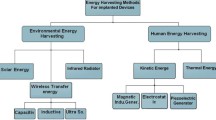
This review addresses questions of the specific characteristics of power supply to implanted devices (ID), including the service life of supply elements and the level of power consumption of contemporary devices, the acceptable weight and size characteristics of ID, and priority areas for implantation. Known methods of energy transmission and transformation are compared and the ranges of potential specific power for these are determined −0.1-100 mW/cm2 for wireless energy transmission, 0.0001-0.1 mW/cm2 for transformation of energy for sources specific to biological objects, and less than 0.0001 mW/cm2 for isotope power sources.
Similar content being viewed by others
References
Caldara, M., Nodari, B., Re, V., and Bonandrini, B., “Miniaturized blood pressure telemetry system with RFID interface,” Electronics, 5, 51 (2016).
Zeng, F.-G., Rebscher, S., Harrison, W., Sun, X., and Feng, H., “Cochlear implants: System design, integration, and evaluation,” IEEE Rev. Biomed. Eng., 1, 115-142 (2008).
Mestais, C. S., Charvet, G., Sauter-Starace, F., Foerster, M., Ratel, D., and Benabid, A. L., “WIMAGINE: Wireless 64-channel ECoG recording implant for long term clinical applications,” IEEE Trans. Neural Syst. Rehabil. Eng., 23, No. 1, 10-21 (2015).
Borton, D. A., Yin, M., Aceros, J., and Nurmikko, A., “An implantable wireless neural interface for recording cortical circuit dynamics in moving primates,” J. Neural Eng., 10, No. 2 (2013).
Medtronic Micra Clinician Manual, https://www.accessdata.fda.gov/cdrh-docs/pdf15/P150033d.pdf.
Uddin, K., Perera, S., Widanage, W. D., Somerville, L., and Marco, J., “Characterising lithiumion battery degradation through the identification and tracking of electrochemical battery model parameters,” Batteries, 2, 13 (2016).
Medical Power Sources, https://integer.net/product/medical-power-sources-crm/.
Xu, B., Oudalov, A., Ulbig, A., Andersson, G., and Kirschen, D. S., “Modeling of lithiumion battery degradation for cell life assessment,” IEEE Trans. Smart Grid, No. 99. P. 1 (2016).
Li, J., Murphy, E., Winnick, J., and Kohl, P. A., “The effects of pulse on cycling characteristics of commercial lithiumion batteries,” J. Power Sources, 102, No. 1, 302-309 (2001).
Chang, W.-Y., “The state of charge estimating methods for battery: A review,” ISRN Applied Mathematics, 2013, 7 (2013).
Schuler, B., Rettich, A., Vogel, J., Gassmann, M., and Arras, M., “Optimized surgical techniques and postoperative care improve survival rates and permit accurate telemetric recording in exercising mice,” BMC Vet. Res., 5, 28 (2009).
Helwig, B. G., Blaha, M. D., and Leon, L. R., “Effect of intraperitoneal radiotelemetry instrumentation on voluntary wheel running and surgical recovery in mice,” J. Am. Assoc. Lab. Anim. Sci., 51, No. 5, 600-608 (2012).
Guidelines fort the Experimental (Preclinical) Study of Novel Pharmacological Substances, Corresponding Member of the Russian Academy of Medical Sciences Professor R. U. Khabriev (general editor), Meditsina, Moscow (2005).
DSI Implantable Telemetry Brochure, http://www.datasci.com/.
Medtronic Activa RC Model 37612 Multi-Program Rechargeable Neurostimulator Implant Manual, http://manuals.medtronic.com.
Boston Scientific Precision Spinal Cord Stimulator System Clinician Manual, https://www.bostonscientific.com/.
Rajappan, K., “Permanent pacemaker implantation technique. Part I,” Heart, 95, 259-264 (2009).
Revishvili, A. Sh., et al., Arrhythmology: Clinical Guidelines for Electrophysiological Investigations, Catheter Ablation, and the Use of Implanted Antiarrhythmic Devices [in Russian], Geotar Media, Moscow (2010).
Kotsakou, M., Kioumis, I., and Lazaridis, G., “Pacemaker insertion,” Ann. Transl. Med., 3, No. 3, 42 (2015).
Moons, C. P. H., Hermans, K., Remie, R., Duchateau, L., and Odberg, F. O., “Intraperitoneal versus subcutaneous telemetry devices in young Mongolian gerbils (Meriones unguiculatus),” Lab. Anim., 41, No. 2, 262-271 (2007).
Ahn, D. and Hong, S., “Wireless power transmission with self-regulated output voltage for biomedical implant,” IEEE Trans. Industrial Electronics, 61, No. 5, 2225-2235 (2014).
Artan, N., Hitesh, V., Gurudath, V., Fu Zhen, Santosh, B., Nandor, L., Medveczky, G, and Chao, H., “A high-performance transcutaneous battery charger for medical implants. 2010 Conference Proceedings,” IEEE Eng. Med. Biol. Soc., 1, 1581-1584 (2010).
Jegadeesan, R., Nag, S., Agarwal, K., Thakor, N. V., and Yong-Xin, G., “Enabling wireless powering and telemetry for peripheral nerve implants,” IEEE J. Biomed. Health Inf., 19, No. 3, 958-970 (2015).
Young, D. J., Cong, P., Suster, M. A., and Damaser, M., “Implantable wireless battery recharging system for bladder pressure chronic monitoring,” Lab. Chip, 15, 4338-4347 (2015).
Sodagar, A. and Amiri, P., “Capacitive coupling for power and data telemetry to implantable biomedical microsystems,” in: NER ’09. 4th International IEEE/EMBS Conference (2009), pp. 411-414.
Liu, X., Berger, J. L., Ogirala, A., and Mickle, M. H., “A touch probe method of operating an implantable RFID tag for orthopedic implant identification,” Biomedical Circuits and Systems, IEEE Transactions, 7, No. 3, 236-242 (2013).
Chow, E. Y., Chlebowski, A. L., Chakraborty, S., Chappell, W. J., and Irazoqui, P. P., “Fully wireless implantable cardiovascular pressure monitor integrated with a medical stent,” IEEE Trans. Biomed. Eng., 57, No. 6, 1487-1496 (2010).
Ho, J. S., Yeh, A. J., Neofytou, E., Kim, S., Tanabe, Y., Patlolla, B., Beygui R. E., and Poon, A. S. Y., “Wireless power transfer to deep-tissue microimplants,” Proc. Nat. Acad. Sci. USA, 111, No. 22, 7974-7979 (2014).
Liu, C., Guo Y.-X., Sun, H., and Xiao S., “Design and safety considerations of an implantable rectenna for far-field wireless power transfer,” IEEE Trans. Antennas Propag., 62, No. 11, 5798-5806 (2014).
Murakawa, K., Kobayashi, M., Nakamura, O., and Kawata, S. A., “Wireless near-infrared energy system for medical implants,” IEEE Eng. Med. Biol. Mag., 18, 70-72 (1999).
Goto, K., Nakagawa, T., Nakamura, O., and Kawata, S., “An implantable power supply with an optically rechargeable lithium battery,” IEEE Trans. Biomed. Eng., 48, 830-833 (2001).
Liu, H., Zhao, T., Jiang, W., Jia, R., Niu, D., Qiu, G., Fan, L., Li, X., Liu, W., Chen, B., Shi, Y., Yin, L., and Lu, B., “Flexible battery-less bioelectronic implants: wireless powering and manipulation by near-infrared light,” Adv. Funct. Mater., 25, 7071 (2015).
Mazzilli, F., Peisino, M., Mitouassiwou, R., Cottй, B., Thoppay, P., Lafon, C., Favre, P., Meurville, E., and Dehollain, C., “In-vitro platform to study ultrasound as source for wireless energy transfer and communication for implanted medical devices,” Conf. Proc. IEEE Eng. Med. Biol. Soc., 2010, 3751-3755 (2010).
Ozeri, S., Shmilovitz, D., Singer, S., and Wang, C., “Ultrasonic transcutaneous energy transfer using a continuous wave 650 kHz Gaussian shaded transmitter,” Ultrasonics, 50, 666-674 (2010).
Maleki, T., Cao, N., Song, S. H., Kao, C., Ko, S. C. A., and Ziaie, B., “An ultrasonically powered implantable micro-oxygen generator (IMOG),” IEEE Trans. Biomed. Eng., 58, No. 11, 3104-3111 (2011).
Dagdeviren, C., et al., “Conformal piezoelectric energy harvesting and storage from motions of the heart, lung, and diaphragm,” Proc. Natl. Acad. Sci. USA, 111, No. 5, 1927-1932 (2014).
Tashiro, R., Kabei, N., Katayama, K., Ishizuka, Y., Tsuboi, F., and Tsuchiya, K., “Development of an electrostatic generator that harnesses the motion of a living body,” Int. J. Jpn. Soc. Mechan. Eng., 43, 916-922 (2000).
Miao, P., Mitcheson, P., Holmes, A., Yeatman, E., Green, T., and Stark, B., “MEMS inertial power generators for biomedical applications,” Microsyst. Technol., 12, No. 10-11, 1079-1083 (2006).
Goto, H., Sugiura, T., Harada, Y., and Kazui, T., “Feasibility of using the automatic generating system for quartz watches as a lead-less pacemaker power source,” Med. Biol. Eng. Comput., 37, No. 1, 377-380 (1999).
Stark, I. and Stordeur, M., “New micro thermoelectric devices based on bismuth telluride-type thin solid films,” in: Proc. 18th Int. Conf. Thermoelectric (1999), pp. 465-472.
Strasser, M., Aigner, R., Lauterbach, C., Sturm, T. F., Franosch, M., and Wachutka, G., “Micromachined CMOS thermoelectric generators as on-chip power supply,” Sensors Actuators A. Phys., 114, No. 2-3, 362-370 (2004).
Chen, G., Ghaed, H., Haque, R., Wieckowski, M., Yejoong Kim, Gyouho Kim, Fick, D., Daeyeon Kim, Mingoo Seok, Wise, K., Blaauw, D., and Sylvester, D., “A cubic-millimeter energy-autonomous wireless intraocular pressure monitor,” IEEE International Solid-State Circuits Conference (2011), pp. 310-312.
Drake, R., Kusserow, B., Messinger, S., and Matsuda S., “A tissue implantable fuel cell power supply,” ASAIO J., 16, No. 1, 199-205 (1970).
Weidlich, E., Richter, G., von Sturm, F., and Rao, J. R., “Animal experiments with biogalvanic and biofuel cells,” Biomaterials, Medical Devices, and Artificial Organs, No. 3-4, 227-306 (1976).
Rapoport, B. I., Kedzierski, J. T., and Sarpeshkar, R., “A glucose fuel cell for implantable brain-machine interfaces,” PLoS ONE, 7, No. 6 (2012).
Dong, K., Jia, B., Yu, C., Dong, W., Du, F., and Liu, H., “Microbial fuel cell as power supply for implantable medical devices: A novel configuration design for simulating colonic environment,” Biosens. Bioelectron., 41, 916-919 (2013).
Mercier, P. P., Lysaght, A. C., Bandyopadhyay, S., Chandrakasan, A. P., and Stankovic, K. M., “Energy extraction from the biologic battery in the inner ear,” Nat. Biotechnol., 30, No. 12, 1240-1243 (2012).
Widetronix, http://www.widetronix.com/.
City Labs, http://www.citylabs.net/.
Drews, J., Fehrmann, G., Staub, R., and Wolf, R., “Primary batteries for implantable pacemakers and defibrillators,” J. Power Sour., 97, 747-749 (2001).
Mallela, V. S., Ilankumaran, V., and Rao, N. S., “Trends in cardiac pacemaker batteries,” Indian Pacing Electrophysiol. J., 4, 201 (2004).
RamRakhyani, A. K. and Lazzi, G., “Multicoil telemetry system for compensation of coil misalignment effects in implantable systems,” IEEE Antennas and Wireless Propagation Letters, 11, 1675-1678 (2012).
Qusba, A., RamRakhyani, A. K., So, J., Hayes, G. J., Dickey, M. D., and Lazzi, G., “On the design of microfluidic implant coil for flexible telemetry system,” IEEE Sensors J., 14, No. 4, 1074-1080 (2014).
Denisov, A. and Yeatman, E., “Ultrasonic vs. inductive power delivery for miniature biomedical implants,” in: 2010 Int. Conf. on Body Sensor Networks (2010), pp. 84-89.
Jegadeesan, R., Guo, Y.-X., and Minkyu, J., “Electric near-field coupling for wireless power transfer in biomedical applications,” in: Proc. IEEE MTTS Int. Microw. Workshop Ser. RF Wireless Technol. Biomed. Healthcare Appl. (2013), pp. 1-3.
Author information
Authors and Affiliations
Corresponding author
Additional information
Translated from Meditsinskaya Tekhnika, Vol. 52, No. 3, May-Jun., 2018, pp. 43-47.
Rights and permissions
About this article
Cite this article
Gorskii, O.V. Potential Power Supply Methods for Implanted Devices. Biomed Eng 52, 204–209 (2018). https://doi.org/10.1007/s10527-018-9814-z
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10527-018-9814-z