Abstract
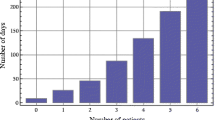
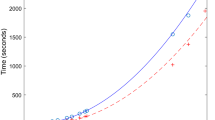
Discrete-time Markov chain and queueing-theoretic models are used to quantitatively formulate the flow of neonatal inpatients over several wards in a hospital. Parameters of the models are determined from the operational analysis of the record of the numbers of admission/departure for each ward every day and the order log of patient movement from ward to ward for two years provided by the Medical Information Department of the University of Tsukuba Hospital in Japan. Our formulation is based on the analysis of the precise routes (the route of an inpatient is defined as a sequence of the wards in which he/she stays from admission to discharge) and their length-of-stay (LoS) in days in each ward on their routes for all neonatal inpatients. Our theoretical model calculates the probability distribution for the number of patients staying in each ward per day which agrees well with the corresponding histogram observed for each ward as well as for the whole hospital. The proposed method can be used for the long-term capacity planning of hospital wards with respect to the probabilistic bed utilization.





Similar content being viewed by others
References
Adeyemi S, Chaussalet TJ, Xie H, Asaduzzaman M (2010) Random effects models for operational patient pathways. J Appl Stat 37(3):691–702
Adeyemi S, Chaussalet T, Demir E (2011) Nonproportional random effects modelling of a neonatal unit operational patient pathways. Statistical Method & Applications 20:507–518
Asaduzzaman M, Chaussalet TJ, Robertson NJ (2010) A loss network model with overflow for capacity planning of a neonatal unit. Ann Oper Res 178(1):67–76
Asaduzzaman M, Chaussalet TJ (2011) An overflow loss network model for capacity planning of a perinatal network. Journal of Royal Statistical Society. A 174(2):403–417
Asaduzzaman M, Chaussalet TJ (2014) Capacity planning of a perinatal network with generalised loss network model with overflow. Eur J Oper Res 232(1):178–183
Bai J, Fügener A, Schoenfelder J, Brunner JO (2018) Operations research in intensive care unit management: a literature review. Health Care Management Science 21(1):1–24
Baskett F, Chandy KM, Muntz MM, Palacios FG (1975) Open, closed, and mixed networks of queues with different classes of customers. J Assoc Comput Mach 22(2):248–260
Bekker R, de Bruin AM (2010) Time-dependent analysis for refused admissions in clinical wards. Ann Oper Res 178:45–65
Bountourelis T, Ulukus MY, Kharoufeh JP, Nabors SG (2013) The modeling, analysis, and management of intensive care units. In: Denton B T (ed) Handbook of healthcare operations management: methods and applications, springer:, pp 153–182
Brahimi M, Worthington DJ (1991) Queueing models for out-patient appointment systems – a case study. Journal of the Operational Research Society 42(9):733–746
Brandeau ML, Sainfort F, Pierskalla WP (eds) (2004) Operations Research and Health care: A Handbook of Methods and Applications Kluwer Academic Publishers
de Bruin AM, van Rossum AC, Visser MC, Koole GM (2007) Modeling the emergency cardiac in-patient flow: an application of queueing theory. Health Care Management Science 10(2):125–137
de Bruin AM, Bekker R, van Zanten L, Koole GM (2010) Dimensioning hospital wards using the Erlang loss model. Annals of Operations Research 178:23–43
Cohen MA, Hershey JC, Weiss EN (1980) Analysis of capacity decisions for progressive patient care hospital facilities. Health Serv Res 15:145–160
Côté M J, Stein WE (2007) A stochastic model for a visit to the doctor’s office. Math Comput Model 45:309–323
Creemers S, Lambrecht M (2011) Modeling a hospital queueing network. In: Boucherie R J, van Dijk N M (eds) Queueing networks: a fundamental approach, Springer, pp 767–798
Dai JG, Shi P (2019) Inpatient overflow: An approximate dynamic programming approach. Manufacturing & Service Operations Management Published Online: 16 May
Dai T, Tayur S (eds) (2018) Handbook of Healthcare analytics: Theoretical Minimum for Conducting 21st Century Research on Healthcare Operations, John Wiley & Sons. Hoboken, New Jersey
Demir E, Lebcir R, Adeyemi S (2014) Modelling length of stay and patient flows: methodological case studies from the UK neonatal care services. Journal of the Operational Research Societies 65(4):532–545
Denning PE, Buzen JP (1978) The operational analysis of queueing network models. ACM Comput Surv 10(3):225–261
Denton BT (ed) (2013) Handbook of Healthcare Operations management: Methods and Applications Springer
Faddy MJ, McClean SI (1999) Analysing data on lengths of stay of hospital patients using phase-type distributions. Appl Stoch Model Bus Ind 15(4):311–317
Gorunescu F, McClean SI, Millard PH (2002) Using a queueing model to help plan bed allocation in a department of geriatric medicine. Health Care Management Science 5(4):307– 312
Green L (2004) Capacity planning and management in hospitals. In: Brandeau M L, Sainfort F, Pierskalla W P (eds) Operations research and health care: A handbook of methods and applications, kluwer:, pp 15–41
Green L (2006) Queueing analysis in healthcare. In: Hall R W (ed) Patient flow: reducing delay in healthcare delivery, springer:, pp 281–307
Griffin J, Xia S, Peng S, Keskinocak P (2012) Improving patient flow in an obstetric unit. Health Care Management Science 15(1):1–14
Griffiths JD, Price-Lloyd N, Smithies M, Williams J (2006) A queueing model of activities in an intensive care unit. IMA J Manag Math 17(3):277–288
Gross D, Shortle JF, Thompson JM, Harris CM (2008) Fundamentals of queueing theory, 4th edn. John Wiley & Sons, Hoboken, New Jersey
Günal M M, Pidd M (2010) Discrete event simulation for performance modelling in health care: a review of the literature. Journal of Simulation 4:42–51
Gupta D (2013) Queueing models for healthcare operations. In: Denton B T (ed) Handbook of healthcare operations management: methods and applications, springer:, pp 19–44
Hall RW (1991) Queueing methods: for services and manufacturing Prentice-Hall. Englewood Cliffs, New Jersey
Hall R (ed) (2006) Patient flow: Reducing Delay in Healthcare Delivery. Springer, Boston
Hall R (ed) (2012) Handbook of Healthcare System Scheduling Springer
Hall R (2012) Bed assignment and bed management. In: Hall R (ed) Handbook of healthcare system scheduling, springer:, pp 177–200
Harris MD (2010) Little’s law: The science behind proper staffing. Emergency Physicians Monthly
Helm JE, AhmadBeygi S, Van Oyen MP (2011) Design and analysis of hospital admission control for operational effectiveness. Production and Operations Management 20(3):359–374
Hershey JC, Weiss EN, Cohen MA (1981) A stochastic service network model with application to hospital facilities. Oper Res 29(1):1–22
Heyman DP, Sobel MJ (1982) Stochastic Models in Operations Research, Volume I: Stochastic Processes and Operating Characteristics. McGraw-Hill Book Company
Irvine V, McClean S, Millard P (1994) Stochastic models for geriatric in-patient behaviour. Mathematical Medicine and Biology: A Journal of the IMA 11(3):207–216
Jacobson SH, Hall SN, Swisher JR (2006) Discrete-event simulation of health care systems. In: Hall RW (ed) Patient flow: reducing delay in healthcare delivery, springer:, pp 211–252
Jiang L, Giachetti RF (2008) A queueing network model to analyze the impact of parallelization of care on patient cycle time. Health Care Management Science 11(3):248–261
Jun JB, Jacobson SH, Swisher JR (1999) Application of discrete-event simulation in health care clinics: A survey. The Journal of the Operational Research Society 50(2):109–123
Kahraman C, Topcu YI (eds) (2018) Operations Research Applications in Health Care Management. Springer, Berlin
Kim SC, Horowitz I, Young KK, Buckley TA (1999) Analysis of capacity management of the intensive care unit in a hospital. Eur J Oper Res 115(1):36–46
Kim SH, Whitt W (2014) Are call center and hospital arrivals well modeled by nonhomogeneous Poisson processes? Manufacturing & Service Operations Management 16(3):464–480
Kleinrock L (1976) Queueing systems Volume II: computer applications. John Wiley & Sons, New York
Koizumi N, Kuno E, Smith TE (2005) Modeling patient flows using a queuing network with blocking. Health Care Management Science 8(1):49–60
Kortbeek N, van Dijk N (2007) On dimensioning intensive care units. AENORM 57:22–26
Laksmi C, Iyer SA (2013) Application of queueing theory in health care: a literature review. Operations Research for Health Care 2(1–2):25–39
Little JDC (1961) A proof for the queuing formula L = λW. Operations Research 9(3):383–387
Little JDC (2011) Little’s law as viewed on its 50th anniversary. Oper Res 59(3):536–549
Little JDC, Graves SC (2008) Little’s law. In: Chhajed D, Lowe T J (eds) Building intuition: insights from basic operations management models and principles. Springer, pp 81–100
Litvak N, van Rijsbergen M, Boucherie RJ, van Houdenhoven M (2008) Managing the overflow of intensive care patients. Eur J Oper Res 185(3):998–1010
Lovejoy WS, Desmond JS (2011) Little’s law flow analysis of observation unit impact and sizing. Acad Emerg Med 18(2):183–189
McClain JO (1976) Bed planning using queuing theory models of hospital occupancy: a sensitivity analysis. Inquiry 13(2):167–176
McClain JO (1978) A model for regional obstetric bed planning. Health Serv Res 13(4):378–394
McClean S, Millard P, El-Darzi E, Nugent CD (eds) (2009) Intelligent Patient Management. Springer, Berlin
McClean S, Millard P (1993) Patterns of length of stay after admission in geriatric medicine: an event history approach. Journal of the Royal Statistical Society Series D (The Statistician) 42(3):263–274
Mirasol NM (1963) The output of an M/G/ \(\infty \) queuing system is Poisson. Oper Res 11(2):282–284
Palvannan RK, Teow KL (2012) Queueing for healthcare. J Med Syst 36(2):541–547
Pehlivan C (2014) Design and flow control of stochastic health care networks without waiting rooms: a perinatal application. Ecole Nationale de Supérieure des Mines de Saint-Etienne, Business administration. https://tel.archives-ouvertes.fr/tel-00994291/file/Pehlivan-Canan-diff.pdf
Perros H (1994) Queueing networks with blocking. Oxford University Press, New York
Ramalhoto MF, Amaral JA, Teresa Cochito M (1983) A survey of Little’s formula. Int Stat Rev 51(3):255–278
Ridge JC, Jones SK, Nielsen MS, Shahani AK (1998) Capacity planning for intensive care units. Eur J Oper Res 105:346–355
Song H, Veeraraghaven S (2018) Quality care. In: Dai T, Tayur S (eds) Handbook of Healthcare Analytics: Theoretical Minimum for Conducting 21st Century Research on Healthcare Operations, John Wiley & Sons, New York, pp 79–108
Takagi H, Kanai Y, Misue K (2017) Queueing network model for obstetric patient flow in a hospital. Health Care Management Science 20(3):435–451
Taylor HM, Karlin S (1994) An Introduction to Stochastic Modeling. revised edition Academic Press. San Diego, California
Truong VA (2018) Inpatient care. In: Dai T, Tayur S (eds) Handbook of Healthcare Analytics: Theoretical Minimum for Conducting 21st Century Research on Healthcare Operations, John Wiley & Sons, New York, pp 243–255
Utley M, Worthington D (2012) Capacity planning. In: Hall R (ed) Handbook of healthcare system scheduling, springer:, pp 11–30
van de Vrugt NM, Schneider AJ, Zonderland ME, Stanford DA, Boucherie RJ (2018) Operations research for occupancy modeling at hospital wards and its integration into practice. In: Kahraman C, Topcu Y I (eds) Operations research applications in health care management, springer:, pp 101–137
van Dijk NM, Kortbeek N (2009) Erlang loss bounds for OT-ICU systems. Queueing Systems 63(1–4):253–280
Weiss EN, Cohen AM, Hershey JC (1982) An iterative estimation and validation procedure for specification of semi-Markov models with application to hospital patient flow. Oper Res 30(6):1082–1104
Weiss EN, McClain JO (1987) Administrative days in acute care facilities: a queueing-analytic approach. Oper Res 35(1): 35–44
Wiler JL, Griffey RT, Olsen T (2011) Review of modeling approaches for emergency department patient flow and crowding research. Acad Emerg Med 18(12):1371–1379
Xie H, Chaussalet TJ, Millard PH (2005) A continuous time Markov model for the length of stay of elderly people in institutional long-term care. Journal of the Royal Statistical Society:, Series A (Statistics in Society) 168(1):51–61
Yankovic N, Green LV (2011) Identifying good nursing levels: a queuing approach. Oper Res 59(4):942–955
Zachary S, Ziedins I (2011) Loss networks. In: Boucherie R J, van Dijk N M (eds) Queueing networks: a fundamental approach, springer:, pp 701–728
Zhang H, Best TJ, Chivu A, Meltzer DO (2020) Simulation-based optimization to improve hospital patient assignment to physicians and clinical units. Health Care Management Science 23(1):117–141
Zonderland ME, Boucherie RJ (2012) Queuing networks in healthcare systems. In: Hall R (ed) Handbook of healthcare system scheduling, springer:, pp 201–243
Acknowledgements
The order log of patient transfers used in this paper was provided to us by the University of Tsukuba Hospital (UTH) through the approval of its Research Ethics Committee. The authors are grateful to the following staff of the UTH during 2011–2013 for their support of this work: Dr. Tetsuya Igarashi, the then Director of UTH, Dr. Hiromi Hamada and Dr. Tsuyoshi Ogura of the Obstetrics and Gynecology Section, Dr. Hiroyuki Hoshimoto of the Medical Information and Medical Records, and Mr. Masaki Suzuki of the Head Division of Accounting and Management. The authors thank Editor-in-Chief of the journal and two reviewers of the original manuscript for their valuable and constructive comments as well as a list of additional references, which were very useful in revising the manuscript.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This work was partially supported by the Grant-in-Aid for Scientific Research (A) No. 23241047 from the Japan Society for the Promotion of Science (JSPS) during the fiscal years 2011–2013 for data acquisition as well as by (C) No. 17K00435 in 2017–2019 for the theoretical analysis.
Appendices
Appendix 1: Routes of neonatal patients in two groups
Numerical characteristics for the two groups of routes taken by neonatal patients are given in Table 4. A set of 12 routes of neonatal patients in Group 1 which do not pass Ward 430 are displayed in Fig. 6. The symbol λr stands for route r given in Table 4 (a), 1 ≤ r ≤ 12. A set of 10 routes of neonatal patients in Group 2 which pass Ward 430 and do not pass Ward 300 are displayed in Fig. 7. The symbol \( \lambda ^{*}_{r} \) stands for route r∗ given in Table 4 (b), 1 ≤ r∗≤ 10. Due to the complexity of these routes, Ward 500 is shown in several separate places in these figures.
The complexity of the routes may contribute to the observed independence assumption for the arrival process of patients from mixed routes in each ward mentioned in Section 6.4.
Appendix 2: Patient arrival process observed during the two years
The counted numbers of neonatal patients who are admitted to the hospital (a) in each month, (b) in each quarter, (c) on each day-of-the-week, and (d) on each lunar-calendar day during two fiscal years 2010 and 2011 are shown in Table 10. It is not appropriate to try to draw any definite conclusion about the seasonal variability from the data observed only for these two particular years. We observe that more neonatal patients are admitted in the 4th Q than in any other quarters in the fiscal year 2010, but that the least patients are admitted in the 4th Q in the fiscal year 2011. There was the Great East Japan Earthquake in the 4th Q of the fiscal year 2010 (March 11, 2011). We also observe that twice as many neonatal patients are admitted on Monday as on Sunday. There seems to be no particular dependence on the lunar calendar.
Rights and permissions
About this article
Cite this article
Kanai, Y., Takagi, H. Markov chain analysis for the neonatal inpatient flow in a hospital. Health Care Manag Sci 24, 92–116 (2021). https://doi.org/10.1007/s10729-020-09515-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10729-020-09515-3
Keywords
- Hospital capacity planning
- Bed utilization
- Neonatal patient flow
- Patient-days
- Operations research
- Markov chain
- Queueing theory
- Poisson process