Abstract
Purpose
This study aimed to evaluate the diagnostic performance of ultrasound to locate atresia/stenosis and other abdominal anomalies in pediatric patients with duodenal atresia/stenosis, including intestinal malrotation and annular pancreas.
Methods
We classified 36 retrospective cases of duodenal atresia/stenosis based on intestinal malrotation status, and evaluated the diagnostic performance of ultrasound/upper gastrointestinal contrast studies to locate atresia/stenosis and intestinal malrotation, as well as ultrasound for detecting additional anomalies such as annular pancreas. The incidence of annular pancreas was compared between groups using Fisher’s exact test.
Results
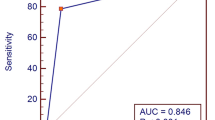
Atresia/stenosis was correctly located by ultrasound in 33 (91.7%) cases and by upper gastrointestinal contrast study in 36 (100%) cases. Of the eight cases with intestinal malrotation, five and two were correctly diagnosed by ultrasound and upper gastrointestinal contrast study, respectively. Ultrasound correctly diagnosed annular pancreas in 6/14 cases. The incidence of annular pancreas was significantly different between the groups (present/absent in groups with vs. without intestinal malrotation: 6/2 vs. 8/20, P = 0.036).
Conclusions
Ultrasound has a relatively high capability in locating atresia/stenosis. However, some cases are misdiagnosed. In clinical practice, upper gastrointestinal contrast studies should be used complementarily during diagnosis. Additional anomalies may not be detected by preoperative examinations; therefore, surgeons should carefully evaluate for additional anomalies during surgery, especially coexisting intestinal malrotation and annular pancreas.






Similar content being viewed by others
References
Chen QJ, Gao ZG, Tou JF, et al. Congenital duodenal obstruction in neonates: a decade’s experience from one center. World J Pediatr. 2014;10:238–44.
Kimura K, Tsugawa C, Ogawa K, et al. Diamond-shaped anastomosis for congenital duodenal obstruction. Arch Surg. 1977;112:1262–3.
Bethell GS, Long AM, Knight M, et al. The impact of trisomy 21 on epidemiology, management, and outcomes of congenital duodenal obstruction: a population-based study. Pediatr Surg Int. 2020;36:477–83.
Gfroerer S, Theilen TM, Fiegel HC, et al. Comparison of outcomes between complete and incomplete congenital duodenal obstruction. World J Gastroenterol. 2019;25:3787–97.
Bethell GS, Long AM, Knight M, et al. Congenital duodenal obstruction in the UK: a population-based study. Arch Dis Child Fetal Neonatal Ed. 2020;105:178–83.
Carroll AG, Kavanagh RG, Ni Leidhin C, et al. Comparative effectiveness of imaging modalities for the diagnosis of intestinal obstruction in neonates and infants: a critically appraised topic. Acad Radiol. 2016;23:559–68.
Miscia ME, Lauriti G, Lelli Chiesa P, et al. Duodenal atresia and associated intestinal atresia: a cohort study and review of the literature. Pediatr Surg Int. 2019;35:151–7.
Hosokawa T, Yamada Y, Tanami Y, et al. Sonography for an imperforate anus: approach, timing of the examination, and evaluation of the type of imperforate anus and associated anomalies. J Ultrasound Med. 2017;36:1747–58.
Hosokawa T, Hosokawa M, Tanami Y, et al. Use of ultrasound findings to predict bowel ischemic changes in pediatric patients with intestinal volvulus. J Ultrasound Med. 2020;39:683–92.
Guerra A, De Gaetano AM, Infante A, et al. Imaging assessment of portal venous system: pictorial essay of normal anatomy, anatomic variants and congenital anomalies. Eur Rev Med Pharmacol Sci. 2017;21:4477–86.
Harnoss JM, Harnoss JC, Diener MK, et al. Portal annular pancreas: a systematic review of a clinical challenge. Pancreas. 2014;43:981–6.
Joseph P, Raju RS, Vyas FL, et al. Portal annular pancreas. A rare variant and a new classification. JOP. 2010;11:453–5.
Kanazawa H, Nosaka S, Miyazaki O, et al. The classification based on intrahepatic portal system for congenital portosystemic shunts. J Pediatr Surg. 2015;50:688–95.
Chen Q, Gao Z, Zhang L, et al. Multifaceted behavior of Meckel’s diverticulum in children. J Pediatr Surg. 2018;53:676–81.
Yousefzadeh DK, Kang K, Tessicini L. Assessment of retromesenteric position of the third portion of the duodenum: an US feasibility study in 33 newborns. Pediatr Radiol. 2010;40:1476–84.
Yousefzadeh DK. The position of the duodenojejunal junction: the wrong horse to bet on in diagnosing or excluding malrotation. Pediatr Radiol. 2009;39(Suppl 2):S172–7.
Menten R, Reding R, Godding V, et al. Sonographic assessment of the retroperitoneal position of the third portion of the duodenum: an indicator of normal intestinal rotation. Pediatr Radiol. 2012;42:941–5.
Piglia E, Penna CRR, Tobias J, et al. The main radiologic findings in annular pancreas. Radiol Bras. 2019;52:275–6.
Sandrasegaran K, Patel A, Fogel EL, et al. Annular pancreas in adults. AJR Am J Roentgenol. 2009;193:455–60.
Sizemore AW, Rabbani KZ, Ladd A, et al. Diagnostic performance of the upper gastrointestinal series in the evaluation of children with clinically suspected malrotation. Pediatr Radiol. 2008;38:518–28.
Mentessidou A, Saxena AK. Laparoscopic repair of duodenal atresia: systematic review and meta-analysis. World J Surg. 2017;41:2178–84.
Taylor GA. CT appearance of the duodenum and mesenteric vessels in children with normal and abnormal bowel rotation. Pediatr Radiol. 2011;41:1378–83.
Choi KS, Choi YH, Cheon JE, et al. Intestinal malrotation in patients with situs anomaly: Implication of the relative positions of the superior mesenteric artery and vein. Eur J Radiol. 2016;85:1695–700.
McVay MR, Kokoska ER, Jackson RJ, et al. Jack Barney Award. The changing spectrum of intestinal malrotation: diagnosis and management. Am J Surg. 2007;194:712–7.
Xiong Z, Shen Y, Morelli JN, et al. CT facilitates improved diagnosis of adult intestinal malrotation: a 7-year retrospective study based on 332 cases. Insights Imaging. 2021;12:58.
Steiner GM. The misplaced caecum and the root of the mesentery. Br J Radiol. 1978;51:406–13.
Nagpal SJS, Peeraphatdit T, Sannapaneni SK, et al. Clinical spectrum of adult patients with annular pancreas: Findings from a large single institution cohort. Pancreatology. 2019;19:290–5.
Sadler TW. Langman’s medical embryology (English edition). 14th ed. Philadelphia: Wolters Kluwer Health; 2018.
Acknowledgements
We would like to thank Editage for English language editing.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Takahiro Hosokawa, Yutaka Tanami, Yumiko Sato, Tetsuya Ishimaru, Hiroshi Kawashima, and Eiji Oguma declare that they have no financial or personal relationships that could lead to a conflict of interest.
Research involving human subjects
This research was performed in accordance with the tenets of the Declaration of Helsinki.
Informed consent
This retrospective study was approved by the ethics committee of our institution, and informed consent was waived.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Hosokawa, T., Tanami, Y., Sato, Y. et al. The diagnostic accuracy of ultrasound and upper gastrointestinal contrast studies for locating atresia/stenosis and intestinal malrotation and detecting annular pancreas in pediatric patients with duodenal atresia/stenosis. J Med Ultrasonics 49, 299–309 (2022). https://doi.org/10.1007/s10396-021-01176-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10396-021-01176-1