mental health, sickness absence and return to work. Copenhagen: National Research Centre for the Working Environment; 2010.
Canada Safety Council. (2018) Mental Health and the Workplace. In: Canada Safety Council. https://canadasafetycouncil.org/mental-health-and-the-workplace. Accessed 25 July 2018
Dewa CS, Chau N, Dermer S. Examining the comparative incidence and costs of physical and mental health-related disabilities in an employed population. J Occup Environ Med. 2010;52:758–62.
Dewa CS, Chau N, Dermer S. Factors associated with short-term disability episodes. J Occup Environ Med. 2009;51:1394–402.
Dewa CS, McDaid D, Ettner SL. An International perspective on worker mental health problems: who bears the burden and how are costs addressed? Can J Psychiatry. 2007;52:346–56.
Fossey EM, Harvey CA. Finding and sustaining employment: A qualitative meta-synthesis of mental health consumer views. Can J Occup Ther. 2010;77:303–14.
Lim D, Sanderson K, Andrews G. Lost productivity among full-time workers with mental disorders. J Ment Health Policy Econ. 2000;3:139–46.
Mental Health Commission of Canada. Making the case for investing in mental health in Canada. Ottawa: Health Canada; 2013.
OECD. Sick on the Job? Myths and Realities about Mental Health and Work. Paris: OECD Publishing; 2012.
Grazier KL. The Economic Impact of Depression in the Workplace. In: Riba MB, Parikh SV, Greden JF, editors. Mental health in the workplace: strategies and tools to optimize outcomes. Cham: Springer International Publishing; 2019. p. 17–26.
Kinman G. Sickness presenteeism at work: prevalence, costs and management. Br Med Bull. 2019;129:69–78.
Greenberg PE, Fournier AA, Sisitsky T, et al. The economic burden of adults with major depressive disorder in the United States (2005 and 2010). J Clin Psychiatry. 2015;76:155–62.
Stewart WF, Ricci JA, Chee E, et al. Cost of lost productive work time among US workers with depression. JAMA. 2003;289:3135–44.
Tomonaga Y, Haettenschwiler J, Hatzinger M, et al. The economic burden of depression in Switzerland. Pharmacoeconomics. 2013;31:237–50.
Lim KL, Jacobs P, Ohinmaa A, et al. A new population-based measure of the economic burden of mental illness in Canada. Chronic Dis Can. 2008;28:92–8.
Cullen KL, Irvin E, Collie A, et al. Effectiveness of workplace interventions in return-to-work for musculoskeletal, pain-related and mental health conditions: an update of the evidence and messages for practitioners. J Occup Rehabil. 2018;28:1–15.
Martin MHT, Nielsen MBD, Petersen SMA, et al. Implementation of a coordinated and tailored return-to-work intervention for employees with mental health problems. J Occup Rehabil. 2012;22:427–36.
Sylvain C, Durand MJ, Sanchez AV, et al. Development and Implementation of a Mental Health Work Rehabilitation Program: Results of a Developmental Evaluation. J Occup Rehabil. 2019;29:303–14.
Andersen MF, Nielsen KM, Brinkmann S. Meta-synthesis of qualitative research on return to work among employees with common mental disorders. Scand J Work Environ Health. 2012;38:93–104.
Nielsen MBD, Bültmann U, Amby M, et al. Return to work among employees with common mental disorders: Study design and baseline findings from a mixed-method follow-up study. Scand J Soc Med. 2010;38:864–72.
Wisenthal A, Krupa T, Kirshm BH, Lysaght R. Cognitive work hardening for return to work following depression: An intervention study. Can J Occup Ther. 2018;85:21–32.
Blonk RWB, Brenninkmeijer V, Lagerveld SE, Houtman ILD. Return to work: a comparison of two cognitive behavioural interventions in cases of work-related psychological complaints among the self-employed. Work Stress. 2006;20:129–44.
Martin MHT, Nielsen MBD, Madsen IEH, et al. Effectiveness of a coordinated and tailored return-to-work intervention for sickness absence beneficiaries with mental health problems. J Occup Rehabil. 2013;23:621–30.
Thisted CN, Nielsen CV, Bjerrum M. Work participation among employees with common mental disorders: a meta-synthesis. J Occup Rehabil. 2018;28(3):452–64.
Dewa CS, Trojanowski L, Joosen MCW, Bonato S. Employer best practice guidelines for the return to work of workers on mental disorder-related disability leave: a systematic review. Can J Psychiatry Rev Can Psychiatr. 2016;61:176–85.
Loisel P, Durand MJ, Berthelette D, et al. Disability prevention: new paradigm for the management of occupational back pain. Dis Manag Health Outcomes. 2001;9:351–60.
Durand, MJ., Loisel, P., Charpentier, N. et al. The Therapeutic Return to Work (RTT) program. An evidence-based occupational rehabilitation program (Le programme de Retour Thérapeutique au Travail (RTT). Un programme de réadaptation au travail basé sur les données probantes.) Boucherville: PREVICAP occupational rehabilitation clinical research center (Centre de recherche clinique en réadaptation au travail PRÉVICAP); 2004.
Loisel P, Anema J, editors. Handbook of Work Disability: Prevention and Management. New York: Springer-Verlag; 2013.
Durand, MJ., Briand, C. (2011) Return-to-work interventions/programs for workers with transient mental disorders (Interventions/programmes de retour au travail destinés aux travailleurs ayant un trouble mental transitoire). In: Corbière M, Durand M-J, (eds) From mental disorder to work disability: A transdisciplinary perspective which aims to better understand this problem and to offer avenues for intervention (Du trouble mental à l’incapacité au travail: Une perspective transdisciplinaire qui vise à mieux saisir cette problématique et à offrir des pistes d’interventions). Presses de l’Université du Québec (PUQ), Québec (pp. 199-224)
Durand MJ, Loisel P. Therapeutic Return to Work: Rehabilitation in the workplace. Work Read Mass. 2001;17:57–63.
Durand MJ, Loisel P. (2001) The transformation of occupational rehabilitation from a compartmentalized perspective to a systemic perspective (La transformation de la réadaptation au travail d’une perspective parcellaire à une perspective systémique). Interdisciplinary perspectives on work and health (Perspectives interdisciplinaires sur le travail et la santé) [Internet]. https://doi.org/10.4000/pistes.3799.
Durand MJ, Vachon B, Loisel P, Berthelette D. Constructing the program impact theory for an evidence-based work rehabilitation program for workers with low back pain. Work Read Mass. 2003;21:233–42.
Durand MJ, Berthelette D, Loisel P, Imbeau D. Validation of the programme impact theory for a work rehabilitation programme. Work Read Mass. 2012;42:495–505.
Loisel P, Lemaire J, Poitras S, et al. Cost-benefit and cost-effectiveness analysis of a disability prevention model for back pain management: a six year follow up study. Occup Environ Med. 2002;59:807–15.
Loisel P, Abenhaim L, Durand P, et al. A population-based, randomized clinical trial on back pain management. Spine. 1997;22:2911–8.
Briand C, Durand MJ, St-Arnaud L, Corbière M. Work and mental health: learning from return-to-work rehabilitation programs designed for workers with musculoskeletal disorders. Int J Law Psychiatry. 2007;30:444–57.
Pineault, R., Daveluy, C. (1995) Health planning: concepts, methods, strategies (La planification de la santé: concepts, méthodes, stratégies). Editions Nouvelles p. 480
Bowen DJ, Kreuter M, Spring B, et al. How we design feasibility studies. Am J Prev Med. 2009;36:452–7.
Yin RK. Case study research: design and methods. 4th ed. Los Angeles: Sage Publications; 2009.
Durand, MJ., Corbière, M., Briand, C. et al. (2011) Factors related to prolonged absences from work due to a transient mental disorder: development of a measurement tool (Les facteurs reliés aux absences prolongées du travail en raison d’un trouble mental transitoire: développement d’un outil de mesure). Montreal: Robert-Sauvé Research Institute in Occupational Health and Safety (Institut de recherche Robert-Sauvé en santé et en sécurité du travail)
Durand MJ, Coutu MF, Berbiche D. Validation of the work disability diagnosis interview for musculoskeletal and mental disorders. J Occup Rehabil. 2021;31:232–42.
American Psychiatric Association. (2022) Diagnostic and Statistical Manual of Mental Disorders: DSM-IV. American Psychiatric Association
Patton, MQ. (2015) Enhancing the Quality and Credibility of Qualitative Study. In: Qualitative Research & Evaluation Methods. 4th ed. Sage Publications, Thousand Oaks (pp. 652‑743)
Miles MB, Huberman AM. Qualitative data analysis (Analyse des données qualitatives). Louvain-la-Neuve: De Boeck Supérieur; 2003.
Vézina, M., Cloutier, E., Stock, SR. et al. (2011) Quebec survey on working and employment conditions and occupational health and safety (Enquête québécoise sur des conditions de travail, d’emploi et de santé et de sécurité du travail (EQCOTESST). Quebec, QC: Robert-Sauvé Research Institute in Occupational Health and Safety (Institut de recherche Robert-Sauvé en santé et sécurité du travail), Quebec National Institute of Public Health (Institut national de santé publique du Québec), Quebec Institute of Statistics (Institut de la statistique du Québec)
Pfadenhauer LM, Gerhardus A, Mozygemba K, et al. Making sense of complexity in context and implementation: the context and implementation of complex interventions (CICI) framework. Implement Sci. 2017;12:1–17.
Powell BJ, McMillen JC, Proctor EK, et al. A compilation of strategies for implementing clinical innovations in health and mental health. Med Care Res Rev. 2012;69:123–57.
Joosen MC, Lugtenberg M, Arends I, et al. Barriers and facilitators for return to work from the perspective of workers with common mental disorders with short, medium and long-term sickness absence: a longitudinal qualitative study. J Occup Rehabil. 2022;32:272–83.
de Vries G, Schene AH. Reintegration to Work of People Suffering from Depression. In: Söderback I, editor. International handbook of occupational therapy interventions. New York: Springer; 2009. p. 375–82.
Mikkelsen MB, Rosholm M. Systematic review and meta-analysis of interventions aimed at enhancing return to work for sick-listed workers with common mental disorders, stress-related disorders, somatoform disorders and personality disorders. Occup Environ Med. 2018;75:675–86.
Dol M, Varatharajan S, Neiterman E, et al. Systematic review of the impact on return to work of return-to-work coordinators. J Occup Rehabil. 2021;31:675–98.
Parsons V, Juszczyk D, Gilworth GA, et al. case management occupational health model to facilitate earlier return to work of NHS staff with common mental health disorders: a feasibility study. Health Technol Assess. 2021. https://doi.org/10.3310/hta25120.
Mayne J. Useful theory of change models. Can J Program Eval. 2015;30:119–42.
Brousselle A, Buregeya JM. Theory-based evaluations: Framing the existence of a new theory in evaluation and the rise of the 5th generation. Evaluation. 2018;24:153–68.
Lemire ST, Nielsen SB, Dybdal L. Making contribution analysis work: a practical framework for handling influencing factors and alternative explanations. Evaluation. 2012;18:294–309.
Shenton AK. Strategies for ensuring trustworthiness in qualitative research projects. Educ Inf. 2004;22:63–75.
Acknowledgements
We are grateful for the contribution of all the occupational health professionals, as well as the workers’, employers’ and insurers’ representatives who participated in this study.
Funding
This study was funded by the Research Chair in Occupational Rehabilitation (JA Bombardier/Pratt & Whitney Canada).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None of the authors have any conflicts of interest to declare.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Durand, MJ., Sylvain, C. & Paquette, MA. Return to Work for People with Common Mental Disorders: Insights into the Implementation of a Collaborative Program in a Specialized Mental Health Hospital. J Occup Rehabil 33, 362–374 (2023). https://doi.org/10.1007/s10926-022-10079-y
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10926-022-10079-y