Abstract
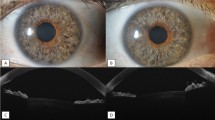
Our aim was to measure the endothelial quality of prestripped Descemet membrane endothelial keratoplasty (DMEK) 48 h after preparation in an eye bank with the Muraine technique and shipping in a distant center. Ten pairs of human corneas with similar eye bank endothelial cell density (ebECD) were stored in organ-culture (OC) for 25 days (20, 28) [median (10–90 percentiles)]. One cornea was then randomized to DMEK preparation using the Moria Muraine trephine, the other served as control. The grafts were left attached to the center of the cornea, immersed in the OC medium (without Dextran) and shipped to a distant center. After 48 h, the viable ECD (vECD) was assessed by image analysis after staining with Hoechst/Ethidium/Calcein-AM. In addition, immunostaining was performed on flat mounted tissues for structural (ZO-1, NCAM, CD166) and functional (Na+/K+ ATPase) proteins of ECs, and for collagen I. Just before stripping, ebECD was 2428 (2268–2669) cells/mm2 for DMEK and 2471 (2135–2714) for controls (P = 1). Forty-eight hours after stripping, vECD was 2057 (1829–2463) cells/mm2 for DMEK and 2119 (1496–2525) for controls (P = 0.508). The expression patterns of the 5 proteins were similar in ECs of both groups. Notably, the deep posterior folds observed in OC controls almost disappeared in prestripped DMEK due to the lack of a link between Descemet membrane and stroma. As a consequence of the elimination of mechanical stress in these zones, EC evenly covered the whole graft. In conclusion, DMEK prestripping with the Muraine technique and shipping away can be used safely by eye banks.





Similar content being viewed by others
References
Albon J, Tullo AB, Aktar S, Boulton ME (2000) Apoptosis in the endothelium of human corneas for transplantation. Investig Ophthalmol Vis Sci 41:2887–2893
Anshu A, Price MO, Price FW Jr (2012) Risk of corneal transplant rejection significantly reduced with descemet’s membrane endothelial keratoplasty. Ophthalmology 119:536–540
Anwar M, Teichmann KD (2002) Big-bubble technique to bare descemet’s membrane in anterior lamellar keratoplasty. J Cataract Refract Surg 28:398–403
Bernard A et al (2014) CorneaJ: an imageJ plugin for semi-automated measurement of corneal endothelial cell viability. Cornea 33:604–609
Bhogal M, Balda MS, Matter K, Allan BD (2016) Global cell-by-cell evaluation of endothelial viability after two methods of graft preparation in descemet membrane endothelial keratoplasty. Br J Ophthalmol 100:572–578
Busin M, Scorcia V, Patel AK, Salvalaio G, Ponzin D (2010) Pneumatic dissection and storage of donor endothelial tissue for descemet’s membrane endothelial keratoplasty: a novel technique. Ophthalmology 117:1517–1520
Dapena I, Ham L, Melles GR (2009) Endothelial keratoplasty: DSEK/DSAEK or DMEK—the thinner the better? Curr Opin Ophthalmol 20:299–307
Dapena I, Moutsouris K, Droutsas K, Ham L, van Dijk K, Melles GR (2011) Standardized “no-touch” technique for descemet membrane endothelial keratoplasty. Arch Ophthalmol 129:88–94
Deng SX, Sanchez PJ, Chen L (2015) Clinical outcomes of descemet membrane endothelial keratoplasty using eye bank-prepared tissues. Am J Ophthalmol 159:590–596
EBAA (2015) Eye banking statistical report. Eye Bank Association of America, Atlanta
EEBA (2018) Directory, 26 edn, January 2018. European Eye Bank Association, Venice
Forest F, Thuret G, Gain P, Dumollard JM, Peoc’h M, Perrache C, He Z (2015) Optimization of immunostaining of flatmounted human corneas. Mol Vis 21:1345–1356
Gain P, Jullienne R, He Z, Aldossary M, Acquart S, Cognasse F, Thuret G (2016) Global survey of corneal transplantation and eye banking. JAMA Ophthalmol 134:167–173
Gauthier AS et al (2017) Very early endothelial cell loss after penetrating keratoplasty with organ-cultured corneas. Br J Ophthalmol 101:1113–1118
He Z et al (2011) Optimization of immunolocalization of cell cycle proteins in human corneal endothelial cells. Mol Vis 17:3494–3511
He Z et al (2016) 3D map of the human corneal endothelial cell. Sci Rep 6:29047
Heinzelmann S, Bohringer D, Eberwein P, Reinhard T, Maier P (2017) Graft dislocation and graft failure following descemet membrane endothelial keratoplasty (DMEK) using precut tissue: a retrospective cohort study. Graefes Arch Clin Exp Ophthalmol 255:127–133
Jardine GJ, Holiman JD, Stoeger CG, Chamberlain WD (2014) Imaging and quantification of endothelial cell loss in eye bank prepared DMEK grafts using trainable segmentation software. Curr Eye Res 39:894–901
Jumelle C et al (2017) Considering 3D topography of endothelial folds to improve cell count of organ cultured corneas. Cell Tissue Bank 18:185–191
Kelliher C, Engler C, Speck C, Ward D, Farazdaghi S, Jun AS (2009) A comprehensive analysis of eye bank-prepared posterior lamellar corneal tissue for use in endothelial keratoplasty. Cornea 28:966–970
Kitazawa K et al (2017) The existence of dead cells in donor corneal endothelium preserved with storage media. Br J Ophthalmol 101:1725–1730
Kruse FE, Laaser K, Cursiefen C, Heindl LM, Schlotzer-Schrehardt U, Riss S, Bachmann BO (2011) A stepwise approach to donor preparation and insertion increases safety and outcome of descemet membrane endothelial keratoplasty. Cornea 30:580–587
Liu YC, Alvarez Paraz CM, Cajucom-Uy HY, Agahari D, Sethuraman S, Tan DT, Mehta JS (2014a) Risk factors for donor endothelial loss in eye bank-prepared posterior lamellar corneal tissue for descemet stripping automated endothelial keratoplasty. Cornea 33:677–682
Liu YC, Teo EP, Adnan KB, Yam GH, Peh GS, Tan DT, Mehta JS (2014b) Endothelial approach ultrathin corneal grafts prepared by femtosecond laser for descemet stripping endothelial keratoplasty. Investig Ophthalmol Vis Sci 55:8393–8401
Melles GR, Lander F, Rietveld FJ (2002) Transplantation of descemet’s membrane carrying viable endothelium through a small scleral incision. Cornea 21:415–418
Menzel-Severing J, Kruse FE, Tourtas T (2017) Organ-cultured, prestripped donor tissue for DMEK surgery: clinical outcomes. Br J Ophthalmol 101:1124–1127
Muraine M, Gueudry J, He Z, Piselli S, Lefevre S, Toubeau D (2013) Novel technique for the preparation of corneal grafts for descemet membrane endothelial keratoplasty. Am J Ophthalmol 156:851–859
Nejepinska J, Juklova K, Jirsova K (2010) Organ culture, but not hypothermic storage, facilitates the repair of the corneal endothelium following mechanical damage. Acta Ophthalmol 88:413–419
Nelson BA, Ritenour RJ (2014) Tissue quality of eye-bank-prepared precut corneas for descemet’s stripping automated endothelial keratoplasty. Can J Ophthalmol 49:92–95
Okumura N et al (2014) Cell surface markers of functional phenotypic corneal endothelial cells. Investig Ophthalmol Vis Sci 55:7610–7618
Parekh M, Baruzzo M, Favaro E, Borroni D, Ferrari S, Ponzin D, Ruzza A (2017) Standardizing descemet membrane endothelial keratoplasty graft preparation method in the eye bank-experience of 527 descemet membrane endothelial keratoplasty tissues. Cornea 36:1458–1466
Pipparelli A et al (2011) Pan-corneal endothelial viability assessment: application to endothelial grafts predissected by eye banks. Investig Ophthalmol Vis Sci 52:6018–6025
Price FW Jr, Price MO (2013) Evolution of endothelial keratoplasty. Cornea 32(Suppl 1):S28–S32
Price MO, Baig KM, Brubaker JW, Price FW Jr (2008) Randomized, prospective comparison of precut vs surgeon-dissected grafts for descemet stripping automated endothelial keratoplasty. Am J Ophthalmol 146:36–41
Price MO, Giebel AW, Fairchild KM, Price FW Jr (2009) Descemet’s membrane endothelial keratoplasty: prospective multicenter study of visual and refractive outcomes and endothelial survival. Ophthalmology 116:2361–2368
Ragunathan S, Ivarsen A, Nielsen K, Hjortdal J (2014) Comparison of organ cultured precut corneas versus surgeon-cut corneas for descemet’s stripping automated endothelial keratoplasty. Cell Tissue Bank 15:573–578
Romano V et al (2017) Comparison of preservation and transportation protocols for preloaded descemet membrane endothelial keratoplasty. Br J Ophthalmol 102:549–555
Schallhorn JM, Holiman JD, Stoeger CG, Chamberlain W (2016) Quantification and patterns of endothelial cell loss due to eye bank preparation and injector method in descemet membrane endothelial keratoplasty tissues. Cornea 35:377–382
Terry MA, Shamie N, Chen ES, Phillips PM, Hoar KL, Friend DJ (2009) Precut tissue for descemet’s stripping automated endothelial keratoplasty: vision, astigmatism, and endothelial survival. Ophthalmology 116:248–256
Yoeruek E, Bartz-Schmidt KU, Hofmann J (2016) Impact of the radius of the injector system on the cell viability in descemet membrane endothelial keratoplasty: an ex vivo experimental study. Acta Ophthalmol 94:e1–e5
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Dr. Muraine is consultant for Moria, France. Dr Gain and Dr Thuret are consultant for les Laboratoires Théa, France. The other authors have no conflicting interest to disclose.
Human participants and/or animal rights
Corneas assigned to scientific use and procured by the Normandy Eye Bank (Rouen, France) were used after informed consent of the relatives, as authorized by French bioethics laws. All procedures conformed to the tenets of the Declaration of Helsinki for biomedical research involving human subjects.
Informed consent
Not applicable.
Rights and permissions
About this article
Cite this article
He, Z., Gueudry, J., Toubeau, D. et al. Endothelial quality of eye bank-prestripped DMEK prepared form organ-cultured corneas with the Muraine technique. Cell Tissue Bank 19, 705–716 (2018). https://doi.org/10.1007/s10561-018-9723-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10561-018-9723-0