Abstract
Purpose
To study the effector mechanism against pathogens of polymorphonuclear neutrophils (PMN) and macrophages, called ETosis, involving the release of extracellular traps (ETs) in patients with acute epididymitis. To assess the different ET phenotypes present in semen samples and to identify correlations between ETosis and clinical parameters.
Materials and methods
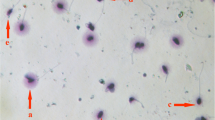
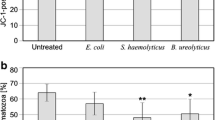
Samples from patients diagnosed with acute epididymitis were examined and compared with samples from uninfected controls. Biochemical analyses of seminal fluid included determination of peroxidase, α-glucosidase, fructose, and elastase levels. ETosis in semen was determined through presence of citrullinated histones, global histones, and extracellular DNA. Different ETosis phenotypes such as spread ETs, aggregated ETs, and diffuse ETs were identified by co-localisation of extruded DNA with myeloperoxidase and global histones. Anti-CD15+ and anti-CD68+ antibodies were used to identify different cell lines.
Results
Revealed a high number of ETs compared with the control group. The mean number of CD15+PMN and CD68+ macrophages was higher in the acute epididymitis group. ETosis increase in ejaculates correlated with clinical parameters such as enhancement of elastase concentrations and diminution of fructose in the semen.
Conclusions
This work shows for the first time the presence of ETs and their components in semen from patients with acute epididymitis. The presence of infections is an important factor for induction of ETs in semen. Furthermore, the presence of ETosis in ejaculates is suggestive of developing infectious processes and might possibly have a diagnostic value.



Similar content being viewed by others
Data availability
The data and material can be requested to the corresponding author.
References
Inhorn MC, Patrizio P. Infertility around the globe: new thinking on gender, reproductive technologies and global movements in the 21st century. Hum Reprod Update. 2015;21(4):411–26.
Pilatz A, Kilb J, Kaplan H, et al. High prevalence of urogenital infection/inflammation in patients with azoospermia does not impede surgical sperm retrieval. Andrologia. 2019;51(10):e13401.
Pilatz A, Hossain H, Kaiser R, Mankertz A, Schüttler CG, Domann E, et al. Acute epididymitis revisited: impact of molecular diagnostics on etiology and contemporary guideline recommendations. Eur Urol. 2015;68(3):428–35.
Sanchez R, Villegas J, Pena P, Miska W, Schill WB. Determination of peroxidase positive cells in semen: is it a secure parameter for the diagnosis of silent genital infections? Rev Med Chil. 2003;131(6):613–6.
Aitken RJ. A free radical theory of male infertility. Reprod Fertil Dev. 1994;6(1):19–23 discussion 23–14.
Plante M, de Lamirande E, Gagnon C. Reactive oxygen species released by activated neutrophils, but not by deficient spermatozoa, are sufficient to affect normal sperm motility. Fertil Steril. 1994;62(2):387–93.
Baker HW, Brindle J, Irvine DS, Aitken RJ. Protective effect of antioxidants on the impairment of sperm motility by activated polymorphonuclear leukocytes. Fertil Steril. 1996;65(2):411–9.
Kumar N, Singh AK. Reactive oxygen species in seminal plasma as a cause of male infertility. J Gynecol Obstet Hum Reprod. 2018;47:565–72.
Easterhoff D, Ontiveros F, Brooks LR, Kim Y, Ross B, Silva JN, et al. Semen-derived enhancer of viral infection (SEVI) binds bacteria, enhances bacterial phagocytosis by macrophages, and can protect against vaginal infection by a sexually transmitted bacterial pathogen. Antimicrob Agents Chemother. 2013;57(6):2443–50.
Kurzawa R. Modulation of peritoneal macrophage function: effect of selected drugs on their activity and sperm phagocytosis. Ann Acad Med Stetin. 1997;43:79–97.
Marey MA, Liu J, Kowsar R, Haneda S, Matsui M, Sasaki M, et al. Bovine oviduct epithelial cells downregulate phagocytosis of sperm by neutrophils: prostaglandin E2 as a major physiological regulator. Reproduction. 2014;147(2):211–9.
Zambrano F, Carrau T, Gartner U, et al. Leukocytes coincubated with human sperm trigger classic neutrophil extracellular traps formation, reducing sperm motility. Fertil Steril. 2016;106(5):1053–60 e1051.
Uhl B, Vadlau Y, Zuchtriegel G, Nekolla K, Sharaf K, Gaertner F, et al. Aged neutrophils contribute to the first line of defense in the acute inflammatory response. Blood. 2016;128(19):2327–37.
Castanheira FVS, Kubes P. Neutrophils and NETs in modulating acute and chronic inflammation. Blood. 2019;133(20):2178–85.
Brinkmann V, Reichard U, Goosmann C, Fauler B, Uhlemann Y, Weiss DS, et al. Neutrophil extracellular traps kill bacteria. Science. 2004;303(5663):1532–5.
Fuchs TA, Abed U, Goosmann C, Hurwitz R, Schulze I, Wahn V, et al. Novel cell death program leads to neutrophil extracellular traps. J Cell Biol. 2007;176(2):231–41.
Granger V, Faille D, Marani V, Noël B, Gallais Y, Szely N, et al. Human blood monocytes are able to form extracellular traps. J Leukoc Biol. 2017;102(3):775–81.
Papayannopoulos V, Metzler KD, Hakkim A, Zychlinsky A. Neutrophil elastase and myeloperoxidase regulate the formation of neutrophil extracellular traps. J Cell Biol. 2010;191(3):677–91.
Munoz-Caro T, Rubio RM, Silva LM, et al. Leucocyte-derived extracellular trap formation significantly contributes to Haemonchus contortus larval entrapment. Parasit Vectors. 2015;8:607.
Munoz-Caro T, Conejeros I, Zhou E, et al. Dirofilaria immitis microfilariae and third-stage larvae induce canine NETosis resulting in different types of neutrophil extracellular traps. Front Immunol. 2018;9:968.
Schulz M, Zambrano F, Schuppe HC, et al. Determination of leucocyte extracellular traps (ETs) in seminal fluid (ex vivo) in infertile patients-a pilot study. Andrologia. 2019;51(9). https://doi.org/10.1111/and.13356.
Schulz M, Zambrano F, Schuppe HC, et al. Monocyte-derived extracellular trap (MET) formation induces aggregation and affects motility of human spermatozoa in vitro. Syst Biol Reprod Med. 2019;65(5):357–66. https://doi.org/10.1080/19396368.2019.1624873.
World Health Organization. WHO laboratory manual for the examination and processing of human semen. Geneva: WHO Press; 2010.
Wolff H, Panhans A, Zebhauser M, Meurer M. Comparison of three methods to detect white blood cells in semen: leukocyte esterase dipstick test, granulocyte elastase enzymeimmunoassay, and peroxidase cytochemistry. Fertil Steril. 1992;58(6):1260–2.
Cooper TG, Yeung CH, Nashan D, Jockenhovel F, Nieschlag E. Improvement in the assessment of human epididymal function by the use of inhibitors in the assay of alpha-glucosidase in seminal plasma. Int J Androl. 1990;13(4):297–305.
Gonzales GF, Villena A. True corrected seminal fructose level: a better marker of the function of seminal vesicles in infertile men. Int J Androl. 2001;24(5):255–60.
Neumann S, Gunzer G, Hennrich N, Lang H. “PMN-elastase assay”: enzyme immunoassay for human polymorphonuclear elastase complexed with alpha 1-proteinase inhibitor. J Clin Chem Clin Biochem. 1984;22(10):693–7.
Lange MK, Penagos-Tabares F, Munoz-Caro T, et al. Gastropod-derived haemocyte extracellular traps entrap metastrongyloid larval stages of Angiostrongylus vasorum, Aelurostrongylus abstrusus and Troglostrongylus brevior. Parasit Vectors. 2017;10(1):50.
Knopf J, Leppkes M, Schett G, Herrmann M, Munoz LE. Aggregated NETs sequester and detoxify extracellular histones. Front Immunol. 2019;10:2176.
Alghamdi AS, Foster DN. Seminal DNase frees spermatozoa entangled in neutrophil extracellular traps. Biol Reprod. 2005;73(6):1174–81.
Alghamdi AS, Lovaas BJ, Bird SL, Lamb GC, Rendahl AK, Taube PC, et al. Species-specific interaction of seminal plasma on sperm-neutrophil binding. Anim Reprod Sci. 2009;114(4):331–44.
Eggert-Kruse W, Zimmermann K, Geissler W, Ehrmann A, Boit R, Strowitzki T. Clinical relevance of polymorphonuclear (PMN-) elastase determination in semen and serum during infertility investigation. Int J Androl. 2009;32(4):317–29.
Parzy E, Bouchaud V, Massot P, Voisin P, Koonjoo N, Moncelet D, et al. Overhauser-enhanced MRI of elastase activity from in vitro human neutrophil degranulation. PLoS One. 2013;8(2):e57946.
Rajeeve K, Das S, Prusty BK, Rudel T. Chlamydia trachomatis paralyses neutrophils to evade the host innate immune response. Nat Microbiol. 2018;3(7):824–35.
Yu Y, Kwon K, Pieper R. Detection of neutrophil extracellular traps in urine. Methods Mol Biol. 2019;2021:241–57.
Munoz-Caro T, Mena Huertas SJ, Conejeros I, et al. Eimeria bovis-triggered neutrophil extracellular trap formation is CD11b-, ERK 1/2-, p38 MAP kinase- and SOCE-dependent. Vet Res. 2015;46:23.
Hahn S, Giaglis S, Hoesli I, Hasler P. Neutrophil NETs in reproduction: from infertility to preeclampsia and the possibility of fetal loss. Front Immunol. 2012;3:362.
Haidl G, Allam JP, Schuppe HC. Chronic epididymitis: impact on semen parameters and therapeutic options. Andrologia. 2008;40(2):92–6.
Xin S, Hao Y, Zhi-Peng M, Nanhe L, Bin C. Chronic epididymitis and leptin and their associations with semen characteristics in men with infertility. Am J Reprod Immunol. 2019;82(1):e13126.
Furuya R, Takahashi S, Furuya S, Kunishima Y, Takeyama K, Tsukamoto T. Is seminal vesiculitis a discrete disease entity? Clinical and microbiological study of seminal vesiculitis in patients with acute epididymitis. J Urol. 2004;171(4):1550–3.
Okamura N, Tajima Y, Ishikawa H, Yoshii S, Koiso K, Sugita Y. Lowered levels of bicarbonate in seminal plasma cause the poor sperm motility in human infertile patients. Fertil Steril. 1986;45(2):265–72.
Marconi M, Pilatz A, Wagenlehner F, Diemer T, Weidner W. Impact of infection on the secretory capacity of the male accessory glands. Int Braz J Urol. 2009;35(3):299–308 discussion 308–299.
Funding
This work was funded by the Institute of Parasitology, Justus Liebig University Giessen, Germany. FZ was a recipient of a post-doctoral scholarship financed by the Universidad de La Frontera, Chile.
Author information
Authors and Affiliations
Contributions
FZ, IC, MS, and PU performed the quantification of ETs and image analysis. AT, RS, and CH cooperated in research design, data analysis, and manuscript review. AP, HS, and FW cooperated in manuscript review. AP cared for the patients and controls and provided the clinical data. All the authors checked and accepted the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Ethics approval
This study was approved by the Ethics Committees of the Universidad de La Frontera and University of Giessen (Ref. N°100/7-Clinical trials: DRKS00003325). All work has been carried out in compliance with the Helsinki Declaration.
Consent to participate
Patients and controls were enrolled after signing consent.
Consent for publication
Not applicable for that section.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Zambrano, F., Schulz, M., Pilatz, A. et al. Increase of leucocyte-derived extracellular traps (ETs) in semen samples from human acute epididymitis patients—a pilot study. J Assist Reprod Genet 37, 2223–2231 (2020). https://doi.org/10.1007/s10815-020-01883-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10815-020-01883-7