Abstract
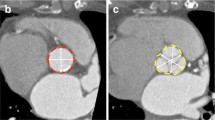
Recognition of bicuspid aortic valve (BAV) may be challenging in elderly patients with heavily calcified aortic valves undergoing transcatheter aortic valve replacement (TAVR). In this subset, the diagnostic value of pre-procedural echocardiography in clinical routine is unknown. From a total of 2583 patients undergoing TAVR in our center, we determined the rate of BAV detected by routine echocardiography as documented in the medical records. Pre-procedural multidetector computed tomography (MDCT) images were retrospectively analyzed for the presence of BAV and served as reference standard. Using MDCT criteria, BAV was found in 235 (9.1%) (age 80.1 years [interquartile range 76.4; 83.4], 44.3% female). Of these, only 27/235 (11.5%) had been identified as BAV according to echocardiography reports, whereas 6/2348 (0.3%) with TAV had been wrongly diagnosed as BAV (p < 0.001; sensitivity 11.5%, specificity 99.7%). Correct diagnosis of BAV by echocardiography was more likely when transesophageal echocardiography was available (odds ratio (OR) 5.12 [95% confidence interval (CI) 2.22; 11.80]; p < 0.001) and the reader was experienced (OR 5.28 [95% CI 1.55; 18.04]; p = 0.008). Furthermore, correct diagnosis of BAV was more likely in bicommissural-type BAV (OR 2.22 [95% CI 0.90; 5.48]; p = 0.08), whereas heavy aortic valve calcification lead to misdiagnosis (OR 0.39 [95% CI 0.14; 1.06]; p = 0.07). In elderly patients with severe aortic stenosis that are candidates for TAVR, the presence of BAV may be considerably underestimated when relying solely on routine echocardiography. This underlines the value of MDCT for the screening of BAV in this patient population.



Similar content being viewed by others
References
Yoon SH, Bleiziffer S, De Backer O et al (2017) Outcomes in transcatheter aortic valve replacement for bicuspid versus tricuspid aortic valve stenosis. J Am Coll Cardiol 69(21):2579–2589. doi:https://doi.org/10.1016/j.jacc.2017.03.017
Perlman GY, Blanke P, Dvir D et al (2016) Bicuspid aortic valve stenosis: favorable early outcomes with a next-generation transcatheter heart valve in a multicenter study. JACC Cardiovasc Interv 9(8):817–824. doi:https://doi.org/10.1016/j.jcin.2016.01.002
Takeda H, Muro T, Saito T et al (2013) Diagnostic accuracy of transthoracic and transesophageal echocardiography for the diagnosis of bicuspid aortic valve: comparison with operative findings. Osaka City Med J 59(2):69–78
Tanaka R, Yoshioka K, Niinuma H et al (2010) Diagnostic value of cardiac CT in the evaluation of bicuspid aortic stenosis: comparison with echocardiography and operative findings. Am J Roentgenol 195(4):895–899. doi:https://doi.org/10.2214/AJR.09.3164
Ryan T, Berlacher K, Lindner JR et al (2015) COCATS 4 Task Force 5: training in echocardiography. J Am Coll Cardiol 65(17):1786–1799. doi:https://doi.org/10.1016/j.jacc.2015.03.035
Kim WK, Blumenstein J, Liebetrau C et al (2017) Comparison of outcomes using balloon-expandable versus self-expanding transcatheter prostheses according to the extent of aortic valve calcification. Clin Res Cardiol 106(12):995–1004. doi:https://doi.org/10.1007/s00392-017-1149-3
Joo I, Park EA, Kim KH et al (2012) MDCT differentiation between bicuspid and tricuspid aortic valves in patients with aortic valvular disease: correlation with surgical findings. Int J Cardiovasc Imaging 28(1):171–182. doi:https://doi.org/10.1007/s10554-010-9780-3
Jilaihawi H, Chen M, Webb J et al (2016) A bicuspid aortic valve imaging classification for the TAVR era. JACC Cardiovasc Imaging 9(10):1145–1158. doi:https://doi.org/10.1016/j.jcmg.2015.12.022
Rosenhek R, Binder T, Porenta G et al (2000) Predictors of outcome in severe, asymptomatic aortic stenosis. N Engl J Med 343(9):611–617. doi:https://doi.org/10.1056/NEJM200008313430903
Kong WKF, Delgado V, Bax JJ (2017) Bicuspid aortic valve: what to image in patients considered for transcatheter aortic valve replacement? Circ Cardiovasc Imaging. doi:https://doi.org/10.1161/CIRCIMAGING.117.005987
Kim WK, Gaede L, Husser O et al (2018) Computed tomography for diagnosis and classification of bicuspid aortic valve disease in transcatheter aortic valve replacement. JACC Cardiovasc Imaging 11(10):1539–1540. doi:https://doi.org/10.1016/j.jcmg.2017.12.010
Kim WK, Schafer U, Tchetche D et al (2019) Incidence and outcome of peri-procedural transcatheter heart valve embolization and migration: the TRAVEL Registry (TranscatheteR HeArt Valve EmboLization and Migration). Eur Heart J. doi:https://doi.org/10.1093/eurheartj/ehz429
Mack MJ, Leon MB, Thourani VH et al (2019) Transcatheter aortic-valve replacement with a balloon-expandable valve in low-risk patients. N Engl J Med 380(18):1695–1705. doi:https://doi.org/10.1056/NEJMoa1814052
Acknowledgements
We thank Elizabeth Martinson, Ph.D., from the KHFI Editorial Office for her editorial assistance.
Financial disclosures
Won-Keun Kim: Proctor for Symetis SA, St. Jude Medical/Abbott, Lecture Honoraria from Symetis SA, St. Jude Medical/Abbott. Christoph Liebetrau: Lecture Honoraria from Abbott, Astra Zeneca, Bayer, Berlin Chemie, Boehringer Ingelheim, Daiichi-Sankyio, and Pfizer—Bristol-Myers Squibb; travel accommodation/meeting expenses from Bayer and Daiichi-Sankyo. Matthias Renker: Lecture Honoraria from St. Jude Medical/Abbott. Andreas Rolf: Lecture Honoraria from Astra Zeneca, Boehringer, Pfizer, MSD, Bristol Myers Squibb. Mirko Doss: Proctor for St. Jude Medical/Abbott. Christian W. Hamm: Advisory Board Medtronic. Helge Möllmann: Proctor Fees and/or Speaker Honoraria from Abbott, Biotronic, Edwards Lifesciences, St. Jude Medical, Symetis SA.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All other authors declare that they have no relevant conflict of interest to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations
Rights and permissions
About this article
Cite this article
Kim, WK., Liebetrau, C., Fischer-Rasokat, U. et al. Challenges of recognizing bicuspid aortic valve in elderly patients undergoing TAVR. Int J Cardiovasc Imaging 36, 251–256 (2020). https://doi.org/10.1007/s10554-019-01704-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10554-019-01704-8