Abstract
Computational fluid dynamics (CFD) is widely used to simulate blood-contacting medical devices. To be relied upon to inform high-risk decision making, however, model credibility should be demonstrated through validation. To provide robust data sets for validation, researchers at the FDA and collaborators developed two benchmark medical device flow models: a nozzle and a centrifugal blood pump. Experimental measurements of the flow fields and hemolysis were acquired using each model. Concurrently, separate open interlaboratory CFD studies were performed in which participants from around the world, who were blinded to the measurements, submitted CFD predictions of each benchmark model. In this study, we report the results of the interlaboratory CFD study of the FDA benchmark blood pump. We analyze the results of 24 CFD submissions using a wide range of different flow solvers, methods, and modeling parameters. To assess the accuracy of the CFD predictions, we compare the results with experimental measurements of three quantities of interest (pressure head, velocity field, and hemolysis) at different pump operating conditions. We also investigate the influence of different CFD methods and modeling choices used by the participants. Our analyses reveal that, while a number of CFD submissions accurately predicted the pump performance for individual cases, no single participant was able to accurately predict all quantities of interest across all conditions. Several participants accurately predicted the pressure head at all conditions and the velocity field in all but one or two cases. Only one of the eight participants who submitted hemolysis results accurately predicted absolute plasma free hemoglobin levels at a majority of the conditions, though most participants were successful at predicting relative hemolysis levels between conditions. Overall, this study highlights the need to validate CFD modeling of rotary blood pumps across the entire range of operating conditions and for all quantities of interest, as some operating conditions and regions (e.g., the pump diffuser) are more challenging to accurately predict than others. All quantities of interest should be validated because, as shown here, it is possible to accurately predict hemolysis despite having relatively inaccurate predictions of the flow field.

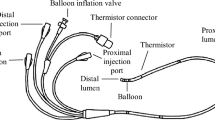
Adapted from Hariharan et al.16










Similar content being viewed by others
References
ASME V&V 40-2018. Assessing Credibility of Computational Modeling Through Verification and Validation: Application to Medical Devices. New York, NY: American Society of Mechanical Engineers, 2018.
Aycock, K. I., R. L. Campbell, F. C. Lynch, K. B. Manning, and B. A. Craven. The importance of hemorheology and patient anatomy on the hemodynamics in the inferior vena cava. Ann. Biomed. Eng. 44:3568–3582, 2016.
Aycock, K. I., R. L. Campbell, F. C. Lynch, K. B. Manning, and B. A. Craven. Computational predictions of the embolus-trapping performance of an IVC filter in patient-specific and idealized IVC geometries. Biomech. Model. Mechanobiol. 16:1957–1969, 2017.
Aycock, K. I., R. L. Campbell, K. B. Manning, S. P. Sastry, S. M. Shontz, F. C. Lynch, and B. A. Craven. A computational method for predicting inferior vena cava filter performance on a patient-specific basis. J. Biomech. Eng.136:081003, 2014.
Bianchi, M., G. Marom, R. P. Ghosh, O. M. Rotman, P. Parikh, L. Gruberg, and D. Bluestein. Patient-specific simulation of transcatheter aortic valve replacement: impact of deployment options on paravalvular leakage. Biomech. Model. Mechanobiol. 18:435, 2018.
Chiastra, C., S. Morlacchi, D. Gallo, U. Morbiducci, R. Cardenes, I. Larrabide, and F. Migliavacca. Computational fluid dynamic simulations of image-based stented coronary bifurcation models. J. R. Soc. Interface. 10:20130193–20130193, 2013.
Craven, B. A., K. I. Aycock, L. H. Herbertson, and R. A. Malinauskas. A CFD-based Kriging surrogate modeling approach for predicting device-specific hemolysis power law coefficients in blood-contacting medical devices. Biomech. Model. Mechanobiol. 18:1005–1030, 2019.
Craven, B. A., M. M. Faghih, K. I. Aycock, and E. M. Kolahdouz. A Poisson equation method for prescribing fully developed non-Newtonian inlet conditions for computational fluid dynamics simulations in models of arbitrary cross-section. Math. Comput. Simul. 194:523–538, 2022.
Dixon, S. L., and C. A. Hall. Fluid Mechanics and Thermodynamics of Turbomachinery. Oxford: Butterworth-Heinemann, 2010.
Elkins, C. J., and M. T. Alley. Magnetic resonance velocimetry: applications of magnetic resonance imaging in the measurement of fluid motion. Exp. Fluids. 43:823–858, 2007.
Elkins, C., M. Markl, N. Pelc, and J. Eaton. 4D Magnetic resonance velocimetry for mean velocity measurements in complex turbulent flows. Exp. Fluids. 34:494–503, 2003.
FDA. Reporting of Computational Modeling Studies in Medical Device Submissions: Guidance for Industry and Food and Drug Administration Staff. https://www.fda.gov/media/87586/download, 2016.
Fraser, K. H., T. Zhang, M. Ertan Taskin, B. P. Griffith, and Z. J. Wu. A quantitative comparison of mechanical blood damage parameters in rotary ventricular assist devices: shear stress, exposure time and hemolysis index. J. Biomech. Eng. 134:081002, 2012.
Good, B. C., and K. B. Manning. Computational modeling of the Food and Drug Administration’s benchmark centrifugal blood pump. Artif. Organs. 44:E263–E276, 2020.
Gundert, T. J., A. L. Marsden, W. Yang, and J. F. LaDisa. Optimization of cardiovascular stent design using computational fluid dynamics. J. Biomech. Eng.134:011002, 2012.
Hariharan, P., K. I. Aycock, M. Buesen, S. W. Day, B. C. Good, L. H. Herbertson, U. Steinseifer, K. B. Manning, B. A. Craven, and R. A. Malinauskas. Inter-laboratory characterization of the velocity field in the FDA blood pump model using particle image velocimetry (PIV). Cardiovasc. Eng. Technol. 9:623–640, 2018.
Hariharan, P., M. Giarra, V. Reddy, S. W. Day, K. B. Manning, S. Deutsch, S. F. Stewart, M. R. Myers, M. R. Berman, G. W. Burgreen, E. G. Paterson, and R. A. Malinauskas. Multilaboratory particle image velocimetry analysis of the FDA benchmark nozzle model to support validation of computational fluid dynamics simulations. J. Biomech. Eng.133:041002, 2011.
Herbertson, L. H., S. E. Olia, A. Daly, C. P. Noatch, W. A. Smith, M. V. Kameneva, and R. A. Malinauskas. Multilaboratory study of flow-induced hemolysis using the FDA benchmark nozzle model. Artif. Organs. 39:237–248, 2015.
ISO 14708-5:2020. Implants for Surgery—Active Implantable Medical Devices—Part 5: Circulatory Support Devices. Geneva, CH: International Organization for Standardization, 2020.
Kheradvar, A., E. M. Groves, A. Falahatpisheh, M. K. Mofrad, S. H. Alavi, R. Tranquillo, L. P. Dasi, C. A. Simmons, K. J. Grande-Allen, C. J. Goergen, F. Baaijens, S. H. Little, S. Canic, and B. Griffith. Emerging trends in heart valve engineering: part IV. Computational modeling and experimental studies. Ann. Biomed. Eng. 43:2314–2333, 2015.
Lee, J. H., A. D. Rygg, E. M. Kolahdouz, S. Rossi, S. M. Retta, N. Duraiswamy, L. N. Scotten, B. A. Craven, and B. E. Griffith. Fluid-structure interaction models of bioprosthetic heart valve dynamics in an experimental pulse duplicator. Ann. Biomed. Eng. 48:1475–1490, 2020.
Malinauskas, R. A., P. Hariharan, S. W. Day, L. H. Herbertson, M. Buesen, U. Steinseifer, K. I. Aycock, B. C. Good, S. Deutsch, K. B. Manning, and B. A. Craven. FDA benchmark medical device flow models for CFD validation. ASAIO J. 63:150–160, 2017.
Markl, M., F. P. Chan, M. T. Alley, K. L. Wedding, M. T. Draney, C. J. Elkins, D. W. Parker, R. Wicker, C. A. Taylor, R. J. Herfkens, and N. J. Pelc. Time-resolved three-dimensional phase-contrast MRI. J. Magn. Resonance Imaging. 17:499–506, 2003.
Marsden, A. L., Y. Bazilevs, C. C. Long, and M. Behr. Recent advances in computational methodology for simulation of mechanical circulatory assist devices. Wiley Interdiscip. Rev. Syst. Biol. Med. 6:169–188, 2014.
Morrison, T. M., M. L. Dreher, S. Nagaraja, L. M. Angelone, and W. Kainz. The role of computational modeling and simulation in the total product life cycle of peripheral vascular devices. J. Med. Devices.11:024503, 2017.
Mueller, M., H. Schima, H. Engelhardt, A. Salat, D. Olsen, U. Losert, and E. Wolner. In vitro hematological testing of rotary blood pumps: remarks on standardization and data interpretation. Artif. Organs. 17:103–110, 1993.
Najjari, M. R., J. A. Hinke, K. V. Bulusu, and M. W. Plesniak. On the rheology of refractive-index-matched, non-Newtonian blood-analog fluids for PIV experiments. Exp. Fluids. 2016. https://doi.org/10.1007/s00348-016-2185-x.
Oberkampf, W. L., and C. J. Roy. Verification and Validation in Scientific Computing. Cambridge, UK: Cambridge University Press, 2010.
Pant, S., G. Limbert, N. P. Curzen, and N. W. Bressloff. Multiobjective design optimisation of coronary stents. Biomaterials. 32:7755–7773, 2011.
Pauli, L., J. Nam, M. Pasquali, and M. Behr. Transient stress-based and strain-based hemolysis estimation in a simplified blood pump. Int. J. Numer. Methods Biomed. Eng. 29:1148–1160, 2013.
Roache, P. J. Fundamentals of Verification and Validation. Socorro, New Mexico: Hermosa Publishers, 2009.
Song, X., A. L. Throckmorton, H. G. Wood, J. F. Antaki, and D. B. Olsen. Computational fluid dynamics prediction of blood damage in a centrifugal pump. Artif. Organs. 27:938–941, 2003.
Stewart, S. F., P. Hariharan, E. G. Paterson, G. W. Burgreen, V. Reddy, S. W. Day, M. Giarra, K. B. Manning, S. Deutsch, M. R. Berman, M. R. Myers, and R. A. Malinauskas. Results of FDA’s first interlaboratory computational study of a nozzle with a sudden contraction and conical diffuser. Cardiovasc. Eng. Technol. 4:374–391, 2013.
Stewart, S. F., E. G. Paterson, G. W. Burgreen, P. Hariharan, M. Giarra, V. Reddy, S. W. Day, K. B. Manning, S. Deutsch, M. R. Berman, M. R. Myers, and R. A. Malinauskas. Assessment of CFD performance in simulations of an idealized medical device: results of FDA’s first computational interlaboratory study. Cardiovasc. Eng. Technol. 3:139–160, 2012.
Stewart, S. F. C., R. A. Robinson, R. A. Nelson, and R. A. Malinauskas. Effects of thrombosed vena cava filters on blood flow: flow visualization and numerical modeling. Ann. Biomed. Eng. 36:1764–1781, 2008.
Walenga, R., C. Butler, B. Craven, P. Longest, R. Mohamed, B. Newman, B. Olsson, G. Hochhaus, B. Li, M. Luke, L. Zhao, A. Przekwas, and R. Lionberger. Mechanistic Modeling of Generic Orally Inhaled Drug Products (OIDPs): A Workshop Summary Report. Clinical Pharmacology & Therapeutics: Pharmacometrics & Systems Pharmacology (in press), 2022.
Acknowledgments
We thank Dr. Steven Day of the Rochester Institute of Technology who helped to design and fabricate the blood pump model in collaboration with RAM, and Dr. Sandy Stewart of the FDA for administering the interlaboratory CFD study. We thank Dr. Kenneth Aycock for reviewing the manuscript and for providing helpful comments and suggestions. This project was funded by the FDA CDRH Critical Path program and, in part, by a National Science Foundation INTERN supplement through NSF CMMI-2017805.
Conflict of interest
The authors declare that they have no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
Associate Editor Joel Stitzel oversaw the review of this article.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ponnaluri, S.V., Hariharan, P., Herbertson, L.H. et al. Results of the Interlaboratory Computational Fluid Dynamics Study of the FDA Benchmark Blood Pump. Ann Biomed Eng 51, 253–269 (2023). https://doi.org/10.1007/s10439-022-03105-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10439-022-03105-w