Abstract
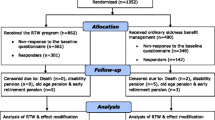
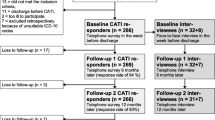
Purpose Sickness absence and exclusion from the labour market due to mental health problems (MHPs) is a growing concern in many countries. Knowledge about effective return-to-work (RTW) intervention models is still limited, but a multidisciplinary, coordinated and tailored approach has shown promising results in the context of musculoskeletal disorders. The purpose of this study was to assess the effectiveness of this approach as implemented among sickness absence beneficiaries with MHPs. Methods In a quasi-randomised, controlled trial, we assessed the intervention’s effect in terms of time to RTW and labour market status after 1 year. We used two different analytical strategies to compare time to RTW between participants receiving the intervention (n = 88) and those receiving conventional case management (n = 80): (1) a traditional multivariable regression analysis controlling for measured confounding, and (2) an instrumental variable (IV) analysis controlling for unmeasured confounding. Results The two analytical approaches provided similar results in terms of a longer time to RTW among recipients of the intervention (HR = 0.50; 95 % CI 0.34–0.75), although the estimate provided by the IV-analysis was non-significant (HR = 0.70; 95 % CI 0.23–2.12). After 1 year, more recipients of the intervention than of conventional case management were receiving sickness absence benefits (p = 0.031). Conclusion The intervention delayed RTW compared to conventional case management, after accounting for measured confounding. The delayed RTW may be due to either implementation or program failure, or both. It may also reflect the complexity of retaining employees with mental health problems in the workplace.


Similar content being viewed by others
References
OECD. Sickness, disability and work: breaking the barriers. A synthesis of findings across OECD countries. Paris: OECD Publishing; 2010.
van der Klink JJL, Blonk RWB, Schene AH, van Dijk FJH. Reducing long term sickness absence by an activating intervention in adjustment disorders: a cluster randomised controlled design. Occup Environ Med. 2003;60:429–37.
Brouwers EPM, Tiemens BG, Terluin B, Verhaak PFM. Effectiveness of an intervention to reduce sickness absence in patients with emotional distress or minor mental disorders: a randomized controlled effectiveness trial. Gen Hosp Psychiatry. 2006;28:223–9.
de Vente W, Kamphuis JH, Ernmelkamp PMG, Blonk RWB. Individual and group cognitive-behavioral treatment for work-related stress complaints and sickness absence: a randomized controlled trial. J Occup Health Psychol. 2008;13:214–31.
Willert MV, Thulstrup AM, Bonde JP. Effects of a stress management intervention on absenteeism and return to work—results from a randomized wait-list controlled trial. Scand J Work Env Health. 2011;37:186–95.
van Oostrom SH, van Mechelen W, Terluin B, de Vet HC, Knol DL, Anema JR. A workplace intervention for sick-listed employees with distress: results of a randomised controlled trial. Occup Environ Med. 2010;67:596–602.
Fleten N, Johnsen R. Reducing sick leave by minimal postal intervention: a randomised, controlled intervention study. Occup Environ Med. 2006;63:676–82.
Netterstrøm B, Bech P. Effect of a multidisciplinary stress treatment programme on the return to work rate for persons with work-related stress. A non-randomized controlled study from a stress clinic. BMC Public Health. 2010;10:658.
Søgaard HJ, Bech P. The effect on length of sickness absence by recognition of undetected psychiatric disorder in long-term sickness absence. A randomized controlled trial. Scand J Public Health. 2009;37:864–71.
Nieuwenhuijsen K, Bültmann U, Neumeyer-Gromen A, Verhoeven AC, Verbeek JH, van der Feltz-Cornelis CM. Interventions to improve occupational health in depressed people. Cochr Database System Rev. 2008;2:CD006237.
Borg V, Nexø M, Kolte I, Andersen M. Hvidbog om mentalt helbred, sygefravær og tilbagevenden til arbejde [White paper on mental health, sickness absence and return to work] [Danish]. Copenhagen: The National Research Centre for the Working Environment; 2010.
Bültmann U, Sherson D, Olsen J, Hansen CL, Lund T, Kilsgaard J. Coordinated and tailored work rehabilitation: a randomized controlled trial with economic evaluation undertaken with workers on sick leave due to musculoskeletal disorders. J Occup Rehabil. 2009;19:81–93.
Bonell CP, Hargreaves J, Cousens S, Ross D, Hayes R, Petticrew M, et al. Alternatives to randomisation in the evaluation of public health interventions: design challenges and solutions. J Epidemiol Community Health. 2011;65:582–7.
Earle CC, Tsai JS, Gelber RD, Weinstein MC, Neumann PJ, Weeks JC. Effectiveness of chemotherapy for advanced lung cancer in the elderly: instrumental variable and propensity analysis. J Clin Oncol. 2001;19:1064–70.
Martens EP, Pestman WR, de Boer A, Belitser SV, Klungel OH. Instrumental variables application and limitations. Epidemiology. 2006;17:260–7.
Loisel P, Durand MJ, Diallo B, Vachon B, Charpentier N, Labelle J. From evidence to community practice in work rehabilitation: the Quebec experience. Clin J Pain. 2003;19:105–13.
Nielsen MBD, Bultmann U, Madsen IEH, Martin MHT, Christensen U, Diderichsen F, et al. Health, work, and personal-related predictors of time to return to work among employees with mental health problems. Disabil Rehabil. 2012;34:1311–6.
Hernan MA, Robins JM. Instruments for causal inference: an epidemiologist’s dream? Epidemiology. 2006;17:360–72.
Angrist JD, Imbens GW, Rubin DB. Identification of causal effects using instrumental variables. JASA. 1996;91:444–55.
Cousens S, Hargreaves J, Bonell C, Armstrong B, Thomas J, Kirkwood BR, et al. Alternatives to randomisation in the evaluation of public-health interventions: statistical analysis and causal inference. J Epidemiol Community Health. 2011;65:576–81.
Cole JA, Norman H, Weatherby LB, Walker AM. Drug copayment and adherence in chronic heart failure: effect on cost and outcomes. Pharmacotherapy. 2006;26:1157–64.
Brookhart MA, Rassen JA, Schneeweiss S. Instrumental variable methods in comparative safety and effectiveness research. Pharmacoepidemiol Drug Saf. 2010;19:537–54.
Martin MHT, Nielsen MBD, Petersen SMA, Jakobsen LM, Rugulies R. Implementation of a coordinated and tailored return-to-work intervention for employees with mental health problems. J Occup Rehabil. 2012;22:427–36.
World Health Organization. International statistical classification of diseases and related health problems, 10th revision (ICD-10). Geneva: World Health Organization; 1992.
World Health Organization. International classification of functioning, disability and health (ICF). Geneva: World Health Organization; 2007.
Sekjær, K. Stadigt flere psykisk syge må vente på behandling [Increasing number of mentally ill must wait for treatment] [Danish]. Available from: http://www.information.dk/259442.
Pedersen J, Villadsen E, Burr H, Martin MHT, Nielsen MBD, Meinertz L. Register for sygedagpenge og sociale ydelser i Danmark [The Danish register of sickness absence compensation and social transfer payments] [Danish]. Copenhagen: The National Research Centre for the Working Environment; 2011.
Nielsen MBD, Madsen IEH, Bültmann U, Christensen U, Diderichsen F, Rugulies R. Predictors of return to work in employees sick-listed with mental health problems: findings from a longitudinal study. Eur J Public Health. 2011;21:806–11.
Sell L, Bültmann U, Rugulies R, Villadsen E, Faber A, Sogaard K. Predicting long-term sickness absence and early retirement pension from self-reported work ability. Int Arch Occ Env Health. 2009;82:1133–8.
Virtanen M, Kawachi I, Oksanen T, Salo P, Tuisku K, Pulkki-Raback L, et al. Socio-economic differences in long-term psychiatric work disability: prospective cohort study of onset, recovery and recurrence. Occup Environ Med. 2011;68:791–8.
Blank L, Peters J, Pickvance S, Wilford J, MacDonald E. A systematic review of the factors which predict return to work for people suffering episodes of poor mental health. J Occup Rehabil. 2008;18:27–34.
Rose D, Harrison E. The European socio-economic classification: a new social class schema for comparative European research. Eur Societies. 2007;9:459–90.
Ware JE Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30:473–83.
Bech P, Rasmussen NA, Olsen LR, Noerholm V, Abildgaard W. The sensitivity and specificity of the Major Depression Inventory, using the Present State Examination as the index of diagnostic validity. J Affect Dis. 2001;66:159–64.
Derogatis LR. SCL-90-R. Administration, scoring and procedures. MANUAL-II. Townson MD, 1983.
Durlak JA, DuPre EP. Implementation matters: a review of research on the influence of implementation on program outcomes and the factors affecting implementation. Am J Community Psychol. 2008;41:327–50.
Rebergen DS, Bruinvels DJ, Bos CM, van der Beek AJ, van Mechelen W. Return to work and occupational physicians’ management of common mental health problems–process evaluation of a randomized controlled trial. Scand J Work Environ Health. 2010;36:488–98.
Aust B, Helverskov T, Nielsen MB, Bjorner JB, Rugulies R, Nielsen K, et al. The Danish national return-to-work program–aims, content, and design of the process and effect evaluation. Scand J Work Environ Health. 2012;38:120–33.
Loisel P, Durand P, Abenhaim L, Gosselin L, Simard R, Turcotte J, et al. Management of occupational back pain—the Sherbrooke model—results of a pilot and feasibility study. Occup Environ Med. 1994;51:597–602.
Punnett L, Wegman DH. Work-related musculoskeletal disorders: the epidemiologic evidence and the debate. J Electromyograph Kinesiol. 2004;14:13–23.
Romanov K, Appelberg K, Honkasalo ML, Koskenvuo M. Recent interpersonal conflict at work and psychiatric morbidity: a prospective study of 15,530 employees aged 24–64. J Psychosom Res. 1996;40:169–76.
Stansfeld S, Candy B. Psychosocial work environment and mental health: a meta-analytic review. Scand J Work Env Health. 2006;32:443–62.
Netterstrøm B, Conrad N, Bech P, Fink P, Olsen O, Rugulies R, et al. The relation between work-related psychosocial factors and the development of depression. Epidemiol Rev. 2008;30:118–32.
Hensing G, Wahlstrom R. Chapter 7. Sickness absence and psychiatric disorders. Scand J Public Health. 2004;32:152–80.
Schademan HK, Jensen S, Thuesen F, Holt H. Virksomhedernes sociale engagement [Corporate social responsibility] [Danish]. Copenhagen: SFI—The Danish National Centre for Social Research; 2008.
Høgelund J, Holm A, McIntosh J. Does graded return-to-work improve sick-listed workers’ chance of returning to regular working hours? J Health Econ. 2010;29:158–69.
Acknowledgments
The study was supported by grants from the Danish Prevention Fund (Forebyggelsesfonden, grant #07-2-2-020) and the Danish Working Environment Research Fund (Arbejdsmiljøforskningsfonden, grant #31-2008-09). The study was approved and registered by the Danish Data Protection Agency (Registration number: 2008-54-0438).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Martin, M.H.T., Nielsen, M.B.D., Madsen, I.E.H. et al. Effectiveness of a Coordinated and Tailored Return-to-Work Intervention for Sickness Absence Beneficiaries with Mental Health Problems. J Occup Rehabil 23, 621–630 (2013). https://doi.org/10.1007/s10926-013-9421-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10926-013-9421-5