Abstract
Purpose
The aim of this study was to investigate blood flow changes in the temporal and nasal short posterior ciliary arteries (SPCAs) in pseudoexfoliation syndrome using color Doppler ultrasonography.
Methods
This prospective clinical study included 67 eyes of 53 patients scheduled for cataract surgery. Pseudophakic eyes, eyes with traumatic cataract, were excluded. The demographic characteristic of the patients were recorded. Ocular blood flow was measured using 6–10 MHz Doppler ultrasound. Peak systolic velocity (PSV), end-diastolic velocity (EDV), mean flow velocity (Vm), and resistive index (RI) in the temporal and nasal SPCAs were determined for 39 eyes of 30 patients with pseudoexfoliation syndrome and cataract and a control group comprising 28 eyes of 23 patients with senile cataract.
Results
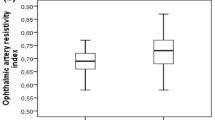
Compared to the control group, patients with pseudoexfoliation syndrome had significantly lower PSV (8.85 ± 2.88 cm/s), EDV (3.21 ± 1.12 cm/s), and Vm (5.27 ± 1.98 cm/s) in the temporal SPCA (PSV P = .001; EDV P = .002; Vm P = .001). There was no difference in velocities in the nasal SPCA. RI of both the temporal and nasal SPCA did not differ statistically between the groups (temporal SPCA P = .517, nasal SPCA P = .752)
Conclusion
There were significant decreases in temporal SPCA hemodynamic parameters in patients with pseudoexfoliation syndrome. These findings suggest that temporal SPCA ocular blood flow measurements have greater diagnostic value than those of the nasal SPCA.
Similar content being viewed by others
References
Sclötzer-Schrehardt U, Naumann GOH (1995) Trabecular meshwork in pseudoexfoliation syndrome with and without open angle glaucoma: a morphometric, ultrastructural study. Invest Ophthalmol Vis Sci 36:1750–1764
You QS, Xu L, Wang YX et al (2013) Pseudoexfoliation: normative data and associations: the beijing eye study 2011. Ophthalmology 120:1551–1558
Lindberg JG (1989) Clinical investigation on depigmentation of the pupillary border and translucency of the iris. Acta Ophthalmol Suppl 67:1–96
Tarkkanen A, Kivela T (2002) Lindberg and discovery of exfoliation syndrome. Acta Ophthalmol Scand 80:151–154
Schlötzer-Schrehardt U, Koca MR, Naumann GO et al (1992) Pseudoexfoliation syndrome ocular manifestation of a systemic disorder. Arch Ophthalmol 110:1752–1756
Detorakis ET, Actharapoulus KA, Dropkanaski E et al (2007) Haemodynamic evaluation of the posterior ciliary circulation in exfoliation syndrome and exfoliation glaucoma. Graefe's Arch Clin Exp Ophthalmol 245:516–521
Martinez A, Sanchez M (2008) Ocular haemodynamics in pseudoexfoliative and primary open-angle glaucoma. Eye 22:515–520
Tarkkanen A (2008) Is exfoliation syndrome a sign of systemic vascular disease? Acta Ophthalmol 86:832–836
Joos KM, Kay MD, Pillunat LE (1999) Effect of acute intraocular pressure changes on short posterior ciliary artery hemodynamics. Br J Ophthalmol 83:33–38
Dayanır V, Topaloglu A, Ozsunar Y et al (2009) Orbital blood flow parameters in unilateral pseudoexfoliation syndrome. Int Ophthalmol 29:27–32
Kocaturk T, Isıklıgil I, Uz B et al (2016) Ophthalmic artery blood flow parameters in pseudoexfoliation glaucoma. Eur J Ophthalmol 26(2):124–127
Remington LA (2012) Clinical anatomy and physiology of the visual system, 3rd edn. Elsevier, St. Louis, pp 202–217
Wolf S, Arend O, Haase A et al (1995) Retinal hemodynamics in patients with open angle glaucoma. Ger J Ophthalmol 4:279–282
Chung H, Arora S, Damji KF et al (2017) Association of pseudoexfoliation syndrome with cardiovascular and cerebrovascular disease: a systematic review and meta-analysis. Can J Ophthalmol 53(4):365–372
Vessani RM, Ritch R, Liebmann JM et al (2003) Plasma homocysteine is elevated in patients with exfoliative syndrome. Am J Ophthalmol 136:41–46
Yagci R, Gurel A, Ersoz I et al (2009) The activities of paraoxonase, xanthine oxidase, adenosine deaminase and the level of nitrite in pseudoexfoliation syndrome. Ophthalmic Res 42:155–159
Koliakos GG, Befani CD, Mikropoulos D et al (2008) Prooxidant-antioxidant balance, peroxide and catalase activity in the aqueous humour and serum of patients with exfoliation syndrome or exfoliative glaucoma. Graefes Arch Clin Exp Ophthalmol 246:1477–1483
Irkec M (2006) Exfoliation and carotid stiffness. Br J Ophthalmol 90:529–530
Visontai Z, Merisch B, Kollai M et al (2006) Increase of carotid artery stiffness and decrease in baroreflex sensitivity in exfoliation syndrome and glaucoma. Br J Ophthalmol 90:563–567
Harju M, Vesti E (2001) Blood flow of optic nerve head and peripapillary retina in exfoliation syndrome with unilateral glaucoma or ocular hypertension. Graefes Arch Clin Exp Opthalmol 239:271–277
Plange N, Kaup M, Arend O, Remky A (2006) Asymmetric visual field loss and retrobulbar haemodynamics in primary open angle glaucoma. Graefe's Arch Clin Exp Ophthalmol 244:978–983
Sekeroglu MA, İrkec M, Mocan MC et al (2011) The association of ocular blood flow with haemorheological parameters in primary open angle and exfoliative glaucoma. Acta Ophthalmol 89(5):429–430
Koukoula SC, Katsanos A, Tentes IK et al (2018) Retrobulbar hemodynamics and aqueous humour levels of endothelin-1 in exfoliation syndrome and exfoliation glaucoma. Clin Ophthalmol 12:1199–1204
Galassi F, Sodi A, Ucci F et al (2003) Ocular haemodynamics and glaucoma prognosis: a color Doppler imaging study. Arch Ophthalmol 121:1711–1715
Satılmış M, Orgül S, Doubler B et al (2003) Rate of progression of glaucoma correlates with retrobulbar circulation and intraocular pressure. Am J Ophthalmol 135:664–669
Martinez A, Sanchez M (2005) Predictive value of color Doppler imaging in prospective study of visual field progression in primer open glaucoma. Acta Ophthalmol Scand 83:716–722
Yüksel N, Karabaş VL, Arslan A (2001) Ocular hemodynamics in pseudoexfoliation syndrome and pseudoexfoliation glaucoma. Ophthalmology 108:1043–1049
Funding
None.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by Nese Çetin Dogan and Nusret Ozdemir. The first draft of the manuscript was written by Nese Çetin Dogan, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethics approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Ethics Committee of Cukurova University (10.2007/No 9).
Informed consent
Informed consent was obtained from all individual participants included in the study. Approval was obtained from the ethics committee of Cukurova University. The procedures used in this study adhere to the tenets of the Declaration of Helsinki.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Cetin Doğan, N., Ozdemir, N., Aikimbaev, K. et al. Hemodynamics of the temporal and nasal short posterior ciliary arteries in pseudoexfoliation syndrome. Int Ophthalmol 41, 335–340 (2021). https://doi.org/10.1007/s10792-020-01586-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10792-020-01586-z