Abstract
Background
Gastrointestinal hemorrhage (GIH) is reported to occur in 1–8% of patients admitted with acute ischemic stroke (AIS). AIS is considered to be a relative contraindication to GIE.
Aims
Evaluate the outcomes of gastrointestinal endoscopy (GIE) in patients hospitalized with AIS and GIH.
Methods
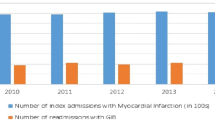
Patients hospitalized with AIS and GIH were included from the National Inpatient Sample 2005–2014. Primary outcome measure was in-hospital mortality in patients with AIS and GIH who underwent gastrointestinal endoscopy. Secondary outcomes were (1) resource utilization as measured by length of stay (LOS) and total hospitalization costs and (2) to identify independent predictors of undergoing GIE in patients with AIS and GIH. Confounders were adjusted for by using multivariable regression analysis.
Results
A total of 75,756 hospitalizations were included in the analysis. Using a multivariate analysis, the in-hospital mortality was significantly lower in patients who underwent GIE as compared to those who did not [aOR: 0.4, P < 0.001]. Patients who underwent GIE also had significantly shorter adjusted mean LOS [adjusted mean difference in LOS: 0.587 days, P < 0.001]. Patients with AIS and GIH who did not undergo GIE had significantly higher adjusted total hospitalization costs. [Mean adjusted difference in total hospitalization costs was $5801 (P < 0.001).] Independent predictors of undergoing GIE in this population were male gender, age > 65 years, Asian or Pacific race, hypovolemic shock, need for blood transfusion and admission to urban non-teaching hospital.
Conclusions
Gastrointestinal endoscopy can be safely performed in a substantial number of patients with AIS and GIH.

Similar content being viewed by others
References
Longstreth GF. Epidemiology of hospitalization for acute upper gastrointestinal hemorrhage: a population-based study. Am J Gastroenterol. 1995;90:206–210.
Antithrombotic Trialists C, Baigent C, Blackwell L, et al. Aspirin in the primary and secondary prevention of vascular disease: collaborative meta-analysis of individual participant data from randomised trials. Lancet. 2009;373:1849–1860.
Berger JS, Bhatt DL, Steg PG, et al. Bleeding, mortality, and antiplatelet therapy: results from the Clopidogrel for High Atherothrombotic Risk and Ischemic Stabilization, Management, and Avoidance (CHARISMA) trial. Am Heart J. 2011;162:98–105 e101.
Bhatt DL, Scheiman J, Abraham NS, et al. American College of Cardiology Foundation Task Force on Clinical Expert Consensus D: ACCF/ACG/AHA 2008 expert consensus document on reducing the gastrointestinal risks of antiplatelet therapy and NSAID use: a report of the American College of Cardiology Foundation Task Force on Clinical Expert Consensus Documents. Circulation. 2008;118:1894–1909.
Committee ASoP, Early DS, Ben-Menachem T, et al. Appropriate use of GI endoscopy. Gastrointest Endosc. 2012;75:1127–1131.
U.S. Agency for Healthcare Research and Quality. NIS Description of Data Elements. 2014. https://www.hcup-us.ahrq.gov/db/nation/nis/nisdde.jsp. Accessed 2 Dec 2018.
Garg SK, Anugwom C, Campbell J, et al. Early esophagogastroduodenoscopy is associated with better outcomes in upper gastrointestinal bleeding: a nationwide study. Endosc Int Open. 2017;5:E376–E386.
Quan H, Sundararajan V, Halfon P, et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care. 2005;43:1130–1139.
Southern DA, Quan H, Ghali WA. Comparison of the Elixhauser and Charlson/Deyo methods of comorbidity measurement in administrative data. Med Care. 2004;42:355–360.
Zhu H, Hill MD. Stroke: the Elixhauser Index for comorbidity adjustment of in-hospital case fatality. Neurology. 2008;71:283–287.
Frieling T. The role of the endoscopist in the stroke unit. Visc Med. 2016;32:53–57.
Hsu HL, Lin YH, Huang YC, et al. Gastrointestinal hemorrhage after acute ischemic stroke and its risk factors in Asians. Eur Neurol. 2009;62:212–218.
Johnston KC, Li JY, Lyden PD, et al. Medical and neurological complications of ischemic stroke: experience from the RANTTAS trial. RANTTAS Investigators. Stroke. 1998;29:447–453.
Kawakubo K, Ibayashi S, Nagao T, et al. Brain ischemia and gastric mucosal damage in spontaneously hypertensive rats. Dig Dis Sci. 2000;41:2383–2391. https://doi.org/10.1007/bf02100132.
Liu B, Liu S, Yin A, Siddiqi J. Risks and benefits of stress ulcer prophylaxis in adult neurocritical care patients: a systematic review and meta-analysis of randomized controlled trials. Crit Care. 2015;19:409.
Liu Y, Luo S, Kou L, et al. Ischemic stroke damages the intestinal mucosa and induces alteration of the intestinal lymphocytes and CCL19 mRNA in rats. Neurosci Lett. 2017;658:165–170.
Scharver CH, Hammond CS, Goldstein LB. Post-stroke Malnutrition and Dysphagia. In: Bales CW, Ritchie CS, eds. Handbook of Clinical Nutrition and Aging. Totowa: Humana Press; 2009:479–497.
Wijdicks EF, Fulgham JR, Batts KP. Gastrointestinal bleeding in stroke. Stroke. 1994;25:2146–2148.
Gonzalez-Fernandez M, Ottenstein L, Atanelov L, Christian AB. Dysphagia after Stroke: an overview. Curr Phys Med Rehabil Rep. 2013;1:187–196.
Chen CM, Hsu H-C, Chuang YW, Chang CH, Lin CH, Hong CZ. Study on factors affecting the occurrence of upper gastrointestinal bleeding in elderly acute stroke patients undergoing rehabilitation. J Nutr Health Aging. 2011;15:632–636.
Davenport RJ, Dennis MS, Warlow CP. Gastrointestinal hemorrhage after acute stroke. Stroke. 1996;27:421–424.
Kumar S, Selim MH, Caplan LR. Medical complications after stroke. Lancet Neurol. 2010;9:105–118.
Ogata T, Kamouchi M, Matsuo R, et al. Gastrointestinal bleeding in acute ischemic stroke: recent trends from the fukuoka stroke registry. Cerebrovasc Dis Extra. 2014;4:156–164.
Rumalla K, Mittal MK. Gastrointestinal bleeding in acute ischemic stroke: a population-based analysis of hospitalizations in the United States. J Stroke Cerebrovasc Dis. 2016;25:1728–1735.
Schirmer CM, Kornbluth J, Heilman CB, Bhardwaj A. Gastrointestinal prophylaxis in neurocritical care. Neurocrit Care. 2012;16:184–193.
O’Donnell MJ, Kapral MK, Fang J, et al. Gastrointestinal bleeding after acute ischemic stroke. Neurology. 2008;71:650–655.
Ji R, Shen H, Pan Y, et al. Risk score to predict gastrointestinal bleeding after acute ischemic stroke. BMC Gastroenterol. 2014;14:130.
Gruneir A, Griffith LE, Fisher K, et al. Increasing comorbidity and health services utilization in older adults with prior stroke. Neurology. 2016;87:2091–2098.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Authors do not have any financial or non-financial disclosure, and there is no conflict of interest.
Appendix: The International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM)
Appendix: The International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM)
Diagnosis/procedure name | ICD-9-CM code |
|---|---|
Cerebrovascular accident | |
Acute ischemic stroke (AIS) | 433.00, 433.01, 433.10, 433.11, 433.20, 433.21, 433.30, 433.31, 433.80, 433.81, 433.90, 433.91, 434.00, 434.01, 434.10, 434.11, 434.90, 434.91, 437.1 |
Acute hemorrhagic stroke | 430, 431, 432.0, 432.1, 432.9 |
Upper gastrointestinal bleeding | |
Bleeding esophageal varices | 456.0,456.2 |
Bleeding peptic ulcer (gastric or duodenal) | 531.00, 531.01, 531.20, 531.21, 531.40, 531.41, 531.60, 531.61 532.00, 532.01, 532.20, 532.21, 532.40, 532.41, 532.60, 532.61, 533.00, 533.01, 533.20, 533.21, 533.40, 533.41, 533.60, 533.61, 534.00, 534.01, 534.20, 534.21, 534.40, 534.41, 534.60, 534.61 |
Mallory–Weiss | 530.7 |
Gastritis with hemorrhage | 535.01, 535.11, 535.21, 535.41, 535.51, 535.61 |
Alcoholic gastritis with hemorrhage | 535.31 |
Dieulafoy’s lesion of stomach or duodenum | 537.84 |
Angiodysplasia of stomach or duodenum with hemorrhage | 537.83 |
Lower gastrointestinal bleeding: | |
Hemorrhage of rectum and anus | 569.3 |
Diverticulosis of colon with hemorrhage | 562.12 |
Diverticulitis of colon with hemorrhage | 562.13 |
Angiodysplasia of intestine with hemorrhage | 569.85 |
Dieulafoy’s lesion (hemorrhage) of intestine | 569.86 |
Blood in stool (hematochezia/melena) | 578.1 |
Hemorrhage of gastrointestinal tract unspecified | 578.9 |
Hemorrhoids | 455.2, 455.5, 455.8 |
Colorectal polyps | 211.3, 211.4 |
Colorectal cancer | 152.0, 152.1, 152.3, 152.8, 1529, 153.0,153.1, 153.2, 153.3, 153.4, 153.5, 153.6, 153.7,153.8, 153.9,154.0, 154.1, 154.2, 154.3, 154.8 230.0, 230.1, 230.2, 230.3, 230.4, 230.5, 230.6,230.7 |
Intestinal ischemia | 5570, 5571, 5579 |
Non-infectious colitis | 5581, 5582, 5583, 55,841, 55,842, 5589 |
Inflammatory bowel disease | 5550, 5551, 5552, 5559, 5560, 5561, 5562, 5563, 5564, 5565, 5566, 5568, 5569 |
Colon ulcer | 569.82 |
Solitary rectal ulcer syndrome | 569.41 |
Anal fissure | 565.0 |
Infectious colitis | 009.0–009.3 |
Radiation enteritis | 5581, 5582, 5583, 55,841, 55,842, 5589 |
Acute respiratory failure | 518.81 |
Acute renal failure including dialysis | 584.5, 584.6, 584.7, 584.8, 584.9, (renal dialysis status) V45.1, V56.0, V56.1 |
Hypovolemic shock | 276.50, 276.52, 785.59 |
Procedures | |
Blood transfusion | 99.03, 99.04 |
Mechanical ventilation | 96.71, 96.72 |
Endotracheal intubation | 96.01, 96.02, 96.04, 96.05, 31.1, 31.21, 31.29 |
Colonoscopy codes | 4522, 4523, 4524, 4525, 4542, 4543 |
Esophagogastroduodenoscopy (EGD) | 45.13, 45.14, 45.16, 42.23, 44.13, 42.33, 44.43 |
Rights and permissions
About this article
Cite this article
Siddiqui, M.T., Bilal, M., Gollapudi, L.A. et al. Endoscopy Is Relatively Safe in Patients with Acute Ischemic Stroke and Gastrointestinal Hemorrhage. Dig Dis Sci 64, 1588–1598 (2019). https://doi.org/10.1007/s10620-018-5399-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-018-5399-3