Abstract
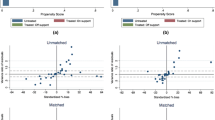
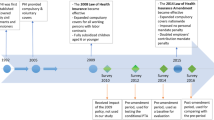
Despite subsidized health insurance has long been proclaimed by many countries including Indonesia, the variety of evaluation results showing that the optimization of benefits obtained by recipients is still questionable. The objective of this study is to analyze the impact of subsidized health insurance programs (ASKESKIN and JAMKESMAS) on the utilization of healthcare facilities in Indonesia. Data from two waves longitudinal data, the Indonesian Family Life Survey (IFLS), were analyzed using the propensity score matching method. This study found that in general, ASKESKIN and JAMKESMAS had very small impacts on the utility of healthcare facilities measured by outpatient and inpatient visits by program’s beneficiaries. It implies that being subsidized health insurance holders does not necessarily encourage them to visit formal healthcare facilities. In addition, the comparison of average treatment effect on the treated (ATT) between ASKESKIN and JAMKESMAS also did not show any significant improvement even though the program had tried to be improved. The results of this study provide the basis for advising policy makers that there needs to revisit the effectiveness of subsidized health insurance program implementation.

Similar content being viewed by others
References
Acharya, A., Vellakkal, S., Taylor, F., Masset, E., Satija, A., Burke, M., & Ebrahim, S. (2013). The impact of health insurance schemes for the informal sector in low-and middle-income countries: A systematic review. World Bank Research Observer, 28(2), 236–266. https://doi.org/10.1093/wbro/lks009
BPJS (2016). Info BPJS Kesehatan.Info BPJS,1–71
Brooks, M. I., Thabrany, H., Fox, M. P., Wirtz, V. J., Feeley, F. G., & Sabin, L. L. (2017). Health facility and skilled birth deliveries among poor women with Jamkesmas health insurance in Indonesia: a mixed-methods study. BMC Health Services Research, 17(1), 1–12. https://doi.org/10.1186/s12913-017-2028-3
Dalinjong, P. A., Welaga, P., Akazili, J., Kwarteng, A., Bangha, M., Oduro, A. … Goudge, J. (2017). The association between health insurance status and utilization of health services in rural Northern Ghana: Evidence from the introduction of the National Health Insurance Scheme. Journal of Health, Population and Nutrition, 36(1), 1–10. https://doi.org/10.1186/s41043-017-0128-7
Evans, D. B., Hsu, J., & Boerma, T. (2013). Universal health coverage and universal access. Bulletin of the World Health Organization, 91(8), 10–11. https://doi.org/10.2471/BLT.13.125450
Johar, M. (2009). The impact of the Indonesian health card program: A matching estimator approach. Journal of Health Economics, 28(1), 35–53. https://doi.org/10.1016/J.JHEALECO.2008.10.001
Khandker, R., Gayatri, S. B., S., & Hussain, A. (2010). K. Handbook on Impact. In Learning (Vol. 1, Issue 1)
Liu, H., & Zhao, Z. (2014). Does health insurance matter? Evidence from China’s urban resident basic medical insurance. Journal of Comparative Economics, 42(4), 1007–1020. https://doi.org/10.1016/j.jce.2014.02.003
Makhloufi, K., Ventelou, B., & Abu-Zaineh, M. (2015). Have health insurance reforms in Tunisia attained their intended objectives? International Journal of Health Economics and Management, 15(1), 29–51. https://doi.org/10.1007/s10754-014-9157-6
Poteliene, S., & Tamasauskiene, Z. (2014). Žmogiškojo Kapitalo Konceptualizacija: Raida, Samprata Ir Formavimas. Business Systems & Economics, 4(1), 89–106. https://doi.org/10.13165/vse-14-4-1-08
Prinja, S., Bahuguna, P., Gupta, I., Chowdhury, S., & Trivedi, M. (2019). Role of insurance in determining utilization of healthcare and financial risk protection in India. PLoS ONE, 14(2), 1–16. https://doi.org/10.1371/journal.pone.0211793
Raza, W., Poel, E., Van De, Bedi, A., Rutten, F., & Impact of community-based health insurance on access and financial protection: evidence from three randomized control trials in rural India. (2008). Health Economics, 1131(2007), 1127–1131. https://doi.org/10.1002/hec
Riuz, F., Amaya, L., & Venegas, S. (2008). Progressive segmented health insurance: Colombian health reform and access to health services. Health Economics, 1131(2007), 1127–1131. https://doi.org/10.1002/hec
Sisira Kumara, A., & Samaratunge, R. (2019). Health insurance ownership and its impact on healthcare utilization: Evidence from an emerging market economy with a free healthcare policy. International Journal of Social Economics, 47(2), 244–267. https://doi.org/10.1108/IJSE-05-2019-0333
Sparrow, R., Suryahadi, A., & Widyanti, W. (2013). Social health insurance for the poor: Targeting and impact of Indonesia’s Askeskin programme. Social Science and Medicine, 96, 264–271. https://doi.org/10.1016/j.socscimed.2012.09.043
Strauss, J., Witoelar, F., & Sikoki, B. (2016). The Fifth Wave of the Indonesia Family Life Survey: Overview and Field Report: Volume 1. The Fifth Wave of the Indonesia Family Life Survey: Overview and Field Report: Volume 1. https://doi.org/10.7249/wr1143.1
Tilahun, H., Atnafu, D. D., Asrade, G., Minyihun, A., & Alemu, Y. M. (2018). Factors for healthcare utilization and effect of mutual health insurance on healthcare utilization in rural communities of South Achefer Woreda, North West, Ethiopia. Health Economics Review, 8(1), 15 https://doi.org/10.1186/s13561-018-0200-z PMID: 30136052; PMCID: PMC6104411
Trujillo, A. J., Portillo, J. E., & Vernon, J. A. (2005). The impact of subsidized health insurance for the poor: Evaluating the colombian experience using propensity score matching. International Journal of Health Care Finance and Economics, 5(3), 211–239. https://doi.org/10.1007/s10754-005-1792-5
Wagstaff, A. (2007). Health insurance for the poor: initial impacts of Vietnam’s health care fund for the poor. World Bank Policy Research Working Paper, No.4134(March 2007), 1–33. https://doi.org/10.1596/1813-9450-4134
Wang, W., Temsah, G., & Mallick, L. (2017). The impact of health insurance on maternal health care utilization: Evidence from Ghana, Indonesia and Rwanda. Health Policy and Planning, 32(3), 366–375. https://doi.org/10.1093/heapol/czw135
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Astuti, R.D., Nugrohowati, R.N.I. Impact evaluation of subsidized health insurance programs on utilization of healthcare facilities: evidence from Indonesia. Int J Health Econ Manag. 22, 315–331 (2022). https://doi.org/10.1007/s10754-021-09321-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10754-021-09321-6