Abstract
Purpose
The variation in breast cancer (BC)-risk factor associations between screen-detected (SD) and non-screen-detected (NSD) tumors has been poorly studied, despite the interest of this aspect in risk assessment and prevention. This study analyzes the differences in breast cancer-risk factor associations according to detection method and tumor phenotype in Spanish women aged between 50 and 69.
Methods
We examined 900 BC cases and 896 controls aged between 50 and 69, recruited in the multicase–control MCC-Spain study. With regard to the cases, 460 were detected by screening mammography, whereas 144 were diagnosed by other means. By tumor phenotype, 591 were HR+, 153 were HER2+, and 58 were TN. Lifestyle, reproductive factors, family history of BC, and tumor characteristics were analyzed. Logistic regression models were used to compare cases vs. controls and SD vs. NSD cases. Multinomial regression models (controls used as a reference) were adjusted for case analysis according to phenotype and detection method.
Results
TN was associated with a lower risk of SD BC (OR 0.30 IC 0.10–0.89), as were intermediate (OR 0.18 IC 0.07–0.44) and advanced stages at diagnosis (OR 0.11 IC 0.03–0.34). Nulliparity in postmenopausal women and age at menopause were related to an increased risk of SD BC (OR 1.60 IC 1.08–2.36; OR 1.48 IC 1.09–2.00, respectively). Nulliparity in postmenopausal women was associated with a higher risk of HR+ (OR 1.66 IC 1.15–2.40). Age at menopause was related to a greater risk of HR+ (OR 1.60 IC 1.22–2.11) and HER2+ (OR 1.59 IC 1.03–2.45) tumors.
Conclusion
Reproductive risk factors are associated with SD BC, as are HR+ tumors. Differences in BC-risk factor associations according to detection method may be related to prevailing phenotypes among categories.
Similar content being viewed by others
Introduction
Breast cancer (BC) is the most common tumor among women worldwide. An estimated 2,261,419 new cases occurred globally in 2020 [1]. The main associated risk factors include nulliparity, early menarche, and late menopause (all three factors related to endogenous hormone exposure), as well as alcohol consumption, being overweight, obesity, and lack of physical activity [2,3,4,5,6]. High-penetrance gene mutations (BRCA1, BRCA2, TP53, PTEN) considerably increase BC risk, however, they only account for a small proportion of the disease burden given their low frequency in the population [2, 4, 5].
Breast cancer is a heterogeneous disease; it includes several entities with a different natural history and response to treatment. Breast tumors can be classified into phenotypes based on the expression of hormone receptors and human epidermal growth factor receptor 2 in tumor cells [7]. Reproductive behavior influences the development of HR+ (hormone receptor positive) tumors as it modifies estrogen levels, whereas lifestyle-related factors (body mass index [BMI], tobacco, alcohol, and physical activity) similarly affect different tumor subtypes [8,9,10]. In addition, HR+ breast carcinomas often have smaller tumors and are in an early stage at diagnosis, features that are associated with a better prognosis [9, 11]. In contrast, HER2+ (human epidermal growth factor receptor 2 positive) and TN (triple negative) carcinomas have larger tumors and are in a more advanced stage at diagnosis [9]. Additionally, TN is associated with aggressive metastatic breast cancer, partly due to its contribution to the rapid progression of the disease [12].
Through European Council Recommendation of 2 December 2003 on cancer screening [13], the EU advises the implementation of systematic population-based breast cancer screening programs as part of prevention strategies. By performing diagnostic tests on an asymptomatic population, screening allows for early detection of the disease, thereby helping to reduce the impact on mortality [14,15,16]. In Spain, these programs have been included in the Spanish National Health System’s service portfolio since 2014, although they have been progressively implemented since the 1990s in different regions. They consist of biennial mammography and the target population is women aged 50–69. According to 2017 data [17], coverage is approximately 85% and the participation rate is over 70%. Nevertheless, uptake is unequal among individuals; women living in the least deprived areas are more likely to participate in breast cancer screening programs than women living in the most deprived areas. This is not only due to their limited knowledge about mammography or misconceptions, but also to practical barriers such as difficulties attending mammography appointments or family commitments [18]. Apart from population-based screening programs, part of the target population participates in opportunistic breast cancer screening practices [19, 20]. These are individual, non-systematic population-based interventions carried out at the patient’s request or arising from a visit for another medical reason.
Tumor characteristics according to detection method have been previously studied. By comparison, non-screen-detected BC (either due to a failure to participate in screening programs or the appearance of interval cancer) is associated with more advanced stages at diagnosis, aggressive tumors, and poorer prognoses, whereas screen-detected tumors are more frequently diagnosed at an early stage, are of a small size, and express hormone receptors [21,22,23,24].
A previous study in the United States has shown differences in breast cancer-risk factor associations by the method of detection [25]. However, there are few studies on variation in breast cancer-risk factor associations between screen-detected and non-screen-detected tumors, and therefore there is little information available on this matter. This study examines whether the screening method affects risk factor associations, regardless of tumor phenotype.
Thus, we aim to analyze the differences in breast cancer-risk factor associations according to method of detection and tumor phenotype in a population of Spanish women aged 50–69.
Material and methods
Study population
MCC-Spain is a population-based multicase–control study aimed at investigating the influence of environmental and genetic factors on different tumors (gastric, colorectal, breast, prostate, and chronic lymphocytic leukemia) [26]. Cases and population controls were recruited between 2008 and 2013 in twelve Spanish regions. Incident cases were actively recruited at 23 collaborating hospitals and population controls were contacted by telephone and invited to take part in the study, after being randomly selected from primary care center lists within the catchment area of these 23 hospitals. Cases had no prior history of cancer and they were identified as soon as possible after the diagnosis was made through an active search that included regular visits to the collaborating hospital departments. Only histologically confirmed incident cancer cases, including breast cancer, were included in the study (International Classification of Diseases 10th Revision: C50, D05.1, D05.7).
Controls were frequency-matched to cases by age, sex, and region, ensuring that there was at least one control of the same sex and within the same five-year age interval for each case in each region.
Participants had resided within the hospital catchment areas for at least 6 months. Cases and controls answered an epidemiological questionnaire in a personal interview. The questionnaire (available at http://www.mccspain.org) focused on socio-demographic characteristics, lifestyle, medical history, and family history of cancer. Additionally, subjects were provided with a semi-quantitative Food Frequency Questionnaire (FFQ), which was a modified version of a previously validated instrument in Spain [27]. It estimated regular dietary intake during the previous year. Clinical and pathological information on the diagnosis and treatment of tumors was collected from hospital records.
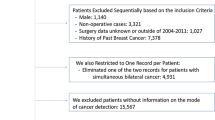
We included 1.796 women in the study in this analysis, 896 controls and 900 BC cases. Inclusion criteria for cases were BC tumor histologically diagnosed during the recruitment period, home address in one of the collaborating hospitals’ catching area, age range 50–69. Cases exclusion criteria were BC diagnosis previous to patient recruitment period, inability to communicate in Spanish, and physical incapacity to take part in the study. By phenotype, 591 were HR+ tumors, 153 were HER2+, and 58 were TN (phenotype data were missing for 98 cases). By self-referred detection method, 460 cases were screen-detected either by organized or spontaneous screening mammography (average age 59,04 years old), and 144 cases were non-screen-detected (average age 57,88 years old). Detection method data were missing and/or inconsistent for 296 cases. The age range was defined in accordance with European Council recommendations on cancer screening programs [13].
Definition of variables.
Detection method: BC cases were classified into screen-detected and non-screen-detected tumors, based on the answers provided in the epidemiological questionnaire. BC cases were considered screen-detected whenever participants declared that the tumor had been diagnosed by screening (organized or spontaneous screening mammography performed in the absence of symptoms) and, additionally, that this mammogram had been performed in the last 6 months. On the contrary, BC cases were classified as non-screen-detected when patients declared that the tumor had not been diagnosed by mammogram screening and, additionally, that they had not undergone a screening mammography in the last 6 months.
Using a simplified version of the St Gallen International Consensus [28], breast tumors were classified into the following phenotypes: HR+ (hormone receptor positive), HER2+ (human epidermal growth factor receptor 2 positive, regardless of hormone receptors), and TN (triple negative, i.e., negative for progesterone and estrogen receptors, and human epidermal growth factor receptor 2 negative). Other tumor characteristics included the stage at diagnosis (early − 0, IA, IB −; intermediate − IIA, IIB −; and advanced − IIIA, IIIB, IIIC, IV −), extension (in situ, invasive), and histology (ductal, lobular, other).
Epidemiological factors included reproductive factors (age at menarche, nulliparity, age at first birth, menopausal status, and age at menopause), history of breast cancer in first-degree relatives, and lifestyles factors (alcohol consumption over the year prior to the interview, tobacco use a month before the interview, leisure-time physical activity over a ten-year period up to two years prior to the interview, BMI at recruitment, and fruit and vegetable consumption over the year prior to the interview).
Statistical analysis
A descriptive analysis of tumor characteristics and epidemiological factors was conducted for screen-detected/non-screen-detected cases, total cases/controls, screen-detected cases/controls, non-screen-detected cases/controls, HR+ cases/controls, HER2+ cases/controls, and TN/controls. Frequencies and percentages were calculated, and significant differences were tested using the Chi-square test for categorical variables and the Wilcoxon test for continuous variables.
Adjusted odds ratios (OR) and 95% confidence intervals (CI) were calculated using multivariate logistic regression models to analyze the association between epidemiological factors and overall BC risk, as well as to investigate the differences in screen-detected/non-screen-detected cases related to tumor characteristics and epidemiological factors.
A multinomial logistic regression model was conducted to examine whether risk factor associations vary according to method of detection. An additional multinomial logistic regression model was used to analyze variation in risk factor associations by tumor phenotype. In both models, controls were used as a reference group. The exponential multinomial logarithmic coefficient provided an estimate of relative risk, expressed here as the relative risk (RR) coefficient.
p values were considered statistically significant below 0.05. All statistical analyses were performed using the statistical software R (version 3.6.0). Analyses were adjusted by region, educational level, age, and menopausal status.
In order to assess the age-related risk factors of menopause and nulliparity, analyses were performed for the overall sample, for postmenopausal women, and for parous women.
Results
Sample description
Table 1 shows the results of the descriptive analysis. Statistically significant differences are observed in the association with epidemiological factors and tumor characteristics (only for cases), with heterogeneous results depending on the method of detection and phenotype.
Comparative analysis of tumor characteristics for screen-detected and non-screen-detected breast cancer
The multivariate logistic regression analysis for screen-detected/non-screen-detected tumors (Table 2) shows significant differences in terms of tumor characteristics. Screen-detected breast cancers are less likely to be diagnosed at intermediate (OR = 0.23; 95%CI 0.11–0.47) and advanced stages (OR = 0.14; 95%CI 0.06–0.36) than non-screen-detected breast cancers. Similar results are obtained for postmenopausal women and parous women, both for intermediate (OR = 0.18; 95%CI 0.07–0.44 and OR = 0.21; 95%CI 0.09–0.52, respectively) and advanced stages (OR = 0.11; 95%CI 0.03–0.34 and OR = 0.18; 95%CI 0.06–0.53, respectively). In comparison with HR+ tumors, TN tumors (OR = 0.30; 95%CI 0.10–0.89) are less likely to be screen-detected. Similar results are found for parous women (OR = 0.18; 95%CI 0.05–0.67).
Breast cancer risk by detection method
Table 3 shows breast cancer-risk factor associations according to detection method. The multinomial logistic regression model for the overall sample reveals that BMI was associated with a 5% greater risk of screen-detected BC (RR = 1.05; 95%CI 1.02–1.08) and a 4% greater risk of non-screen-detected BC (RR = 1.04; 95%CI 1.00–1.08). Similar results are shown for BMI among postmenopausal women and parous women, although in both cases we found a borderline significant trend for risk association with non-screen-detected breast cancers. Likewise, BMI is associated with a slightly higher risk of BC for overall breast cancer cases regardless of the detection method, as shown in the supplementary table.
Concerning reproductive factors, the association of nulliparity and age at menopause with breast cancer risk varied by detection method for postmenopausal women only, with a 60% (RR = 1.60; 1.08–2.36) and 48% (RR = 1.48; 95%CI 1.09–2.00) greater risk of screen-detected BC, respectively. Similar results for nulliparity and age at menopause are found in postmenopausal women for overall breast cancer cases, irrespective of the detection method (see the supplementary table).
Breast cancer-risk variation by phenotype
Concerning lifestyle factors, the risk factor association analysis by phenotype (Table 4) reveals that BMI is related to a marginally increased risk of HR+ tumors for the overall sample (RR = 1.04; 95%CI 1.01–1.07), but also for postmenopausal women (RR = 1.05; 95%CI 1.02–1.08) and parous women (RR = 1.04; 95%CI 1.01–1.07). In the overall sample, we also found a probable increased risk of HER2+ (RR = 1.03; 95%CI 1.00–1.07) and TN (RR = 1.05; 95%CI 1.00–1.10) for BMI, with borderline significant results. Additionally, BMI is associated with a risk of TN (RR = 1.05; 95%CI 1.01–1.10) among postmenopausal women. All in all, the results indicated that BMI is related to a small increase in breast cancer risk, regardless of tumor phenotype.
Table 4 also shows an increased risk, albeit very marginal, of HR+ tumors associated with alcohol consumption in the overall sample. In a similar manner, a borderline significant trend is observed for all phenotypes, also in postmenopausal and parous women.
A possible risk association between lack of physical activity and HER2+ breast cancer is observed in postmenopausal (RR = 1.54; 95%CI 0.98–2.41) and parous women (RR = 1.49; 95%CI 0.96–2.31), with borderline significant results.
Regarding reproductive factors, in postmenopausal women the strength of association of nulliparity varied according to phenotype, with an approximately 60% greater risk of HR+ BC (RR = 1.66; 95%CI 1.15–2.40). Age at menopause also changed risk associations depending on phenotype, with an approximately 60% greater risk of HR+ BC (RR = 1.60; 95%CI 1.22–2.11) and HER2+ BC (RR = 1.59; 95%CI 1.03–2.45). Additionally, in parous women, we also found that age at first birth was positively correlated to TN BC (RR = 1.07; 95%CI 1.01–1.12).
Discussion
This study analyzes variation in breast cancer-risk factors according to method of detection and tumor phenotype. The results showed differences between the association of screen-detected and non-screen-detected breast cancer with the reproductive risk factors of age at menopause and nulliparity. In postmenopausal women, these factors were associated with a risk of screen-detected breast cancer. Meanwhile, age at menopause and nulliparity entailed a greater risk of tumors containing positive hormone receptors. Moreover, we found that screen-detected breast cancers were less likely to be TN tumors. In addition, BMI was related to an increased risk of breast cancer, regardless of the detection method and tumor phenotype.
There is little evidence available on the association of epidemiological risk factors with breast cancer according to method of detection. Unlike the present study, the study conducted by Sprague et al. [25]does not consider tumor phenotype in the analysis. This study reveals that the association of parity/nulliparity with screen-detected and non-screen-detected tumors varies, in line with our results. Nonetheless, they found no differences in the association with age at menopause between screen-detected and non-screen-detected breast cancers.
Previous analyses [29] found that the association of BMI and family history of breast cancer varied between interval BC and screen-detected BC. Although our study does not specifically look at interval breast cancers, we can assume that they are included in non-screen-detected BC, as defined in this paper. Our results show no variation in the association of family history with SD and NSD breast cancers, with no significant risk association in either case. Meanwhile, BMI is a known risk factor for cancer in general, and particularly for breast cancer in postmenopausal women [30], possibly due to increased levels of circulating endogenous estrogen [31]. Accordingly, our analysis reveals a risk association, though slight, between breast cancer and BMI. However, we found no variation in the association of BMI with SD and NSD breast cancers. A prior study comparing SD and interval BC shows that overweight women are more likely to have SD breast cancer [29], although weight-related barriers to mammography screening have been described previously [32]. Further analysis is needed to ascertain the associations between screen-detected and non-screen-detected breast cancers and BMI as well as family history of breast cancer.
Previous evidence has demonstrated a risk association between tumors expressing hormone receptors and reproductive factors [3,4,5, 33]. In the present study, similar results were observed for nulliparity (in postmenopausal women) and age at menopause, although we found no further associations with other reproductive variables that are also known risk factors for hormone-dependent tumors.
Considering the results according to detection method and phenotype, similarities can be observed in the association between screen-detected breast cancers and HR+ tumors with reproductive factors, specifically for nulliparity and age at menopause. This fact suggests that variation in breast cancer-risk factor associations by method of detection (screen-detected vs. non-screen-detected) could be explained by underlying prevailing phenotypes. Thus, the risk association of screen-detected tumors with these reproductive factors could be explained by the fact that they are predominantly hormone-sensitive tumors, which are in turn related to reproductive factors that modify endogenous hormone exposure [21, 34,35,36]. In line with these observations, several studies [23, 24, 37, 38] contribute further evidence that TN tumors are less frequent in breast cancers detected by screening mammography. Due to their rapid progression and shorter asymptomatic phase, these tumors often appear in the time lapse between two screening mammograms (2 years). In this regard, prevalence bias may be a limitation in this study, since HR+ tumors grow slowly and are thus more likely to be detected by screening than other tumor phenotypes.
Our results do not conclusively confirm associations with other known lifestyle-related risk factors [3, 4], such as tobacco use [39,40,41,42,43] and alcohol consumption [6, 44,45,46,47]; this could be due to the limitations of the study, which are outlined later in this section.
With regard to self-referred data (e.g., detection method), there may be a recall bias. Nonetheless, the impact was lessened thanks to the intervention of professional interviewers and the thorough design of the epidemiological questionnaire. Another limitation in this analysis may be the limited number of cases including information on phenotype, which makes stratification difficult.
The strengths of our study include its population-based design and the fact that it includes both opportunistic and organized screening, unlike most studies, which refer exclusively to the latter. As far as we know, this is one of the few studies conducted in a European context that analyzes breast cancer-risk factors according to detection method and tumor phenotype. Taking into account these results it would be advisable to consider detection method in future epidemiological studies on breast cancer. Moreover, further research on the differences between SD and NSD tumors, regarding prognostic and predictive tumor characteristics, could provide relevant information for patient management.
In conclusion, we found that screen-detected breast cancers are essentially associated with reproductive risk factors, and also with tumors including positive hormone receptors. Our results seem to indicate that the differences found in breast cancer-risk factor associations according to detection method can be attributed to predominating phenotypes, given that screening mammography mostly detects hormone-sensitive tumors which are susceptible to changes caused by reproductive factors.
Availability of data and material
The database was registered with the Spanish data protection Agency, under Number 210267217118. Data are available under request.
Code availability
Not Applicable.
References
Global Cancer Observatory (GLOBOCAN) (2020) Cancer Today. https://gco.iarc.fr/today/home. Accessed 15 Dec 2020
World Health Organization (2020) OMS|Breast cancer: prevention and control. https://www.who.int/cancer/detection/breastcancer/en/. Accessed 2 March 2020
Lacey JV, Kreimer AR, Buys SS, Marcus PM, Chang S-C, Leitzmann MF et al (2009) Breast cancer epidemiology according to recognized breast cancer risk factors in the Prostate, Lung, Colorectal and Ovarian (PLCO) Cancer Screening Trial Cohort. BMC Cancer 9:84. https://doi.org/10.1186/1471-2407-9-84
Key TJ, Verkasalo PK, Banks E (2001) Epidemiology of breast cancer. Lancet Oncol 2:133–140. https://doi.org/10.1186/1471-2407-9-84
Martin A-M (2000) Genetic and hormonal risk factors in breast cancer. J Natl Cancer Inst 92(14):1126–1135. https://doi.org/10.1093/jnci/92.14.1126
Key TJ, Reeves GK (2016) Alcohol, diet, and risk of breast cancer. BMJ. https://doi.org/10.1136/bmj.i2503
Goldhirsch A, Winer EP, Coates AS, Gelbe RD, Piccart-Gebhart M, Thürlimann B et al (2013) Personalizing the treatment of women with early breast cancer: highlights of the St Gallen International Expert Consensus on the Primary Therapy of Early Breast Cancer 2013. Ann Oncol 24(9):2206–23. https://doi.org/10.1093/annonc/mdt303
Makama M, Drukker CA, Rutgers EJT, Slaets L, Cardoso F, Rookus MA et al (2017) An association study of established breast cancer reproductive and lifestyle risk factors with tumour subtype defined by the prognostic 70-gene expression signature (MammaPrint®). Eur J Cancer 75:5–13. https://doi.org/10.1016/j.ejca.2016.12.024
Zhang L, Huang Y, Feng Z, Wang X, Li H, Song F et al (2019) Comparison of breast cancer risk factors among molecular subtypes: a case-only study. Cancer Med 8(4):1882–1892. https://doi.org/10.1002/cam4.2012
Atkinson RL, El-Zein R, Valero V, Lucci A, Bevers TB, Fouad T et al (2016) Epidemiological risk factors associated with inflammatory breast cancer subtypes. Cancer Causes Control 27(3):359–366. https://doi.org/10.1007/s10552-015-0712-3
Puig-Vives M, Sánchez MJ, Sánchez-Cantalejo J, Torrella-Ramos A, Martos C, Ardanaz E et al (2013) Distribution and prognosis of molecular breast cancer subtypes defined by immunohistochemical biomarkers in a Spanish population-based study. Gynecol Oncol 130(3):609–614. https://doi.org/10.1016/j.ygyno.2013.05.039
Arpino G, Milano M, De Placido S (2015) Features of aggressive breast cancer. Breast 24(5):594–600. https://doi.org/10.1016/j.breast.2015.06.001
European Council (2020) Council Recommendation of 2 December 2003 on cancer screening. https://eur-lex.europa.eu/LexUriServ/LexUriServ.do?uri=OJ:L:2003:327:0034:0038:ES:PDF. Accessed 2 March 2020
Independent UK Panel on Breast Cancer Screening (2012) The benefits and harms of breast cancer screening: an independent review. Lancet 380(9855):1778–1786. https://doi.org/10.1016/S0140-6736(12)61611-0
Myers ER, Moorman P, Gierisch JM, Havrilesky LJ, Grimm LJ, Ghate S et al (2015) Benefits and harms of breast cancer screening: a systematic review. JAMA. 314(15):1615. https://doi.org/10.1001/jama.2015.13183
Løberg M, Lousdal ML, Bretthauer M, Kalager M (2015) Benefits and harms of mammography screening. Breast Cancer Res 17(1):63. https://doi.org/10.1186/s13058-015-0525-z
Ponti A, Anttila A, Ronco G, Senore C, Cancer Screening in the European Union (2017) Report on the implementation of the Council. Recommendation on cancer screening. https://ec.europa.eu/health/sites/health/files/major_chronic_diseases/docs/2017_cancerscreening_2ndreportimplementation_en.pdf. Lyon. Accessed March 2020
Smith D, Thomson K, Bambra C, Todd A (2019) The breast cancer paradox: a systematic review of the association between area-level deprivation and breast cancer screening uptake in Europe. Cancer Epidemiol 60:77–85. https://doi.org/10.1016/j.canep.2019.03.008
Alcaraz M, Lluch A, Miranda J, Pereiro I, Salas MD (2002) Study of non-participation in the breast cancer screening program in the city of Valencia (Spain). Gac Sanit 16(3):230–5. https://doi.org/10.1016/S0213-9111(02)71666-X
Esteva M, Ripoll J, Leiva A, Sánchez-Contador C, Collado F (2008) Determinants of non attendance to mammography program in a region with high voluntary health insurance coverage. BMC Public Health 8(1):387. https://doi.org/10.1186/1471-2458-8-387
O’Brien KM, Mooney T, Fitzpatrick P, Sharp L (2018) Screening status, tumour subtype, and breast cancer survival: a national population-based analysis. Breast Cancer Res Treat 172(1):133–142. https://doi.org/10.1007/s10549-018-4877-9
Koh VCY, Lim JCT, Thike AA, Cheok PY, Thu MMM, Tan VKM et al (2015) Characteristics and behaviour of screen-detected ductal carcinoma in situ of the breast: comparison with symptomatic patients. Breast Cancer Res Treat 152(2):293–304. https://doi.org/10.1007/s10549-015-3472-6
Bellio G, Marion R, Giudici F, Kus S, Tonutti M, Zanconati F et al (2017) Interval breast cancer versus screen-detected cancer: comparison of clinicopathologic characteristics in a single-center analysis. Clin Breast Cancer 17(7):564–571. https://doi.org/10.1016/j.clbc.2017.04.001
Cheasley D, Li N, Rowley SM, Elder K, Mann GB, Loi S et al (2019) Molecular comparison of interval and screen-detected breast cancers. J Pathol 248(2):243–252. https://doi.org/10.1002/path.5251
Sprague BL, Gangnon RE, Hampton JM, Egan KM, Titus LJ, Kerlikowske K et al (2015) Variation in breast cancer-risk factor associations by method of detection: results from a series of case-control studies. Am J Epidemiol 181(12):956–969. https://doi.org/10.1093/aje/kwu474
Castaño-Vinyals G, Aragonés N, Pérez-Gómez B, Martín V, Llorca J, Moreno V et al (2015) Population-based multicase-control study in common tumors in Spain (MCC-Spain): rationale and study design. Gac Sanit 29(4):308–315. https://doi.org/10.1016/j.gaceta.2014.12.003
García-Closas R, García-Closas M, Kogevinas M, Malats N, Silverman D, Serra C et al (2007) Food, nutrient and heterocyclic amine intake and the risk of bladder cancer. Eur J Cancer 43(11):1731–1740. https://doi.org/10.1016/j.ejca.2007.05.007
Lope V, Castelló A, Mena-Bravo A, Amiano P, Aragonés N, Fernández-Villa T et al (2018) Serum 25-hydroxyvitamin D and breast cancer risk by pathological subtype (MCC-Spain). J Steroid Biochem Mol Biol 182:4–13. https://doi.org/10.1016/j.jsbmb.2018.04.005
Holm J, Humphreys K, Li J, Ploner A, Cheddad A, Eriksson M et al (2015) Risk factors and tumor characteristics of interval cancers by mammographic density. J Clin Oncol 33(9):1030–1037. https://doi.org/10.1200/JCO.2014.58.9986
Collaborative Group on Hormonal Factors in Breast Cancer (2012) Menarche, menopause, and breast cancer risk: individual participant meta-analysis, including 118 964 women with breast cancer from 117 epidemiological studies. Lancet Oncol 13(11):1141–1151. https://doi.org/10.1016/S1470-2045(12)70425-4
Huergo SA, Vargas FCA, Herrero AA, Soto MÁ-M, Urtasun JA, Cortés ÁA et al (2012) [Spanish Society of Medical Oncology, Guidelines on cancer prevention and diagnostic] 266
Littman AJ, Koepsell TD, Forsberg CW, Boyko EJ, Yancy WS Jr (2011) Preventive care in relation to obesity: an analysis of a large, national survey. Am J Prev Med 41:465–472
Anderson KN, Schwab RB, Martinez ME (2014) Reproductive risk factors and breast cancer subtypes: a review of the literature. Breast Cancer Res Treat 144(1):1–10. https://doi.org/10.1007/s10549-014-2852-7
Vanier A, Leux C, Allioux C, Billon-Delacour S, Lombrail P, Molinié F (2013) Are prognostic factors more favorable for breast cancer detected by organized screening than by opportunistic screening or clinical diagnosis? A study in Loire-Atlantique (France). Cancer Epidemiol 37(5):683–687. https://doi.org/10.1016/j.canep.2013.07.001
Chiarelli AM, Edwards SA, Sheppard AJ, Mirea L, Chong N, Paszat L et al (2012) Favourable prognostic factors of subsequent screen-detected breast cancers among women aged 50–69. Eur J Cancer Prev 21(6):499–506. https://doi.org/10.1097/CEJ.0b013e328350b0f4
Falck AK, Röme A, Fernö M, Olsson H, Chebil G, Bendahl PO et al (2016) St Gallen molecular subtypes in screening-detected and symptomatic breast cancer in a prospective cohort with long-term follow-up: St Gallen molecular subtypes and mode of detection. Br J Surg 103(5):513–523. https://doi.org/10.1002/bjs.10070
Meshkat B, Prichard RS, Al-Hilli Z, Bass GA, Quinn C, O’Doherty A et al (2015) A comparison of clinical–pathological characteristics between symptomatic and interval breast cancer. Breast 24(3):278–282. https://doi.org/10.1016/j.breast.2015.02.032
Hofvind S, Holen Å, Román M, Sebuødegård S, Puig-Vives M, Akslen L (2016) Mode of detection: an independent prognostic factor for women with breast cancer. J Med Screen 23(2):89–97. https://doi.org/10.1177/0969141315604006
Gray JM, Rasanayagam S, Engel C, Rizzo J (2017) State of the evidence 2017: an update on the connection between breast cancer and the environment. Environ Health 16(1):94. https://doi.org/10.1186/s12940-017-0287-4
Gram IT, Park S-Y, Maskarinec G, Wilkens LR, Haiman CA, Le Marchand L (2019) Smoking and breast cancer risk by race/ethnicity and oestrogen and progesterone receptor status: the Multiethnic Cohort (MEC) study. Int J Epidemiol 48(2):501–511. https://doi.org/10.1093/ije/dyy290
Bjerkaas E, Parajuli R, Engeland A, Maskarinec G, Weiderpass E, Gram IT (2014) The association between lifetime smoking exposure and breast cancer mortality—results from a Norwegian cohort. Cancer Med 3(5):1448–1457. https://doi.org/10.1002/cam4.304
Gaudet MM, Carter BD, Brinton LA, Falk RT, Gram IT, Luo J et al (2016) Pooled analysis of active cigarette smoking and invasive breast cancer risk in 14 cohort studies. Int J Epidemiol. https://doi.org/10.1093/ije/dyw288
Gram IT, Little MA, Lund E, Braaten T (2016) The fraction of breast cancer attributable to smoking: the Norwegian women and cancer study 1991–2012. Br J Cancer 115(5):616–623. https://doi.org/10.1038/bjc.2016.154
Romieu I, Ferrari P, Chajès V, de Batlle J, Biessy C, Scoccianti C et al (2017) Fiber intake modulates the association of alcohol intake with breast cancer. Int J Cancer 140(2):316–321. https://doi.org/10.1002/ijc.30415
Shield KD, Soerjomataram I, Rehm J (2016) Alcohol use and breast cancer: a critical review. Alcohol Clin Exp Res 40(6):1166–1181. https://doi.org/10.1111/acer.13071
Jung S, Wang M, Anderson K, Baglietto L, Bergkvist L, Bernstein L et al (2016) Alcohol consumption and breast cancer risk by estrogen receptor status: in a pooled analysis of 20 studies. Int J Epidemiol 45(3):916–928. https://doi.org/10.1093/ije/dyv156
Liu Y, Nguyen N, Colditz GA (2015) Links between Alcohol Consumption and Breast Cancer: A Look at the Evidence. Women Health (Lond Engl) 11(1):65–77. https://doi.org/10.2217/WHE.14.62
Acknowledgments
The authors thank all patients and families for their participation in the MCC-Spain study, as well as all study centers and collaborators.
Funding
This research was supported by Acción Transversal del Cáncer, approved by the Spanish Council of Ministeres on the 11th October 2007, by the Carlos III Health Institute-FEDER (PI08/1770, PI08/0533, PI08/1359, PS09/00773, PS09/01286, PS09/01903, PS09/02078, PS09/ 01662, PI11/01403, PI11/01889-FEDER, PI11/00226, PI11/01810, PI11/02213, PI12/00488, PI12/00265, PI12/01270, PI12/00715, PI12/00150, PI14/01219, PI14/0613, PI15/00069, PI15/00914, PI15/01032, PI11/01810, PI14/01219, PI11/02213, PIE16/00049, PI17/01179, PI17-00092), by the Fundación Marqués de Valdecilla (API 10/09), by the ICGC International Cancer Genome Consortium CLL (the ICGC CLL-Genome Project is funded by the Spanish Ministry of Economy and Competitiveness through the Carlos III Health Institute (ISCIII)), by the ISCIII Red Temática de Investigación del Cáncer (RTICC) (RD12/0036/0036), by the Regional Government of Castile and León (LE22A10-2), by the Regional Health Ministry of Andalusia (PI-0571–2009, PI-0306–2011, salud201200057018tra), by the Regional Health Ministry of Valencia (AP_061/10), by Recercaixa (2010ACUP00310), by the Regional Government of the Basque Country, by the Regional Health Ministry of Murcia, by the European Commission (grants FOOD-CT-2006–036224-HIWATE), by the Spanish Association Against Cancer (AECC) Scientific Foundation (GCTRA18022MORE), by the Catalan Regional Government Agency for Management of University and Research Grants (AGAUR) (2014SGR647, 2014SGR850, and 2017SGR723), by the Fundación Caja de Ahorros de Asturias and by the University of Oviedo. ISGlobal is a member of the CERCA Programme, Regional Government of Catalonia. Sample collection was supported by the Carlos III Health Institute- FEDER: Parc de Salut MAR Biobank (MARBiobanc) (RD09/0076/00036), the La Fe Biobank (PT17/0015/0043RD 09 0076/00021), and the FISABIO Biobank (PT17/0015/0017) RD09 0076/00058); the Public Health Laboratory of Gipuzkoa, the Basque Biobank, ICOBIOBANC (sponsored by the Catalan Institute of Oncology), the IUOPA Biobank from the University of Oviedo and ISCIII Biobank. The Spanish National Genotyping Centre (CEGEN-ISCIII) provided SNPs genotyping services. We would like to thank all those who participated in the study and all MCC-Spain study groups and collaborators.
Author information
Authors and Affiliations
Contributions
AM-B, MP, MK, and DS conceptualized and designed the study. MH-G, AM-B, MV-E, and DS developed the methodology. BP, NA, PA, JMA, GC-V, MS, ME, VM, IG-A, CV, AT, RM-G, MP, MK, and DS participated in the acquisition of data. MH-G, AM-B, MV-E, ÓZ, BP, NA, PA, JMA, GC-V, MS, ME, VM, IG-A, CV, AT, RM-G, MP, MK, and DS analyzed and interpreted the data. MH-G, AM-B, MV-E, ÓZ, BP, NA, PA, JMA, GC-V, MS, ME, VM, IG-A, CV, AT, RM-G, MP, MK, and DS wrote and/or revised the manuscript. DS, AM-B, and ÓZ supervised the study.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interests related to this study. They state that they have no affiliations with and are not involved in any organization or entity with financial (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements), or non-financial interests (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript.
Ethical approval
The MCC-Spain study followed national and international directives on ethics and data protection (the Declaration of Helsinki and Spanish law on data confidentiality, Organic Law 15/1999 of 13 December on the Protection of Personal Data—LOPD) and meets the requirements of current legislation. The MCC-Spain study protocol was approved by the ethics committees of participating institutions.
Consent to participate
All participants provided informed consent.
Consent for publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Hernández-García, M., Molina-Barceló, A., Vanaclocha-Espi, M. et al. Differences in breast cancer-risk factors between screen-detected and non-screen-detected cases (MCC-Spain study). Cancer Causes Control 33, 125–136 (2022). https://doi.org/10.1007/s10552-021-01511-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10552-021-01511-4