Abstract
Purpose
To identify germline mutations related to azoospermia etiology and reproductive potential of surgically retrieved spermatozoa, and to investigate the feasibility of predicting seminiferous tubule function of nonobstructive azoospermic men by transcriptomic profiling of ejaculates.
Materials and methods
Sperm specimens were obtained from 30 men (38.4 ± 6 years) undergoing epididymal sperm aspiration for obstructive azoospermia (OA, n = 19) acquired by vasectomy, or testicular biopsy for nonobstructive azoospermia (NOA, n = 11). To evaluate for a correlation with azoospermia etiology, DNAseq was performed on surgically retrieved spermatozoa, and cell-free RNAseq on seminal fluid (n = 23) was performed to predict spermatogenesis in the seminiferous tubule.
Results
Overall, surgically retrieved sperm aneuploidy rates were 1.7% and 1.8% among OA and NOA cohorts, respectively. OA men carried housekeeping-related gene mutations, while NOA men displayed mutations on genes involved in crucial spermiogenic functions (AP1S2, AP1G2, APOE). We categorized couples within each cohort according to ICSI clinical outcomes to investigate genetic causes that may affect reproductive potential. All OA-fertile men (n = 9) carried mutations in ZNF749 (sperm production), whereas OA-infertile men (n = 10) harbored mutations in PRB1, which is essential for DNA replication. NOA-fertile men (n = 8) carried mutations in MPIG6B (stem cell lineage differentiation), whereas NOA-infertile individuals (n = 3) harbored mutations in genes involved in spermato/spermio-genesis (ADAM29, SPATA31E1, MAK, POLG, IFT43, ATG9B) and early embryonic development (MBD5, CCAR1, PMEPA1, POLK, REC8, REPIN1, MAPRE3, ARL4C). Transcriptomic assessment of cell-free RNAs in seminal fluid from NOA men allowed the prediction of residual spermatogenic foci.
Conclusions
Sperm genome profiling provides invaluable information on azoospermia etiology and identifies gene-related mechanistic links to reproductive performance. Moreover, RNAseq assessment of seminal fluid from NOA men can help predict sperm retrieval during testicular biopsies.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
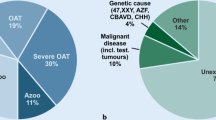
Male infertility accounts for approximately half of the causes of the inability to reproduce among infertile couples [1]. Fortunately, the introduction of ICSI has enhanced the treatment of even the most extreme forms of male factor infertility [2]. Among the different etiologies of male reproductive failure, the most challenging is azoospermia, which accounts for approximately 30% of all cases [3]. The most puzzling form of azoospermia is the testicular type [4]. While it can be attributed to genetic disorders, developmental abnormalities, hormonal imbalances, or consequent exposure to chemotherapy or radiation, the remaining cases are classified as idiopathic [5]. To define azoospermia, a detailed assessment of the patient’s medical history is performed, and various evaluations are carried out [6]. In cases of obstructive azoospermia (OA), assessment of the ejaculate does not yield any spermatozoa, whereas in cases of non-obstructive azoospermia (NOA), the ejaculate may inconsistently yield spermatozoa, representing an additional challenge that often requires an extensive search to identify sperm cells [2].
Once surgical approach is considered, chances of successful sperm retrieval in OA cases is likely to be >99%, while cases with testicular failure can be very unpredictable [2, 7]. Furthermore, if spermatozoa are identified in NOA cases, there also lies the ambiguity of whether azoospermia is due to primary testicular failure or depends on secondary environmental factors [8]. Therefore, it is crucial to characterize the genotypes of azoospermic individuals with impaired germ cell replication and gamete differentiation [9].
Genetic testing has become increasingly prevalent in male infertility screening and includes testing for whole-chromosomal structural aberrations, partial chromosomal defects, and monogenic diseases [10]. In men with azoospermia, genetic screening has revealed a higher incidence of constitutional karyotypic abnormalities [11]. Detection of Y-microdeletions can also identify genetic relationships of impaired spermatogenesis, which would not only remarkably limit reproductive competence, but would also be passed on to male offspring once assisted reproductive technologies (ART) are used [12]. Over the years, the application of genetic testing in azoospermic men has evolved, but it continues to primarily target the individual’s somatic tissue, and at times, a discrepancy between de-novo mutations on the germline vis-à-vis the somatic cells has been reported [13].
To date, genetic assessments have been aimed at highlighting the etiology of compromised sperm production [10]; however, the influence of genomic aberrations on the reproductive competence of surgically retrieved gametes remains relatively unknown.
Testicular spermatozoa have long been considered to be plagued by more chromosomal abnormalities than their ejaculated counterparts and were therefore perceived as more likely to generate aneuploid embryos [14,15,16]. This has recently been refuted [17], and subsequent reports have evidenced that the chromosomal and developmental characteristics of children born from spermatozoa retrieved from the seminiferous tubule are normal [17, 18]. This acquired knowledge on the safety of these gametes reiterates the relevance of understanding the etiology of the most common and concerning form of azoospermia, and reinforces interest in assessing the embryo developmental competence of these spermatozoa. Therefore, genetic assessment of the germline in relation to ART outcomes is necessary.
A pressing need has emerged for the treatment of NOA individuals, prompted by the unpredictability of sperm retrieval during testicular biopsy. This has recently been investigated by identifying rare polymorphisms, differentially expressed genes (DEGs), and the underlying DNA methylation mechanisms that affect sperm development [19, 20]. While most of this information was obtained from retrospective analyses of somatic cells, identification of genomic factors capable of non-invasively predicting successful retrieval of spermatozoa during testicular biopsy is of utmost importance to help streamline the clinical management of men with NOA.
In this study, we performed whole exome sequencing (WES) of the genome of spermatozoa retrieved surgically from azoospermic men to delineate germline mutations that may reveal the etiology of their spermatogenic failure and simultaneously elucidate their specific embryo developmental competence. In a subanalysis, we proposed a non-invasive method to identify testicular transcriptomes from cell-free RNAs in seminal fluid from NOA men to predict spermatozoa retrieval at testicular biopsy.
Materials and methods
Inclusion criteria and study design
This study was conducted between August 2019 and December 2021 at the Center for Reproductive Medicine of a major academic medical center. Men (37.1 ± 6 years) undergoing epididymal sperm aspiration for obstructive azoospermia (OA; n = 19), acquired by vasectomy, or testicular biopsy for nonobstructive azoospermia (NOA; n = 11) (36.8 ± 5 years), were considered eligible (Fig. 1a). Those with negative infertility workups, and for whom spermatozoa were successfully retrieved and subsequently used for ICSI, were included. Semen samples from eight fertile normozoospermic men comprised the control group.
a Men undergoing epididymal sperm aspiration for acquired obstructive azoospermia (OA), or testicular biopsy for nonobstructive azoospermia (NOA), were considered eligible for this study. Those for whom spermatozoa were successfully retrieved, and subsequently used for ICSI, were included. Whole exome sequencing (WES) on spermatozoal DNA was performed to compare copy number variants (CNVs) and common germline mutations between the OA and NOA cohorts, as well as according to the couples’ clinical outcomes. b RNAseq on seminal fluid from men with azoospermia (n = 23) were carried out to compare transcriptomic profiles according to whether spermatozoa were successfully retrieved after testicular biopsy (+ Sperm), or not (− Sperm)
Whole exome sequencing (WES) was performed on spermatozoal DNA from surgically retrieved specimens. Copy number variants (CNVs) and common germline mutations were identified and compared between the OA and NOA cohorts, as well as according to the couples’ clinical outcomes, while controlling for maternal age. Those who had successful pregnancies comprised the fertile subgroup, whereas those who were unsuccessful represented the infertile subgroup (Fig. 1a). Although we adopted a complete whole exome sequencing approach, for the purpose of this investigation, we primarily focused on those clinically meaningful genes that were specifically related to spermiogenesis, impaired fertilization, early embryo cleavage, as well as embryo developmental competence.
In a sub-analysis, we included men with suspected azoospermia (n = 88), for whom no spermatozoa were seen at initial semen analysis. For some men (n = 65), cryptozoospermia was detected after extensive semen analysis. For those with confirmed azoospermia (n = 23) in which no spermatozoa were identified despite extensive semen analyses, we performed transcriptomic assessments of cell-free RNAs in their seminal fluid. Four normozoospermic men were included as a control group. To identify genomic biomarkers that can predict testicular sperm retrieval outcome, we then compared the transcriptomic profiles of the 23 azoospermic men in relation to whether spermatozoa were successfully retrieved after testicular biopsy [( +)Sperm] or not [( −)Sperm] (Fig. 1b).
This study (IRB 1006011085) was approved by the Institutional Review Board, and all participants provided written informed consent with guaranteed confidentiality.
Infertility workup
Female infertility evaluation consisted of a comprehensive review of medical history, targeted physical examination, and tests focusing on ovarian reserve, ovulatory function, tubal patency, and uterine structural abnormalities. All couples underwent hormone profiling. Karyotyping was performed to confirm the absence of genetic alterations. All the couples had normal karyotypes and negative infertility workups, with no family history of genetic diseases. Standard male evaluation for azoospermic men was done according to the AUA/ASRM joint male infertility guidelines [21] with G-band analysis of karyotype and Y microdeletion analysis using multiplex PCR as previously described [22]. All male partners tested negative for Y-microdeletions, and none were taking testosterone supplements or medications to improve sperm parameters before or during the study. None of the patients had family history of infertility. Ejaculates were evaluated according to the 6th edition of the World Health Organization standards [23].
Extensive sperm search
Ejaculates were provided by masturbation following 1–2 days of sexual abstinence and allowed to liquefy at 37°C for at least 15 min. Initial analysis was conducted on 5 μL of the specimen using the Makler® sperm-counting chamber (Sefi Medical Instruments, Ltd., Haifa, Israel). If no spermatozoa were identified, the specimens were diluted in 3:1 Human Tubal Fluid medium (HTF Medium; Irvine Scientific) supplemented with Human Serum Albumin (HSA-Solution; Vitrolife), centrifuged at 3000 × g for 10 min, and reassessed. If spermatozoa were still not present, pellets were placed in 8 μL microdrops under oil in ICSI dishes to be searched under an inverted microscope at 400 × magnification.
Surgical sperm retrieval
Extensive sperm search was performed to exclude cryptozoospermia. Once azoospermia was confirmed, microdissection testicular sperm extraction (mTESE) was carried out as previously described [24, 25]. All surgeries were performed by a single urologist. Testicular samples were taken from only the most normal appearing tubules, distinguished by their larger size and greater opacity [26]. Tissue was dispersed in 300–400 μL of human tubal fluid medium (Irvine Scientific; Irvine, CA) and mechanically dispersed for several minutes by extensively cutting tissue into small pieces and passing the suspension through a 24G angiocatheter to assure complete disruption of tubules [27]. No other mechanical processing was done. Initial assessment for the presence of spermatozoa was carried out on glass slides using a phase contrast microscope (Olympus BX40) under 200× magnification. If no spermatozoa were identified, further extraction from the same testis and eventually the contralateral testis was performed. When no spermatozoa were identified, the testicular tissue suspension was digested with collagenase for 1 h, during which the suspension was mixed every 10–15 min to enhance enzymatic digestion [28]. An extensive search was subsequently carried out by several well-trained clinical embryologists to identify spermatozoa useful for ICSI.
Epididymal sperm aspiration was performed using a microsurgical technique as previously described [29, 30], where epididymal tubules were dissected and carefully punctured using an ophthalmic microknife (AccuSharp, Redmond, WA). The spermatozoa were then aspirated using micropipettes with 250–350 μm tip widths hand-drawn from glass tubing with an inner diameter of 0.6 mm and outer diameter of 0.9 mm (Drummond Scientific, Broomall, PA) [31]. Further epididymal tubule incisions were made to obtain spermatozoa of optimal quality, indicated by acceptable morphology (no major head defects and full-length sperm tail) and motility adequate for ICSI. Motility was considered present if spermatozoa displayed kinetic characteristics ranging from twitching in place, or progressive according to the intensity of the motion or displacement, since this displays proof of sperm viability [2]. All surgical samples were transported in 0.5 ml of human tubal fluid medium (Irvine Scientific; Irvine, CA) from the operating room to a sterile laboratory, where they were cryopreserved by slowly adding sperm cryopreservation medium (Irvine Scientific; Irvine, CA) until a 1:1 ratio of medium to sperm sample was achieved. After mixing, samples were transferred into labeled cryovials and stored in liquid nitrogen vapor until use in subsequent ICSI cycles.
Genetic profiling of surgically retrieved spermatozoa
DNA extraction and amplification were carried out using a commercial kit (Repli-G Single Cell; Qiagen, Hilden, Germany) [17], on 500 spermatozoa/specimen individually aspirated with an ICSI pipette. Specimens were sent to an external facility (Genewiz, Inc.; South Plainfield, NJ), where they underwent 150-bp paired-end exome sequencing on an Illumina HiSeq 2500 platform. Reads were trimmed to remove poor-quality nucleotides (error rate < 0.01), and quality assessments of each indexed sample were performed by qPCR (KAPA SYBR Faster Master Mix; Roche, Basel, Switzerland) with two primers (qPCR primer 1.1: AATGATACGGCGACCACCGAGAT, qPCR primer 1.2: CAAGCAGAAGACGGCATACGA). Resulting nM amounts were assessed to confirm successful adapter ligation. A high quality, average coverage of 85 × was obtained for the specimens, with > 90% exome coverage (Agilent SureSelect Human All Exon V6). The base calling accuracy for all samples was ~ 99.9%, as indicated by an average Phred quality score of Q38. After CNV detection was completed using CLC Genomics Server 9.0, the detected variants were annotated to identify gene mutations. All genomic coordinates were based on the human genome assembly GRCh38 (hg38).
Transcriptomic profiling of seminal plasma from NOA men
Total RNA was isolated and purified from the seminal plasma of men with confirmed azoospermia (n = 23) using an RNeasy Mini Kit spin column (RNeasy; Qiagen, Hilden, Germany) as previously described [32]. Nucleic acid quantification was performed with an Agilent 2100 bioanalyzer to determine the RNA integrity number (RIN), while RNA concentration was determined by a NanoDrop spectrophotometer and confirmed by Quibit RNA assay. After library prep (NEBNext Ultra RNA Library Prep kit, New England BioLabs Inc., Ipswich, MA), ribosomal RNAs were isolated by rRNA depletion (Ribo-Zero Gold rRNA Removal kit, Illumina, San Diego, CA). Sequencing was performed (NextSeq500; Illumina, San Diego, CA) by Genewiz, at a pilot-paired end 36 bp before being expanded to 50–60 M reads at 2 × 75 bp. Sequenced reads were then trimmed to remove low quality bases using Trimmomatic v.0.36 and mapped to the hg20 reference genome by CLC Genomics Server 9.0.
Ovarian superovulation and oocyte collection
Complete descriptions of the stimulation protocol and oocyte collection can be found in previous reports from our institution [33]. Briefly, patients were treated with daily gonadotropins (Follistim, Merck, Kenilworth, NJ, USA; Gonal-F, EMD-Serono, Geneva, Switzerland; and/or Menopur, Ferring Pharmaceuticals Inc, Parsippany, NJ, USA), and pituitary suppression was achieved by GnRH-antagonist (Ganirelix acetate, Merck, Kenilworth, NJ, USA; or Cetrotide, EMD-Serono Inc., Rockland, MA, USA). To attain follicular synchronization, some patients were treated with oral contraceptive pills (Ortho-Novum, Janssen Pharmaceuticals, Beerse, Belgium) prior to starting gonadotropins. The human chorionic gonadotropin trigger (hCG, Ovidreal, EMD Serono) was administered when at least 2 lead follicles reached an average diameter of ≥ 17 mm, and oocyte retrieval was subsequently performed 35–37 h afterwards, transvaginally under conscious sedation. Oocytes were incubated for 3–4 h, then washed in culture medium (home-brew, modified Cornell medium based on G1 and G2 components; Vitrolife, Sweden) [34, 35] and examined under an inverted microscope (TE2000U, Nikon USA, Melville, NY, USA) equipped with 2 × , 4 × , 10 × , 20 × , and 40 × objectives (Nikon CFI Apo & Nikon Polarized optics CFI Plan Fluor). Oocytes with extrusion of the first polar body (PB) were considered to be at the MII stage and ready for ICSI.
Embryo transfer and assessment of clinical outcome
Successful fertilization was assessed using an inverted microscope (TE2000U, Nikon USA, Melville, NY, USA) equipped with 2 × , 4 × , and 10 × objectives (Nikon CFI Apo), and 20 × and 40 × objectives (Nikon Polarized optics CFI Plan Fluor) [36]. In preparation for embryo transfer, patients received 50 mg of intramuscular progesterone supplement daily, starting from the day after ovulation. The overwhelming majority of patients (n = 26) underwent single embryo transfers of blastocysts on day 5, while the remaining (n = 4) transferred 2 embryos at the cleavage stage, on day 3. None of the couples included in this study opted for PGT-A testing. Serum βhCG levels were measured between 10 and 14 days post-embryo transfer. Clinical pregnancy was defined as fetal heart activity (+ FHB) detected on ultrasound at 7 weeks of gestation.
Bioinformatics and statistical analysis
CNV calling and gene mutation annotation was carried out using CLC Genomics Server 9.0 modules including NGS core tools/mapping and re-sequence analysis. Sperm aneuploidy was assessed by calculating the proportion of chromosomal abnormalities detected by CNV analysis [37]. The CNVs were then ranked according to these log-ratio values and corresponding genes annotated. Statistical thresholds of P < 0.0005 for significance and Q < 0.05 for false positive discovery were used. Sperm genetic profiles were compiled by identifying the mutations that were commonly carried by the spermatozoa from all men within the same group or subgroup.
For differential expression analysis, raw read counts were uploaded according to the DESeq2 v1.23.1 (LGPL, Bioconductor) pipeline and calculated in fragments per kilobase of exon of transcript per million mapped reads (FPKM). After data normalization, gene expression comparison was performed. To avoid over- or under-representing FPKM, an algorithm by edgeR (LGPL; Bioconductor) and CONTRA was implemented following the DESeq2 expression analysis to overcome experimental conditions such as fragmentation [32]. Power analyses were performed using STATA (Stata/BE 17; StataCorp LP, College Station, TX). The Mann–Whitney U test and two-tailed t test were used to compare the sperm aneuploidy between the NOA and OA cohorts (Graphpad Software, San Diego, CA). A P value of < 0.05 was considered statistically significant.
Results
A total of 30 men were enrolled in this study. Of these, 19 underwent epididymal sperm retrieval for acquired obstructive azoospermia (OA) due to vasectomy, yielding a sperm concentration of 1.1 ± 4 × 106/mL with 9 ± 12% motility. The remaining 11 men underwent testicular biopsies for nonobstructive azoospermia (NOA), yielding a sperm concentration of 0.03 ± 0.4 × 106/mL and 0.5 ± 1% motility (Table 1).
Spermatozoal DNA extraction and amplification from surgically retrieved specimens resulted in an average DNA concentration of 742 ± 520 ng/μL of good quality, confirmed by a 260/280 absorbance ratio of > 1.7. Copy number variant (CNV) assessment using WES did not indicate any significant differences in sperm aneuploidy between the two etiologies (OA, 1.7%; NOA, 1.8%) and control (1.1%).
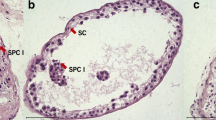
We then analyzed the annotated CNVs to compare the genetic profiles of the spermatozoa according to the etiology of azoospermia. Overall, our germline mutation analysis of spermatozoa from men in the OA cohort identified an average of 261.8 ± 297 gene mutations/patient, including 19.5 ± 3 that were clinically significant. Of these, we identified three genes (OR1D4, SLC17A7, and ATP4A) that were concurrently mutated in all men with OA. These genes were involved in basic cellular processes and were unrelated to sperm production or reproductive potential. Conversely, spermatozoa from men in the NOA cohort carried a higher occurrence of mutations (884.4 ± 103) (P < 0.05) than their OA counterparts, of which 7.1% were clinically meaningful (62.5 ± 21) (P < 0.0001). Moreover, across the entire NOA cohort, frameshift mutations were identified in five genes crucial for spermiogenic function (AP1S2, AP1G2, APOE), RNA transcription (POLR2L), and apoptosis (AP5M1) (Fig. 2 and Table 2).
Gene duplications and deletions were compared according to azoospermia etiology. Spermatozoa from the obstructive azoospermia (OA) cohort exclusively carried mutations on 3 housekeeping-related genes (OR1D4, SLC17A7, ATP4A) that are unrelated to sperm production or reproductive potential. Contrastingly, spermatozoa from all men in the nonobstructive azoospermia (NOA) group displayed mutations on 5 genes involved in RNA transcription (POLR2L), apoptosis (AP5M1), and crucial spermiogenic functions (AP1S2, AP1G2, APOE). These mutations were not identified in specimens from the OA cohort
To further investigate the genetic causes that may impair the reproductive potential of these surgically retrieved spermatozoa, we categorized couples from the OA and NOA cohorts into subgroups, according to their reproductive outcomes (Table 3). Couples from the OA cohort (maternal age, 36.5 ± 3 years; paternal age, 36.8 ± 7 years) each underwent one ICSI cycle, resulting in a delivery rate of 47.4% (9/19). Spermatozoa isolated from the OA-fertile subgroup (n = 9) carried synonymous mutations in a gene specifically affecting sperm production (ZNF749), which was not identified in any other subgroup. Spermatozoa from OA-infertile individuals (n = 10) displayed missense mutations in a gene responsible for controlling essential DNA replication (PRB1), which was also not identified in any other subgroup (Fig. 3).
Spermatozoa from the fertile obstructive azoospermia (OA-fertile) subgroup carried mutations on a spermatogenesis-related gene (ZNF749), while their infertile obstructive azoospermia (OA-infertile) counterparts displayed mutations on a gene (PRB1) responsible for controlling essential DNA replication
Couples from the NOA cohort (maternal age, 36.8 ± 2 years; paternal age, 37.1 ± 6) underwent 11 ICSI cycles, yielding a delivery rate of 72.7% (8/11) (Table 3). Spermatozoa from the NOA-fertile men (n = 8) all carried mild mutations on MPIG6B, a gene involved in stem cell lineage differentiation, while gametes from each of their NOA-infertile counterparts (n = 3) displayed frameshift and point mutations on genes involved in spermato-/spermiogenesis (ADAM29, SPATA31E1, MAK, POLG, IFT43, ATG9B), apoptosis (ADAMTSL4, CSRNP3, BAX, AATK), and acrosomal function (RBFOX2, RTEL1). Most importantly, they carried severe mutations in the genes that encode early embryonic development (MBD5, CCAR1, PMEPA1, POLK, REC8, REPIN1, MAPRE3, ARL4C) (Fig. 4).
Spermatozoa from the fertile nonobstructive azoospermia (NOA-fertile) subgroup carried mutations on a single gene (MPIG6B) involved in stem cell lineage differentiation, while spermatozoa from each of the infertile counterparts displayed mutations on genes not only involved in spermatogenesis, but also apoptosis, acrosomal function, and most importantly, early embryonic development
Next, we performed a sub-analysis using RNAseq to determine whether the transcriptomic profiles of seminal plasma from men can predict successful sperm extraction at testicular biopsy. For this assessment, we included a total of 88 men (37.3 ± 6 years) with suspected azoospermia. We performed extensive semen analyses of their ejaculates and identified rare spermatozoa in the majority (n = 65) of these patients, whereas spermatozoa were not identified in the remaining 23 men. Therefore, these 23 patients with confirmed azoospermia subsequently underwent testicular biopsy.
RNAseq was performed on circulating cell-free RNA in the seminal fluid from each azoospermic patient (concentration 9.1 ± 4 ng/μL). Eleven men (39.0 ± 12 years) who underwent successful testicular sperm retrievals were defined as the ( +)Sperm cohort, while 12 (34.3 ± 5 years) with unsuccessful outcomes comprised the ( −)Sperm cohort. Transcriptomic analyses of seminal plasma from the ( +)Sperm cohort identified 12 significantly imbalanced genes that were exclusively shared by all men in this group. These genes were primarily involved in spermatogenesis (PRM2, KLHL10, SPZ1, SPATA12, H1FNT), sperm maturation (ADAM21), cell cycle regulation (CENPU, TSPAN6, BOD1L2), and sperm function (TTC29, ZBBX, WBP2NL) (Table 4).
Transcriptomic analyses of the (-)Sperm cohort identified 19 significantly imbalanced genes that were exclusively shared in the seminal plasma. These genes were mainly involved in spermatogenesis (PHF7, GAPDHS, ACSBG2, CABS1, TPD52L3, PGK2, CAPZA2, TSSK6, UBQLN3, TEX44, SPATA42), sperm function (TCP11, CABYR, ODF1, ODF3L2, FSCB, AKAP4, TPPP2), and testis development (SPEM2) (Table 5).
Upon comparing the transcriptomic profiles between the ( +) and ( −)Sperm cohorts, we identified eight genes that were significantly over- or underexpressed and shared among the entire azoospermic group (Table 6). These genes are involved in spermatogenesis (TMCO5B, C10orf62, SMKR1, SPZ1), sperm function (NEU1, TPTE2), and testis development (TRPC1, IGSF11-AS1). A comparison of the expression of each gene between the two subgroups showed that TPTE2, implicated in spermatogenic defects and normally highly expressed in the testis, was expressed in the seminal plasma from 81.8% (9/11) of the ( +)Sperm group; most importantly, NEU1, involved in acrosome development and crucial for sperm capacitation, was overexpressed in all men from the ( +)Sperm cohort. Interestingly, these two genes, together with IGSF11-AS1, were consistently underexpressed in the ( −)Sperm cohort (P < 0.0001) (Fig. 5).
RNAseq was performed on the seminal fluid from 23 azoospermic patients. Eleven men who underwent successful testicular sperm retrievals were defined as the ( +)Sperm cohort, while 12 with unsuccessful outcomes comprised the ( −)Sperm cohort. We identified 8 imbalanced genes that were shared among all azoospermic men. TPTE2 was partially expressed in the seminal plasma from 81.8% (9/11) of the ( +)Sperm group, while IGSF11-AS1 was underexpressed in the seminal plasma from all ( −)Sperm men. Most interestingly, NEU1 was identified as the sole gene that was exclusively underexpressed in all men from the ( −)Sperm cohort, yet simultaneously overexpressed in all men from the ( +)Sperm cohort
Discussion
Despite the evolution of genetic testing in the field of male infertility, some gaps remain in its application, particularly in cases requiring testicular sperm extraction. For instance, the assessment of men with azoospermia is primarily focused on identifying the etiology of compromised sperm production and does not extend to the evaluation of the reproductive potential of surgically retrieved gametes. Earlier studies have assessed the chromosomal profile of testicular spermatozoa [14, 15, 38], but these were carried out using early cytogenetic techniques, yielding inaccurate results that fogged the situation and prompted concerns related to the safety of using such specimens. However, recent evidence has mitigated these concerns by showing that clinical outcomes are not impaired in cycles using testicular spermatozoa compared with those using ejaculated specimens [17].
Recent studies on the genetics of azoospermia have identified specific genes associated with a large spectrum of testis phenotypes, from hypospermatogenesis (USP9Y) to residual spermatogenesis (PRY, RBBMY, BPY2, DAZ) [39,40,41]. Rare variants of ADGRG2 have also been associated with unexplained CBAVD cases that do not display any pathogenic CFTR mutations [39]. However, these assessments were primarily performed on somatic tissues. Notably, there is a clear dichotomy between somatic cells and the germline, including the response to environmental stimuli, as well as the type and incidence of mutations associated with the transgenerational role of the latter [42]. Germline and somatic mutations also occur in different settings. Although public databases of somatic and germline mutations indicate many shared variants, this may primarily be attributed to basic chemical vulnerabilities that are common in DNA from both environments [43]. In the current study, we specifically screened spermatozoal DNA to identify germline mutations related to whether azoospermia was due to testicular or post-testicular causes, and to identify key gene–related mechanistic links to the reproductive performance of the surgically retrieved specimens.
Our gamete genome comparison between the two azoospermia etiologies revealed a significantly lower incidence of mutations in the OA cohort than in the NOA cohort. Additionally, the OA cohort concurrently carried mutations in three housekeeping genes (OR1D4, SLC17A7, ATP4A) unrelated to reproductive competence, whereas the NOA cohort displayed frameshift mutations in genes crucial for spermatogenic function (AP1S2, AP1G2, APOE), RNA transcription (POLR2L), and apoptosis (AP5M1).
We then divided the OA cohort according to ICSI outcomes and found that spermatozoa from all men in the OA-fertile subgroup displayed mutations in a gene (ZNF749) from the zinc finger protein family, which has been shown to affect sperm production [44]. This finding was unexpected, given that the OA participants were all post-vasectomies with a history of normal spermatogenesis. However, the mutations were synonymous and would not have disturbed the resulting protein structure. The unaffected protein function, characterized by stable zinc ion activity, also suggests that the subsequent sperm-specific zinc signature crucial for capacitation and sperm-zona pellucida interactions [45] is sustained, which explains why the clinical outcomes were not impaired in this subgroup.
Spermatozoa from all men in the OA-infertile subgroup exclusively carried missense mutations on PRB1. While this gene is known for its critical role in clipping of the histone H3 N-terminal tails, thereby maintaining cellular resistance to DNA-damaging agents in Saccharomyces cerevisiae [46], its capacity to do so in humans is unknown. However, sperm chromatin fragmentation (SCF) assessment by the TUNEL assay showed elevated SCF, suggesting that PRB1 alterations carried by spermatozoa from infertile men with obstructive azoospermia, acquired by vasectomy, may affect their ability to withstand the action of oxygen free radicals, subsequently impairing embryo development and precluding these patients from achieving pregnancy [47].
Our sperm genetic assessment for the NOA-fertile subgroup identified mutations in a single gene, MPIG6B. Although this gene is primarily involved in hematopoietic lineage differentiation, gene expression clustering has shown that it behaves in a coordinated manner with CATSPERD [48], which is crucial for sperm capacitation and successful fertilization. However, this subgroup obtained a fertilization rate of 66.9%, which suggests that any sperm acrosomal flaws from mutations in MPIG6B or other genes within the same cluster were successfully addressed by ICSI, which is known for its ability to overcome defects in sperm-egg fusion and acrosomal development [49]. Indeed, while the NOA-infertile subgroup carried mutations in genes involved in spermato/spermio-genesis (ADAM29, SPATA31E1, MAK, POLG, IFT43, ATG9B), they also displayed additional frameshift and point mutations in genes that encode early embryonic development (MBD5, CCAR1, PMEPA1, POLK, REC8, REPIN1, MAPRE3, ARL4C), which may be a concurrent compounding factor in the implantation failure observed in these couples.
Next, we investigated whether the gene expression profiling of cell-free RNAs in seminal plasma could be used to predict successful testicular sperm retrieval in men with non-obstructive azoospermia. Although the chance of successful micro-TESE in NOA men can reach 60%, the procedure may still fail to yield spermatozoa. The evaluation of several factors has been proposed to predict successful retrieval, including FSH [50], inhibin B [51], genetics [52], and histopathology [53]. Although histopathology is considered the most reliable method for predicting a successful micro-TESE, it is equally invasive. Our RNAseq assessment of circulating cell-free RNA in seminal plasma identified several differentially expressed genes (DEGs), including those involved in spermatogenesis and sperm function, regardless of whether spermatozoa were successfully retrieved after testicular biopsy. However, the differential expression of a select number of genes distinguished those NOA men who had successful micro-TESE sperm retrievals from those who were unsuccessful. Specifically, genes crucial for sperm maturation and cell cycle regulation were underexpressed in the seminal plasma of men who underwent unsuccessful procedures, suggesting that the probability of retrieving spermatozoa is correlated with the downregulation of genes involved in these functions. This was further illustrated by the expression profile of NEU1, which was consistently overexpressed in the seminal plasma from the entire ( +)Sperm cohort, yet jointly underexpressed in all men from the ( −)Sperm cohort. This observation may also warrant further investigation into other genes that are responsible for sperm acrosome function and development.
The limitations of this study stem mainly from the relatively small sample size. Couples were selected according to their willingness to participate, and underwent thorough counseling by a reproductive endocrinologist, reproductive urologist, and research coordinators prior to giving their written consent. There was no difference in demographics between the participants and non-participants. This included ethnicity, socioeconomic status, age, and hormonal profile, AMH level, and BMI of the female partners. Although maternal age was controlled for, confounding factors related to the female partner cannot undoubtedly be excluded. In addition, while we adopted a complete whole exome sequencing approach, for the purpose of this investigation, we primarily focused on those genes suspected to be involved in spermatogenesis and embryo developmental competence. Although spermatozoa from men unable to reproduce displayed common gene mutations that provide information about their condition, these findings should still be prospectively validated. Additionally, somatic DNA analysis could determine whether any of the germline mutations identified in this study overlapped with the somatic mutations of the same genes. A comparison of germline and somatic mutations within the same individual would definitively reveal the relationship between the two types of abnormalities and support the diagnostic value of our germline genomic assessment. It is also important to determine the proportion of gametes that carry these mutations, especially for couples undergoing ICSI, where spermatozoa are individually selected. Therefore, future endeavors would include the utilization of single-cell NGS to explore gamete heterozygosity and mutation rates in individual spermatozoa, due to the inherent variability that has been identified within a spermatozoa population [54]. A concurrent somatic RNAseq analysis could also identify gene imbalances that influence spermatogenesis, which may encourage reconsideration of germline mutations initially dismissed as clinically irrelevant. A confirmatory assessment of circulating cell-free nucleic acids in the seminal fluid of NOA patients may also serve to identify additional predictive biomarkers at the genomic and transcriptional levels. Nevertheless, to our knowledge this is the first study that attempts to attribute reproductive competence to spermatozoa retrieved via surgical intervention by profiling their gene sequences. These findings, combined with our RNAseq observations, can potentially be incorporated into a diagnostic tool to categorize and counsel azoospermic men who are candidates for surgical sperm retrieval. Therefore, screening for DEGs and gene mutations that can predict TESE success and reproductive potential, respectively, can be used as a non-invasive biomarker tool to spare patients from unsuccessful surgery. By querying the sperm genome of surgically retrieved specimens, we identified clear germline mutations related to the origin of azoospermia, and most importantly, the ability to support a healthy pregnancy by pinpointing key gene–related mechanistic links to impaired embryo development. RNAseq of seminal fluid from NOA men also revealed predictive indicators of favorable sperm retrieval at testicular biopsy. In conjunction, these genetic and transcriptomic assessments could potentially serve as a useful precision medicine approach, not only to spare azoospermic men from an unpleasant procedure, but most importantly, to pinpoint the diagnosis and predict clinical outcomes for couples affected by the most severe form of male factor infertility.
References
Practice Committee of the American Society for Reproductive M, the Practice Committee of the Society for Reproductive E, Infertility. Electronic address aao. Optimizing natural fertility: a committee opinion. Fertil Steril. 2022;117(1):53–63. https://doi.org/10.1016/j.fertnstert.2021.10.007.
Palermo GD, Neri QV, Schlegel PN, Rosenwaks Z. Intracytoplasmic sperm injection (ICSI) in extreme cases of male infertility. PLoS One. 2014;9(12):e113671. https://doi.org/10.1371/journal.pone.0113671.
Esteves SC, Miyaoka R, Agarwal A. An update on the clinical assessment of the infertile male. Clinics. 2011;66(4):691–700. https://doi.org/10.1590/S1807-59322011000400026.
Andrade DL, Viana MC, Esteves SC. Differential diagnosis of azoospermia in men with infertility. J Clin Med. 2021;10(14):ARTN 3144. https://doi.org/10.3390/jcm10143144.
Kang C, Punjani N, Schlegel PN. Reproductive chances of men with azoospermia due to spermatogenic dysfunction. J Clin Med. 2021;10(7). https://doi.org/10.3390/jcm10071400.
Punjani N, Kang C, Lamb DJ, Schlegel PN. Current updates and future perspectives in the evaluation of azoospermia: a systematic review. Arab J Urol. 2021;19(3):206–14. https://doi.org/10.1080/2090598x.2021.1954415.
Bernie AM, Ramasamy R, Schlegel PN. Predictive factors of successful microdissection testicular sperm extraction. Basic Clin Androl. 2013;23:5. https://doi.org/10.1186/2051-4190-23-5.
Krzastek SC, Farhi J, Gray M, Smith RP. Impact of environmental toxin exposure on male fertility potential. Transl Androl Urol. 2020;9(6):2797–813. https://doi.org/10.21037/tau-20-685.
He H, Yu F, Shen W, Chen K, Zhang L, Lou S, et al. The novel key genes of non-obstructive azoospermia affect spermatogenesis: transcriptomic analysis based on RNA-Seq and scRNA-Seq data. Front Genet. 2021;12:608629. https://doi.org/10.3389/fgene.2021.608629.
Cariati F, D’Argenio V, Tomaiuolo R. The evolving role of genetic tests in reproductive medicine. J Transl Med. 2019;17(1):ARTN 267. https://doi.org/10.1186/s12967-019-2019-8.
Singhal P, Pendkur G, Parihar RS, Singh S, Chakrabarty BK, Raghavendra SK. The spectrum of chromosomal abnormalities and endocrine profile of male infertility with nonobstructive semen abnormality: a case-control study. J Hum Reprod Sci. 2021;14(2):175–83. https://doi.org/10.4103/jhrs.jhrs_165_20.
Rabinowitz MJ, Huffman PJ, Haney NM, Kohn TP. Y-chromosome microdeletions: a review of prevalence, screening, and clinical considerations. Appl Clin Genet. 2021;14:51–9. https://doi.org/10.2147/Tacg.S267421.
Esteves SC. A clinical appraisal of the genetic basis in unexplained male infertility. J Hum Reprod Sci. 2013;6(3):176–82. https://doi.org/10.4103/0974-1208.121419.
Vozdova M, Heracek J, Sobotka V, Rubes J. Testicular sperm aneuploidy in non-obstructive azoospermic patients. Hum Reprod. 2012;27(7):2233–9. https://doi.org/10.1093/humrep/des115.
Levron J, Aviram-Goldring A, Madgar I, Raviv G, Barkai G, Dor J. Sperm chromosome abnormalities in men with severe male factor infertility who are undergoing in vitro fertilization with intracytoplasmic sperm injection. Fertil Steril. 2001;76(3):479–84. https://doi.org/10.1016/s0015-0282(01)01957-4.
Rodrigo L, Rubio C, Peinado V, Villamón R, Al-Asmar N, Remohí J, et al. Testicular sperm from patients with obstructive and nonobstructive azoospermia: aneuploidy risk and reproductive prognosis using testicular sperm from fertile donors as control samples. Fertil Steril. 2011;95(3):1005–12. https://doi.org/10.1016/j.fertnstert.2010.10.022.
Cheung S, Schlegel PN, Rosenwaks Z, Palermo GD. Revisiting aneuploidy profile of surgically retrieved spermatozoa by whole exome sequencing molecular karyotype. Plos One. 2019;14(1):ARTN e0210079. https://doi.org/10.1371/journal.pone.0210079.
Cheung S, Neri QV, Squires J, Rosenwaks Z, Palermo GD. Assessing the cognitive and behavioral development of 3-year-old children born from fathers with severe male infertility. Am J Obstet Gynecol. 2021;224(5):ARTN 508.e1-e11. https://doi.org/10.1016/j.ajog.2020.11.030.
He HH, Yu F, Shen W, Chen KY, Zhang LJ, Lou S, et al. The novel key genes of non-obstructive azoospermia affect spermatogenesis: transcriptomic analysis based on RNA-Seq and scRNA-Seq data. Front Genet. 2021;12:ARTN 608629. https://doi.org/10.3389/fgene.2021.608629.
Rotondo JC, Lanzillotti C, Mazziotta C, Tognon M, Martini F. Epigenetics of male infertility: the role of DNA methylation. Front Cell Dev Biol. 2021;09:ARTN 689624. https://doi.org/10.3389/fcell.2021.689624.
Schlegel PN, Sigman M, Collura B, De Jonge CJ, Eisenberg ML, Lamb DJ, et al. Diagnosis and treatment of infertility in men: AUA/ASRM guideline part I. Fertil Steril. 2021;115(1):54–61. https://doi.org/10.1016/j.fertnstert.2020.11.015.
Girardi SK, Mielnik A, Schlegel PN. Submicroscopic deletions in the Y chromosome of infertile men. Hum Reprod. 1997;12(8):1635–41. https://doi.org/10.1093/humrep/12.8.1635.
WHO. WHO laboratory manual for the examination and processing of human semen. 6th ed. Geneva: World Health Organization; 2021 [cited 2021 accessed on 23 December 2021]. 6th ed: [Available online: https://www.who.int/publications/i/item/9789240030787]. Available from: https://www.who.int/publications/i/item/9789240030787.
Dardashti K, Williams R, Goldstein M. Microsurgical testis biopsy: a novel technique for diagnostic and therapeutic retrieval of testicular tissue. J Urol. 2000;163:1206–7.
Jow WW, Steckel J, Schlegel PN, Magid MS, Goldstein M. Motile sperm in human testis biopsy specimens. J Androl. 1993;14(3):194–8.
Schlegel PN. Testicular sperm extraction: microdissection improves sperm yield with minimal tissue excision. Hum Reprod. 1999;14(1):131–5. https://doi.org/10.1093/humrep/14.1.131.
Ostad M, Liotta D, Ye Z, Schlegel PN. Testicular sperm extraction for nonobstructive azoospermia: results of a multibiopsy approach with optimized tissue dispersion. Urology. 1998;52(4):692–6. https://doi.org/10.1016/s0090-4295(98)00322-7.
Ramasamy R, Reifsnyder JE, Bryson C, Zaninovic N, Liotta D, Cook CA, et al. Role of tissue digestion and extensive sperm search after microdissection testicular sperm extraction. Fertil Steril. 2011;96(2):299–302. https://doi.org/10.1016/j.fertnstert.2011.05.033.
Matthews GJ, Goldstein M. A simplified method of epididymal sperm aspiration. Urology. 1996;47:123–5.
Schlegel PN, Berkeley AS, Goldstein M, Cohen J, Alikani M, Adler A, et al. Epididymal micropuncture with in-vitro fertilization and oocyte micromanipulation for the treatment of unreconstructable obstructive azoospermia. Fertil Steril. 1994;61(5):895–901.
Stahl PJ, Schlegel PN, Goldstein M. Sperm retrieval and quality evaluation. Methods Mol Biol. 2014;1154:361–84. https://doi.org/10.1007/978-1-4939-0659-8_17.
Cheung S, Parrella A, Rosenwaks Z, Palermo GD. Genetic and epigenetic profiling of the infertile male. PLoS ONE. 2019;14(3):e0214275. https://doi.org/10.1371/journal.pone.0214275.
Huang JY, Rosenwaks Z. Assisted reproductive techniques. Methods Mol Biol. 2014;1154:171–231. https://doi.org/10.1007/978-1-4939-0659-8_8.
Gardner DK, Lane M, Spitzer A, Batt PA. Enhanced rates of cleavage and development for sheep zygotes cultured to the blastocyst stage in vitro in the absence of serum and somatic cells: amino acids, vitamins, and culturing embryos in groups stimulate development. Biol Reprod. 1994;50(2):390–400.
Gardner DK, Lane M. Culture and selection of viable blastocysts: a feasible proposition for human IVF? Hum Reprod Update. 1997;3(4):367–82.
Palermo GD, Cohen J, Alikani M, Adler A, Rosenwaks Z. Intracytoplasmic sperm injection: a novel treatment for all forms of male factor infertility. Fertil Steril. 1995;63(6):1231–40. https://doi.org/10.1016/S0015-0282(16)57603-1.
Zhang R, Chen XB, Wang D, Chen X, Wang C, Zhang YH, et al. Prevalence of chromosomal abnormalities identified by copy number variation sequencing in high-risk pregnancies, spontaneous abortions, and suspected genetic disorders. J Int Med Res. 2019;47(3):1169–78. https://doi.org/10.1177/0300060518818020.
Hwang K, Weedin JW, Lamb DJ. The use of fluorescent in situ hybridization in male infertility. Ther Adv Urol. 2010;2(4):157–69. https://doi.org/10.1177/1756287210373758.
Cioppi F, Rosta V, Krausz C. Genetics of azoospermia. Int J Mol Sci. 2021;22(6). https://doi.org/10.3390/ijms22063264.
Tang D, Li K, Geng H, Xu C, Lv M, Gao Y, et al. Identification of deleterious variants in patients with male infertility due to idiopathic non-obstructive azoospermia. Reprod Biol Endocrinol. 2022;20(1):63. https://doi.org/10.1186/s12958-022-00936-z.
Wyrwoll MJ, Temel SG, Nagirnaja L, Oud MS, Lopes AM, van der Heijden GW, et al. Bi-allelic mutations in are a frequent cause of meiotic arrest and severely impaired spermatogenesis leading to male infertility. Am J Hum Genet. 2020;107(2):342–51. https://doi.org/10.1016/j.ajhg.2020.06.010.
Feng L, Chen X. Epigenetic regulation of germ cells-remember or forget? Curr Opin Genet Dev. 2015;31:20–7. https://doi.org/10.1016/j.gde.2015.04.003.
Meyerson W, Leisman J, Navarro FCP, Gerstein M. Origins and characterization of variants shared between databases of somatic and germline human mutations. BMC Bioinformatics. 2020;21(1):ARTN 227. https://doi.org/10.1186/s12859-020-3508-8.
Ishizuka M, Ohtsuka E, Inoue A, Odaka M, Ohshima H, Tamura N, et al. Abnormal spermatogenesis and male infertility in testicular zinc finger protein Zfp318-knockout mice. Dev Growth Differ. 2016;58(7):600–8. https://doi.org/10.1111/dgd.12301.
Kerns K, Sharif M, Zigo M, Xu W, Hamilton LE, Sutovsky M, et al. Sperm cohort-specific zinc signature acquisition and capacitation-induced zinc flux regulate sperm-oviduct and sperm-zona pellucida interactions. Int J Mol Sci. 2020;21(6):ARTN 2121. https://doi.org/10.3390/ijms21062121.
Xue Y, Vashisht AA, Tan Y, Su T, Wohlschlegel JA. PRB1 is required for clipping of the histone H3 N terminal tail in Saccharomyces cerevisiae. PLoS One. 2014;9(2):e90496. https://doi.org/10.1371/journal.pone.0090496.
Gualtieri R, Kalthur G, Barbato V, Longobardi S, Di Rella F, Adiga SK, et al. Sperm oxidative stress during in vitro manipulation and its effects on sperm function and embryo development. Antioxidants (Basel). 2021;10(7). https://doi.org/10.3390/antiox10071025.
HumanProteinAtlas. Available from: https://www.proteinatlas.org/ENSG00000204420-MPIG6B/cell+line. Accessed 12 Sept 2023.
Neri QV, Lee B, Rosenwaks Z, Machaca K, Palermo GD. Understanding fertilization through intracytoplasmic sperm injection (ICSI). Cell Calcium. 2014;55(1):24–37. https://doi.org/10.1016/j.ceca.2013.10.006.
Bohring C, Schroeder-Printzen I, Weidner W, Krause W. Serum levels of inhibin B and follicle-stimulating hormone may predict successful sperm retrieval in men with azoospermia who are undergoing testicular sperm extraction. Fertil Steril. 2002;78(6):1195–8. https://doi.org/10.1016/S0015-0282(02)04259-0.
Zhu ZG, Zhao ZG, Pang QY, Chen T, Zhang JM, Zhang TJ, et al. Predictive significance of serum inhibin B on testicular haploid gamete retrieval outcomes in nonobstructive azoospermic men. Asian J Androl. 2019;21(2):137–42. https://doi.org/10.4103/aja.aja_94_18.
Goel R, Batra H, Kumar M, Dada R, Kumar R. Evaluation of cell-free seminal mRNA for the diagnosis of obstruction as the cause of azoospermia in infertile men: a prospective cohort study. Andrologia. 2022; ARTN e14364. https://doi.org/10.1111/and.14364.
Das A, Halpern JA, Darves-Bornoz AL, Patel M, Wren J, Keeter MK, et al. Sperm retrieval success and testicular histopathology in idiopathic nonobstructive azoospermia. Asian J Androl. 2020;22(6):555–9. https://doi.org/10.4103/aja.aja_137_19.
Bell AD, Mello CJ, Nemesh J, Brumbaugh SA, Wysoker A, McCarroll SA. Insights into variation in meiosis from 31,228 human sperm genomes. Nature. 2020;583(7815):259-+. https://doi.org/10.1038/s41586-020-2347-0.
Acknowledgments
We thank the clinicians, scientists, embryologists, and nursing staff of The Ronald O. Perelman & Claudia Cohen Center for Reproductive Medicine. We are also grateful to the Reproductive Urologists of New York Presbyterian Hospital for their close collaboration.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Cheung, S., Ng, L., Xie, P. et al. Genetic profiling of azoospermic men to identify the etiology and predict reproductive potential. J Assist Reprod Genet 41, 1111–1124 (2024). https://doi.org/10.1007/s10815-024-03045-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10815-024-03045-5