Abstract
Purpose
Inflammatory breast cancer (IBC) is a rare, poorly understood and aggressive tumor. We extended prior findings linking high body mass index (BMI) to substantial increased IBC risk by examining BMI associations before and after adjustment for well-characterized comorbidities using medical record data for diabetes, insulin resistance, and disturbances of cholesterol metabolism in a general community healthcare setting.
Methods
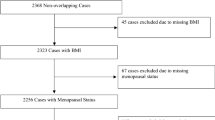
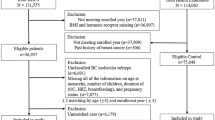
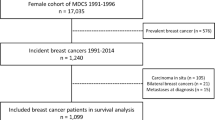
We identified 247 incident IBC cases diagnosed at Kaiser Permanente Northern California between 2005 and 2017 and 2470 controls matched 10:1 on birth year and geographic area and with ≥ 13 months of continuous enrollment prior to diagnosis/index date. We assessed exposures from 6 years up to one year prior to the diagnosis/index date, using logistic regression to calculate odds ratios (ORs) with 95% confidence intervals (CIs).
Results
Before adjustment for comorbidities, ORs (95% CIs) for BMI of 25–< 30, 30–< 35, and ≥ 35 compared to < 25 kg/m2 were 1.5 (0.9–2.3), 2.0 (1.2–3.1), and 2.5 (1.4–4.4), respectively. After adjustment for pre-diabetes/diabetes, HDL-C and triglyceride levels, and dyslipidemia, corresponding ORs were 1.3 (0.8–2.1), 1.6 (0.9–2.9), and 1.9 (1.0–3.5). The OR for HDL-C levels < 50 mg/dL compared to ≥ 65 mg/dL was 2.0 (1.2–3.3) in the adjusted model. In a separate model the OR for a triglyceride/HDL-C ratio ≥ 2.50 compared to < 1.62 was 1.7 (1.1–2.8) after adjustment for BMI, pre-diabetes/diabetes, and dyslipidemia. Results did not differ significantly by estrogen receptor status.
Conclusions
Obesity and measures of insulin resistance independently increased IBC risk as did obesity and low HDL-C levels. These findings, if confirmed, have implications for IBC prevention.
Similar content being viewed by others
Data availability
The data in this manuscript were sourced from electronic health records and related clinical and administrative data sources from Kaiser Permanente Northern California, and are not generally available to the public. These data may be made available through scientific collaborations under IRB-approved protocols and data use agreements.
Abbreviations
- IBC:
-
Inflammatory breast cancer
- KPNC:
-
Kaiser Permanente Northern California
- KPNCCR:
-
Kaiser Permanente Northern California Cancer Registry
- BMI:
-
Body mass index
- ER:
-
Estrogen receptor
- ICD:
-
International Classification of Disease
- OR:
-
Odds ratio
- CI:
-
Confidence interval
- HDL-C:
-
High-density lipoprotein cholesterol
- VEGF:
-
Vascular endothelial growth factor
References
Anderson WF, Schairer C, Chen BE, Hance KW, Levine PH (2005) Epidemiology of inflammatory breast cancer (IBC). Breast Dis 22:9–23
Greene FL, Page DL, Fritz A, Balch CM, Haller DG, Morrow M (2002) Breast. AJCC cancer staging manual, 6th edn. Springer-Verlag, New York, pp 225–226
Hance KW, Anderson WF, Devesa SS, Young HA, Levine PH (2005) Trends in inflammatory breast cancer incidence and survival: the Surveillance, Epidemiology, and End Results Program at the National Cancer Institute. J Natl Cancer Inst 97:966–974
Amiri-Kordestani L, Kamangar F, Zujewski JA (2013) Inflammatory breast cancer: yet another risk of the obesity epidemic? J Natl Cancer Inst 105:1340–1342
Schairer C, Li Y, Frawley P, Graubard BI, Wellman RD, Buist DS, Kerlikowske K, Onega TL, Anderson WF, Miglioretti DL (2013) Risk factors for inflammatory breast cancer and other invasive breast cancers. J Natl Cancer Inst 105:1373–1384
Chang S, Buzdar AU, Hursting SD (1998) Inflammatory breast cancer and body mass index. J Clin Oncol 16:3731–3735
Atkinson RL, El-Zein R, Valero V, Lucci A, Bevers TB, Fouad T, Liao W, Ueno NT, Woodward WA, Brewster AM (2016) Epidemiological risk factors associated with inflammatory breast cancer subtypes. Cancer Causes Control 27:359–366
Suzuki R, Orsini N, Saji S, Key TJ, Wolk A (2009) Body weight and incidence of breast cancer defined by estrogen and progesterone receptor status – A meta-analysis. Int J Cancer 124:698–712
Varmus H, Harlow E (2012) Provocative questions in cancer research. Nature 481:436–437
Matthews SB, Thompson HJ (2016) The obesity-breast cancer conundrum: an analysis of the issues. Int J Mol Sci 17:989
Rose DP, Gracheck PJ, Vona-Davis L (2015) The interactions of obesity, inflammation and insulin resistance in breast cancer. Cancers 7:2147–2168
Ni H, Liu H, Gao R (2015) Serum lipids and breast cancer risk: a meta-analysis of prospective cohort studies. PLoS ONE 10(11):e0142669. https://doi.org/10.1371/journal.pone.0142669
De Bruijn KM, Arends LR, Hansen BE, Leeflang S, Ruiter R, van Eijck CH (2013) Systematic review and meta-analysis of the association between diabetes mellitus and incidence and mortality in breast and colorectal cancer. Br J Surg 100:1421–1429
Huang Y, Cai X, Qiu M, Chen P, Tang H, Hu Y, Huang Y (2014) Prediabetes and the risk of cancer: a meta-analysis. Diabetologia 57:2261–2269
Boyle P, Koechlin A, Pizot C, Boniol M, Robertson C, Mullie P, Bolli G, Rosenstock J, Autier P (2013) Blood glucose concentrations and breast cancer risk in women without diabetes: a meta-analysis. Eur J Nutr 52:1533–1540
Esposito K, Chiodini P, Capuano A, Bellastella G, Maiorino MI, Rafaniello C, Giugliano D (2013) Metabolic syndrome and postmenopausal breast cancer: systematic review and meta-analysis. Menopause 20:1301–1309
Touvier M, Fassier P, His M, Norat T, Chan DS, Blacher J, Hercberg S, Galan P, Druesne-Pecollo N, Latino-Martel P (2015) Cholesterol and breast cancer risk: a systematic review and meta-analysis of prospective studies. Br J Nutr 114:347–357
Autier P, Koechlin A, Boniol M, Mullie P, Bolli G, Rosenstock J, Boyle P (2013) Serum insulin and c-peptide concentration and breast cancer: a meta-analysis. Cancer Causes Control 24:873–883
Hernandez AV, Guarnizo M, Miranda Y, Pasupuleti V, Deshpande A, Paico S, Lenti H, Ganoza S, Montalvo L, Thota P, Lazaro H (2014) Association between insulin resistance and breast carcinoma: a systematic review and meta-analysis. PLoS ONE 9(6):e99317. https://doi.org/10.1371/journal.pone.0099317
Schairer C, Gadalla SM, Pfeiffer RM, Moore SC, Engels EA (2017) Diabetes, abnormal glucose, dyslipidemia, hypertension, and risk of inflammatory and other breast cancer. Cancer Epidemiol Biomark Prev 26:862–868
Nichols GA, Desai J, Lafata JE, Lawrence JM, O’Connor PJ, Pathak RD, Raebel MA, Reid RJ, Selby JV, Silverman BG, Steiner JF, Stewart WF, Vupputuri S, Waitzfelder B, SUPREME-DM Study Group (2012) Construction of a multisite datalink using electronic health records for the identification, surveillance, prevention, and management of diabetes mellitus: the SUPREME-DM Project. Prev Chronic Dis. https://doi.org/10.5888/pcd9.110311
Koebnick C, Smith N, Huang K, Martinez MP, Clancy HA, Kushi LH (2012) The prevalence of obesity and obesity-related health conditions in a large, multiethnic cohort of young adults in California. Ann Epidemiol 22:609–616
McKeever K, Saydah SH, Imperatore G, Cowie CC, Gregg EW, Geiss LS, Cheng YJ, Rolka DB, Williams DE, Caspersen CJ (2013) Secular changes in U.S. prediabetes prevalence defined by hemoglobin A1c and fasting plasma glucose. Diabetes Care 36:2286–2293
Schmittdiel JA, Dyer WT, Marshall CJ, Bivins R (2018) Using neighborhood-level census data to predict diabetes progression in patients with laboratory-defined prediabetes. Perm J 22:18–096
Raghunathan TE, Lepkowski JM, van Hoewyk M, Solenberger PW (2001) A multivariate technique for multiply imputing missing values using a sequence of regression models. Survey Methodol 27:85–95
Priya G, Kalra S (2018) A review of insulin resistance in type I diabetes: is there a place for adjunctive metformin? Diabetes Ther 9:341–361
Hostalek U, Gwilt M, Hildemann S (2015) Therapeutic use of metformin in prediabetes and diabetes prevention. Drugs 75:1071–1094
Ojha A, Ojha U, Mohammed R, Chandrashekar A, Ojha H (2019) Current perspective on the role of insulin and glucagon in the pathogenesis and treatment of type 2 diabetes. Clin Pharm 11:57–65
Scappaticcio L, Maiorino MI, Bellastella G, Giugliano D, Esposito K (2017) Insights into the relationships between diabetes, prediabetes, and cancer. Endocrine 56:231–239
Garcia-Estevez L, Moreno-Bueno G (2019) Updating the role of obesity and cholesterol in breast cancer. Breast Cancer Res 21:35
Vermeulen PB, van Golen KL, Dirix LY (2010) Angiogenesis, lymphangiogenesis, growth pattern, and tumor emboli in inflammatory breast cancer: a review of current knowledge. Cancer 116(Suppl 11):2748–2754
Morrow RJ, Etemadi N, Yeo B, Ernst M (2017) Challenging a misnomer? The role of inflammatory pathways in inflammatory breast cancer. Mediators Inflamm. https://doi.org/10.1155/2017/4754827
Kolb R, Sutterwala FS, Weizhou Z (2016) Obesity and cancer: inflammation bridges the two. Curr Opin Pharmacol 29:77–89
Ahmadieh H, Azar ST (2013) Type 2 diabetes mellitus, oral diabetic medications, insulin therapy, and overall breast cancer risk. ISRN Endocrinol. https://doi.org/10.1155/181240
Schairer C, Freedman DM, Gadalla SM, Pfeiffer RM (2018) Dyslipidemia, lipid-lowering drug use and breast cancer risk in the SEER-Medicare database. Breast Cancer Res Treat 169:607–614
Acknowledgements
This work was supported by the National Cancer Institute at the National Institutes of Health Intramural Research Program and in part by NCI Grant U24 CA171524.
Funding
Division of Cancer Epidemiology and Genetics, National Cancer Institute. Division of Cancer Prevention, National Cancer Institute (U24).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Ethical approval
This project was reviewed and approved by the KPNC Institutional Review Board (Protocol number: 1285916).
Informed consent
The requirement to obtain informed consent for this data-only project was waived.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Schairer, C., Laurent, C.A., Moy, L.M. et al. Obesity and related conditions and risk of inflammatory breast cancer: a nested case–control study. Breast Cancer Res Treat 183, 467–478 (2020). https://doi.org/10.1007/s10549-020-05785-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-020-05785-1