Abstract
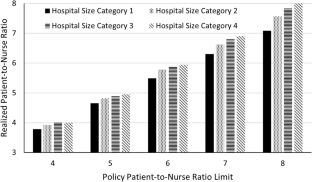
We consider the problem of setting appropriate patient-to-nurse ratios in a hospital, an issue that is both complex and widely debated. There has been only limited effort to take advantage of the extensive empirical results from the medical literature to help construct analytical decision models for developing upper limits on patient-to-nurse ratios that are more patient- and nurse-oriented. For example, empirical studies have shown that each additional patient assigned per nurse in a hospital is associated with increases in mortality rates, length-of-stay, and nurse burnout. Failure to consider these effects leads to disregarded potential cost savings resulting from providing higher quality of care and fewer nurse turnovers. Thus, we present a nurse staffing model that incorporates patient length-of-stay, nurse turnover, and costs related to patient-to-nurse ratios. We present results based on data collected from three participating hospitals, the American Hospital Association (AHA), and the California Office of Statewide Health Planning and Development (OSHPD). By incorporating patient and nurse outcomes, we show that lower patient-to-nurse ratios can potentially provide hospitals with financial benefits in addition to improving the quality of care. Furthermore, our results show that higher policy patient-to-nurse ratio upper limits may not be as harmful in smaller hospitals, but lower policy patient-to-nurse ratios may be necessary for larger hospitals. These results suggest that a “one ratio fits all” patient-to-nurse ratio is not optimal. A preferable policy would be to allow the ratio to be hospital-dependent.









Similar content being viewed by others
Data Availability
The AHA and OSHPD data are publicly available.
References
Agency for Healthcare Research and Quality (2016) Access and disparities in access to health care. Rockville, MD. https://archive.ahrq.gov/research/findings/nhqrdr/nhqdr15/access.html. Accessed 15 Sept 2022
Aiken LH, Clarke SP, Sloane DM, Lake ET, Cheney T (2008) Effects of hospital care environment on patient mortality and nurse outcomes. J Nurs Adm 38(5):223–229
Aiken LH, Clarke SP, Sloane DM, Sochalski J, Silber JH (2002) Hospital nurse staffing and patient mortality, nurse burnout, and job dissatisfaction. J Am Med Assoc 288(16):1987–1993
Aiken LH, Sloane DM, Bruyneel L, Van den Heede K, Griffiths P, Busse R, Diomidous M, Kinnunen J, Kózka M, Lesaffre E, McHugh MD, Moreno-Casbas MT, Rafferty AM, Schwendimann R, Scott PA, Tishelman C, van Achterberg T, Sermeus W (2014) Nurse staffing and education and hospital mortality in nine European countries: A retrospective observational study. The Lancet 383(9931):1824–1830
Aiken LH, Sloane DM, Cimiotti JP, Clarke SP, Flynn L, Seago JA, Spetz J, Smith HL (2010) Implications of the California nurse staffing mandate for other states. Health Serv Res 45(4):904–921
Aiken LH, Sloane DM, Griffiths P, Rafferty AM, Bruyneel L, McHugh M, Maier CB, Moreno-Casbas T, Ball JE, Ausserhofer D, Sermeus W (2017) Nursing skill mix in European hospitals: cross-sectional study of the association with mortality, patient ratings, and quality of care. BMJ Qual Saf 26:559–568
Aiken LH, Sermeus W, Van den Heede K, Sloane DM, Busse R, McKee M, Bruyneel L, Rafferty AM, Griffiths P, Moreno-Casbas MT, Tishelman C, Scott A, Mrzostek T, Kinnunen J, Schwendimann R, Heinen M, Zikos D, Sjetne IS, Smith HL, Kutney-Lee A (2012) Patient safety, satisfaction, and quality of hospital care: Cross sectional surveys of nurses and patients in 12 countries in Europe and the United States. BMJ 344:e1717
Aiken LH, Xue Y, Clarke SP, Sloane DM (2007) Supplemental nurse staffing in hospitals and quality of care. J Nurs Adm 37(7–8):335–342
Ang BY, Lam SWS, Pasupathy Y, Ong MEH (2018) Nurse workforce scheduling in the emergency department: a sequential decision support system considering multiple objectives. J Nurs Manag 26(4):432–441
Bae SH, Mark B, Fried B (2010) Use of temporary nurses and nurse and patient safety outcomes in acute care hospital units. Health Care Manage Rev 35(4):333–344
Ball JE, Bruyneel L, Aiken LH, Sermeus W, Sloane DM, Rafferty AM, Lindqvist R, Tishelman C, Griffiths P (2018) Post-operative mortality, missed care and nurse staffing in nine countries: across-sectional study. Int J Nurs Stud 78:10–15
Benzaid M, Lahrichi N, Rousseau LM (2020) Chemotherapy appointment scheduling and daily outpatient–nurse assignment. Health Care Manag Sci 23(1):34–50
Bond C., Raehl CL, Pitterle ME, Franke T (1999) Health care professional staffing, hospital characteristics, and hospital mortality rates. Pharmacother: J Human Pharmacol Drug Ther 19(2):130–138
Bretthauer KM, Heese HS, Pun H, Coe E (2011) Blocking in healthcare operations: A new heuristic and an application. Prod Oper Manag 20(3):375–391
Brooks Carthon JM, Hatfield L, Brom H, Houton M, Kelly-Hellyer E, Schlak A, Aiken LH (2021) System-level improvements in work environments lead to lower nurse burnout and higher patient satisfaction. J Nurs Care Qual 36(1):7–13
Bureau of Labor Statistics, U.S. Department of Labor (2022) Occupational outlook handbook, registered nurses. http://www.bls.gov/ooh/healthcare/registered-nurses.htm. Accessed 15 Sept 2022
Burke EK, Curtois T (2014) New approaches to nurse rostering benchmark instances. Eur J Oper Res 237(1):71–81
Campbell GM (1999) Cross-utilization of workers whose capabilities differ. Manage Sci 45(5):722–732
Chang AM, Cohen D, Lin A, Augustine J, Handel D, Howell E, Kim H, Pines J, Schuur JD, McConnell KJ, Sun BC (2018) Hospital strategies for reducing emergency department crowding: a mixed-methods study. Ann Emerg Med 71(4):497-505.e4
Cheang B, Li H, Lim A, Rodrigues B (2003) Nurse rostering problems––a bibliographic survey. Eur J Oper Res 151(3):447–460
Chhatwal J, Alagoz O, Burnside ES (2010) Optimal breast biopsy decision-making based on mammographic features and demographic factors. Oper Res 58(6):1577–1591
Cho D, Cattani K (2019) The patient patient: the performance of traditional versus open-access scheduling policies. Decis Sci 50(4):756–785
Cho E, Sloane DM, Kim EY, Kim S, Choi M, Yoo IY, Lee HS, Aiken LH (2015) Effects of nurse staffing, work environments, and education on patient mortality: An observational study. Int J Nurs Stud 52(2):535–542
Cho SH, Ketefian S, Barkauskas VH, Smith DG (2003) The effects of nurse staffing on adverse events, morbidity, mortality, and medical costs. Nurs Res 52(2):71–79
Dall TM, Chen YJ, Seifert RF, Maddox PJ, Hogan PF (2009) The economic value of professional nursing. Med Care 47(1):97–104
Daskin MS, Dean LK (2005) Location of health care facilities. Operations research and health care: a handbook of methods and applications. In: Brandeau M, Sainfort F, Pierskalla WP (eds). Kluwer Academic Publishers. Chapter 3, pp 43–76
De Véricourt F, Jennings OB (2011) Nurse staffing in medical units: a queueing perspective. Oper Res 59(6):1320–1331
Denton BT, Miller AJ, Balasubramanian HJ, Huschka TR (2010) Optimal allocation of surgery blocks to operating rooms under uncertainty. Oper Res 58(4):802–816
Dobson G, Hasija S, Pinker EJ (2011) Reserving capacity for urgent patients in primary care. Prod Oper Manag 20(3):456–473
Dobson G, Lee HH, Pinker E (2010) A model of ICU bumping. Oper Res 58(6):1564–1576
Dobson G, Pinker E, Van Horn RL (2009) Division of labor in medical office practices. Manuf Serv Oper Manag 11(3):525–537
Easton FF (2011) Cross-training performance in flexible labor scheduling environments. IIE Transaction 43(8):589–603
Faridimehr S, Venkatachalam S, Chinnam RB (2021) Managing access to primary care clinics using scheduling templates. Health Care Manag Sci 24(3):482–498
Fagerström L, Kinnunen M, Saarela J (2018) Nursing workload, patient safety incidents and mortality: an observational study from Finland. BMJ Open 8(e016367):1–10
Gnanlet A, Gilland WG (2009) Sequential and simultaneous decision making for optimizing health care resource flexibilities. Decis Sci 40(2):295–326
Gnanlet A, Gilland WG (2014) Impact of productivity on cross-training configurations and optimal staffing decisions in hospitals. Eur J Oper Res 238(1):254–269
Green, L.V. (2005). Capacity Planning and Management in Hospitals. In: Brandeau, M.L., Sainfort, F., Pierskalla, W.P. (eds) Operations Research and Health Care. International Series in Operations Research & Management Science, vol 70. Springer, Boston, MA. pp 15-41
Green LV, Savin S (2008) Reducing delays for medical appointments: A queueing approach. Oper Res 56(6):1526–1538
Griffiths P, Ball J, Bloor K, Böhning D, Briggs J, Dall’Ora C, De Iongh A, Jones J, Kovacs C, Maruotti A, Meredith P, Prytherch D, Saucedo AR, Redfern O, Schmidt P, Sinden N, Smith G (2018) Nurse staffing levels, missed vital signs and mortality in hospitals: Retrospective longitudinal observational study. Health Serv Deliv Res 6(38)
Gupta D, Denton B (2008) Appointment scheduling in health care: Challenges and opportunities. IIE Transaction 40(9):800–819
Gurses AP, Carayon P, Wall M (2009) Impact of performance obstacles on intensive care nurses’ workload, perceived quality and safety of care, and quality of working life. Health Serv Res 44(2p1):422–443
Halawa F, Madathil SC, Gittler A, Khasawneh MT (2020) Advancing evidence-based healthcare facility design: A systematic literature review. Health Care Manag Sci 23(3):453–480
Halm EA, Lee C, Chassin MR (2002) Is volume related to outcome in health care? A systematic review and methodologic critique of the literature. Ann Intern Med 137(6):511–520
Hopp WJ, Tekin E, Van Oyen MP (2004) Benefits of skill chaining in serial production lines with cross-trained workers. Manage Sci 50(1):83–98
Hugonnet S, Chevrolet J, Pittet D (2007) The effect of workload on infection risk in critically ill patients. Crit Care Med 35(1):76–81
Institute of Medicine (2001) Crossing the quality chasm: a new health system for the 21st century. National Academies Press, Washington D.C
Iwashyna TJ, Kramer AA, Kahn JM (2009) Intensive care unit occupancy and patient outcomes. Crit Care Med 37(5):1545–1557
Jones CB (2005) The costs of nurse turnover, part 2: application of the nursing turnover cost calculation methodology. J Nurs Adm 35(1):41–49
Jordan WC, Inman RR, Blumenfeld DE (2004) Chained cross-training of workers for robust performance. IIE Trans 36(10):953–967
Kahn JM, Goss CH, Heagerty PJ, Kramer AA, O’Brien CR, Rubenfeld GD (2006) Hospital volume and the outcomes of mechanical ventilation. N Engl J Med 355(1):41–50
Kanai Y, Takagi H (2021) Markov chain analysis for the neonatal inpatient flow in a hospital. Health Care Manag Sci 24(1):92–116
Kane RL, Shamliyan TA, Mueller C, Duval S, Wilt TJ (2007) The association of registered nurse staffing levels and patient outcomes: systematic review and meta-analysis. Med Care 45(12):1195–1204
Kosel K, Olivo T (2002) The business case for workforce stability. VHA Research Series 7:1–16
Lankshear AJ, Sheldon TA, Maynard A (2005) Nurse staffing and healthcare outcomes: a systematic review of the international research evidence. Adv Nurs Sci 28(2):163–174
Lee DKK, Zenios SA (2009) Optimal capacity overbooking for the regular treatment of chronic conditions. Oper Res 57(4):852–865
Legrain A, Omer J, Rosat S (2020) An online stochastic algorithm for a dynamic nurse scheduling problem. Eur J Oper Res 285(1):196–210
Lim GJ, Mobasher A, Côté MJ (2012) Multi-objective nurse scheduling models with patient workload and nurse preferences. Management 2(5):149–160
Lin H (2014) Revisiting the relationship between nurse staffing and quality of care in nursing homes: An instrumental variables approach. J Health Econ 37:13–24
Lin YK, Chou YY (2020) A hybrid genetic algorithm for operating room scheduling. Health Care Manag Sci 23(2):249–263
Lopez V, Anderson J, West S, Cleary M (2022) Does the COVID-19 pandemic further impact nursing shortages? Issues Ment Health Nurs 43(3):293–295
Ma C, McHugh MD, Aiken LH (2015) Organization of hospital nursing and 30-day readmissions in Medicare patients undergoing surgery. Med Care 53(1):65–70
Mandelbaum A, Momcilovic P, Tseytlin Y (2012) On fair routing from emergency departments to hospital wards: QED queues with heterogeneous servers. Manage Sci 58(7):1273–1291
May JH, Spangler WE, Strum DP, Vargas LG (2011) The surgical scheduling problem: Current research and future opportunities. Prod Oper Manag 20(3):392–405
McCue M, Mark BA, Harless DW (2003) Nurse staffing, quality, and financial performance. J Health Care Finance 29(4):54–76
Mousavi H, Darestani SA, Azimi P (2021) An artificial neural network based mathematical model for a stochastic health care facility location problem. Health Care Manag Sci 24(3):499–514
Musy SN, Endrich O, Leichtle AB, Griffiths P, Nakas CT, Simon M (2020) Longitudinal study of the variation in patient turnover and patient-to-nurse ratio: Descriptive analysis of a Swiss University Hospital. J Med Internet Res 22(4):e15554
Needleman J, Buerhaus P, Mattke S, Stewart M, Zelevinsky K (2002) Nurse-staffing levels and the quality of care in hospitals. N Engl J Med 346(22):1715–1722
Needleman J, Buerhaus P, Pankratz VS, Leibson CL, Stevens SR, Harris M (2011) Nurse staffing and inpatient hospital mortality. N Engl J Med 364(11):1037–1045
Needleman J, Buerhaus PI, Stewart M, Zelevinsky K, Mattke S (2006) Nurse staffing in hospitals: Is there a business case for quality? Health Aff 25(1):204–211
Newhouse RP, Johantgen M, Pronovost PJ, Johnson E (2005) Perioperative nurses and patient outcomes—mortality, complications, and length of stay. AORN J 81(3):508–528
NSI Nursing Solutions, Inc. (2021) 2021 NSI national health care retention & rn staffing report. https://www.emergingrnleader.com/wp-content/uploads/2021/04/NSI_National_Health_Care_Retention_Report.pdf. Accessed 12 Mar 2023
Oakley D, Onggo BS, Worthington D (2020) Symbiotic simulation for the operational management of inpatient beds: model development and validation using Δ-method. Health Care Manag Sci 23(1):153–169
OECD/European Union (2014) Health at a glance: Europe 2014. OECD Publishing. https://doi.org/10.1787/health_glance_eur-2014-en
Olivares M, Terwiesch C, Cassorla L (2008) Structural estimation of the newsvendor model: an application to reserving operating room time. Manage Sci 54(1):41–55
Papanicolas I, Woskie LR, Jha AK (2018) Health care spending in the United States and other high-income countries. JAMA 319(10):1024–1039
Peelen L, de Keizer N, Peek N, Jan Scheffer G, van der Voort P, de Jonge E (2007) The influence of volume and intensive care unit organization on hospital mortality in patients admitted with severe sepsis: a retrospective multicentre cohort study. Crit Care 11(2):1–10
Phibbs C, Bartel A, Giovannetti B, Schmitt S, Stone P (2009) The impact of nurse staffing and contract nurses on patient outcomes: New evidence from longitudinal data. Working Paper, Columbia Business School
Phibbs CS, Baker LC, Caughey AB, Danielsen B, Schmitt SK, Phibbs RH (2007) Level and volume of neonatal intensive care and mortality in very-low-birth-weight infants. N Engl J Med 356(21):2165–2175
Pinker EJ, Shumsky RA (2000) The efficiency-quality trade-off of cross-trained workers. Manuf Serv Oper Manag 2(1):32–48
Pronovost PJ, Dang D, Dorman T, Lipsett PA, Garrett E, Jenckes M, Bass EB (2001) Intensive care unit nurse staffing and the risk for complications after abdominal aortic surgery. Eff Clin Pract 4(5):199–206
Rauner MS, Gutjahr WJ, Heidenberger K, Wagner J, Pasia J (2010) Dynamic policy modeling for chronic diseases: Metaheuristic-based identification of pareto-optimal screening strategies. Oper Res 58(5):1269–1286
Rerkjirattikal P, Huynh VN, Olapiriyakul S, Supnithi T (2020) A goal programming approach to nurse scheduling with individual preference satisfaction. Math Probl Eng 2020:2379091
Rothberg MB, Abraham I, Lindenauer PK, Rose DN (2005) Improving nurse-to-patient staffing ratios as a cost-effective safety intervention. Med Care 43(8):785–791
Schoenfelder J, Bretthauer KM, Wright PD, Coe E (2020) Nurse scheduling with quick-response methods: Improving hospital performance, nurse workload, and patient experience. Eur J Oper Res 283(1):390–403
Shehadeh KS, Padman R (2021) A distributionally robust optimization approach for stochastic elective surgery scheduling with limited intensive care unit capacity. Eur J Oper Res 290(3):901–913
Silber JH, Rosenbaum PR, McHugh MD, Ludwig JM, Smith HL, Niknam BA, Even-Shoshan O, Fleisher LA, Kelz RR, Aiken LH (2016) Comparison of the value of nursing work environments in hospitals across different levels of patient risk. JAMA Surg 151(6):527–536
Sims CE (2003) Increasing clinical, satisfaction, and financial performance through nurse-driven process improvement. J Nurs Adm 33(2):68–75
Sloane DM, Smith HL, McHugh MD, Aiken LH (2018) Effect of changes in hospital nursing resources on improvements in patient safety and quality of care: a panel study. Med Care 56(12):1001–1008
Spence Laschinger HK, Leiter MP (2006) The impact of nursing work environments on patient safety outcomes: the mediating role of burnout engagement. J Nurs Adm 36(5):259–267
Spetz J (2004) California’s minimum nurse-to-patient ratios: the first few months. J Nurs Adm 34(12):571–578
Stanton MW, Rutherford MK (2004) Hospital nurse staffing and quality of care. Research in Action, Issue 14. Agency for Healthcare Research and Quality, Rockville, Maryland
Sturm H, Rieger MA, Martus P, Ueding E, Wagner A, Holderried M, Maschmann J (2019) Do perceived working conditions and patient safety culture correlate with objective workload and patient outcomes: A cross-sectional explorative study from a German university hospital. Plos One 14(1):e0209487 (1-19)
Theokary C, Ren ZJ (2011) An empirical study of the relations between hospital volume, teaching status, and service quality. Prod Oper Manag 20(3):303–318
Thompson S, Nunez M, Garfinkel R, Dean MD (2009) OR practice–-Efficient short-term allocation and reallocation of patients to floors of a hospital during demand surges. Oper Res 57(2):261–273
Tourangeau AE, Doran DM, Hall LMG, O’Brien Pallas L, Pringle D, Tu JV, Cranley LA (2007) Impact of hospital nursing care on 30-day mortality for acute medical patients. J Adv Nurs 57(1):32–44
Tsai SC, Yeh Y, Kuo CY (2021) Efficient optimization algorithms for surgical scheduling under uncertainty. Eur J Oper Res 293(2):579–593
U.S. General Accounting Office (GAO) (2009) Hospital emergency departments: crowding continues to occur, and some patients wait longer than recommended time frames. Report GAO-09-347
Valouxis C, Gogos C, Goulas G, Alefragis P, Housos E (2012) A systematic two phase approach for the nurse rostering problem. Eur J Oper Res 219(2):425–433
Volland J, Fügener A, Schoenfelder J, Brunner JO (2017) Material logistics in hospitals: a literature review. Omega 69:82–101
Wang WY, Gupta D (2011) Adaptive appointment systems with patient preferences. Manuf Serv Oper Manag 13(3):373–389
White DL, Froehle CM, Klassen KJ (2011) The effect of integrated scheduling and capacity policies on clinical efficiency. Prod Oper Manag 20(3):442–455
Wolbeck L, Kliewer N, Marques I (2020) Fair shift change penalization scheme for nurse rescheduling problems. Eur J Oper Res 284(3):1121–1135
Wright PD, Bretthauer KM (2010) Strategies for addressing the nursing shortage: Coordinated decision making and workforce flexibility. Decis Sci 41(2):373–401
Wright PD, Bretthauer KM, Côté MJ (2006) Reexamining the nurse scheduling problem: Staffing ratios and nursing shortages. Decis Sci 37(1):39–70
Wynendaele H, Willems R, Trybou J (2019) Systematic review: Association between the patient–nurse ratio and nurse outcomes in acute care hospitals. J Nurs Manag 27(5):896–917
Yankovic N, Green LV (2011) Identifying good nursing levels: A queuing approach. Oper Res 59(4):942–955
Yu X, Bayram A (2021) Managing capacity for virtual and office appointments in chronic care. Health Care Manag Sci 24(4):742–767
Zhang X, Tai D, Pforsich H, Lin VW (2018) United States registered nurse workforce report card and shortage forecast: a revisit. Am J Med Qual 33(3):229–236
Funding
No funds, grants, or other support was received.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection, analysis, and manuscript writing were performed by David D. Cho, Kurt M. Bretthauer, and Jan Schoenfelder. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Declarations
The AHA and OSHPD data are publicly available.
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendices
Appendix A
1.1 Three case study hospitals
We collected nursing data from three hospitals in the United States. One is located in California and two are located in Indiana. They range in size from 350 to 550 beds. We obtained information on nurse wages, shift types, staff size and mix, shift preferences and availability, patient-to-nurse ratios, and limited bed demand data. Note that detailed and extensive historical patient flow and demand data were not available. Due to the limited bed demand data, we also use data from the American Hospital Association and California Office of Statewide Health Planning and Development to estimate inpatient demand and create hospital size categories, as described in the next subsection. The three hospitals differ in size and nurse wages. Table 5 summarizes the data.
1.2 American hospital association (AHA) data
In addition to the three case study hospitals, we acquired 2015 AHA Annual Survey data from California, New York, and Texas for our numerical experiments. From the dataset, we consider hospitals with the primary service code of “general medical and surgical” and that are coded as either “nongovernment, not-for-profit” or “corporation-owned, for-profit”. We exclude hospitals that do not have any general medical and surgical adult beds. After filtering, the data set contains information on 493 hospitals across the three states of California, New York, and Texas.
Based on the 2015 AHA Annual Survey data, we created four hospital size categories, as shown in Table 6. While the range of total facility inpatient days for category 3 is relatively wide, the impact of hospital size on the policy patient-to-nurse ratio is still captured effectively with the four categories, as shown by the results in Section 5.1.
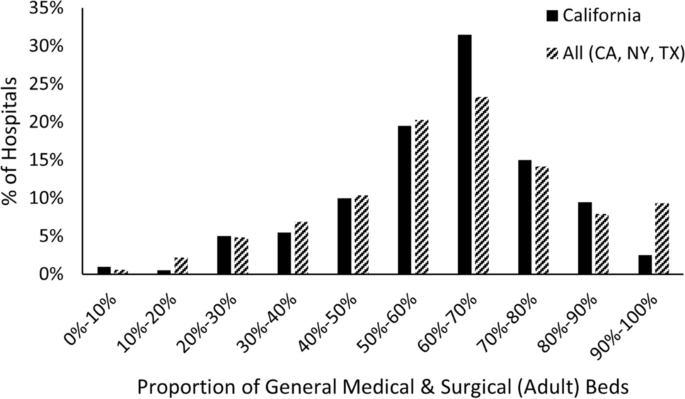
Figure 11 reports the proportion of general medical and surgical beds in the included hospitals according to the AHA data. The AHA data provides total hospital-wide inpatient days, but not unit-specific inpatient days, which is what we need. Therefore, based on Fig. 11, we estimate that the inpatient days for med/surg units are around 50–80% of the total hospital-wide inpatient days.
1.3 California office of statewide health planning and development (OSHPD) data
To further support our estimate of med/surg inpatient days, we also acquired data from the “2014–2015 Fiscal Year Hospital Annual Financial Disclosure Report” provided by California’s Office of Statewide Health Planning and Development (OSHPD). While this data set is limited to hospitals in California, it includes unit-specific information regarding beds and patient (census) days. After applying the identical filter as used for the AHA data set, the OSHPD data set provides information on 198 hospitals in California. Figure 12 shows that our assumption of inpatient days for the med/surg unit being around 50–80% of the total hospital-wide inpatient days is reasonable.
Appendix B. Limiting undesirable shifts for each nurse
In Section 5.3, we minimize the total number of undesirable shifts without incurring any additional schedule costs, but we do not limit the number of undesirable shifts for each nurse. Thus, it is theoretically possible for the remaining undesirable shifts to be assigned disproportionately to a small number of nurses. While this was not a major issue for our numerical experiments in Section 5.3 due to the very low number of remaining undesirable shifts with the second objective function, we can also add constraints (27) and (28) that limit the number of undesirable shifts along with second objective function (23).
where \({\overline{US} }_{i}^{UN}\) and \({\overline{US} }_{i}^{FN}\) are upper limits on the number of undesirable shifts assigned to unit and float nurse \(i\), respectively.
Because we still do not allow additional schedule costs, our optimal costs do not change in this case. Furthermore, we also do not observe any meaningful differences in total number of undesirable shifts compared to the results presented in Section 5.3 as long as \({\overline{US} }_{i}^{UN}\) and \({\overline{US} }_{i}^{FN}\) are not too low. We note that when the limit is too low (for example, 0 or 1 undesirable shift per nurse), the problem sometimes becomes unsolvable for policy PTN ratio of 4:1 due to the insufficient number of available and desirable shifts to stay under the policy PTN for every shift since we do not allow any increase in costs.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Cho, D.D., Bretthauer, K.M. & Schoenfelder, J. Patient-to-nurse ratios: Balancing quality, nurse turnover, and cost. Health Care Manag Sci 26, 807–826 (2023). https://doi.org/10.1007/s10729-023-09659-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10729-023-09659-y