Summary
Background
The role of morbidity and mortality conferences (M&MC) in surgical departments is to provide education and improve patient care. However, there is sparse evidence in the literature that M&MCs reduce preventable deaths. Therefore, this study aimed to assess the impact of routine M&MC on reducing the preventable death rate over 4 years at a tertiary hospital in Botswana.
Methods
This study used a quantitative research methodology. In this retrospective audit of the M&MC data, we collected all mortality data for the surgery department from the time the database started, July 2016, to December 2019. The department adopted and adapted the criteria and definitions of preventability based on the World Health Organization (WHO) guidelines for trauma quality improvement programs. We used the Pearson correlation statistic to evaluate the correlation between the time (years) since the start of routine M&MC and the preventable death rate. Ethical approval for the study was obtained.
Results
There were 4660 registered admissions from July 2016 to December 2019. Of these, 267 deaths were recorded, resulting in a crude mortality rate of 6%. Overall, the department considered 23% (61/267) of the deaths as preventable. A strong linear correlation (R2 = 0.982, p = 0.009) was found between the preventable death rate and time (years) since the commencement of routine M&MC. Trauma was the leading cause of preventable deaths (24.6%, 15/61).
Conclusion
Our findings suggest that routine M&MCs have the desired effect of reducing preventable death rates. Further studies are required to investigate this observed effect.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The historical roots of morbidity and mortality conferences (M&MC) appear to have come from attempts to address medical errors in surgery and anesthesia departments [1, 2]. The role of M&MC in surgical departments is to educate and improve patient care [3]. This forum allows for objective and nonjudgmental reviews of medical errors and adverse events [4]. Evidence in the literature that M&MC reduce preventable deaths is sparse; however, there is more evidence of their educational role [5,6,7,8]. In this study, we adopted and adapted the death preventability classification provided by the World Health Organization (WHO) guidelines for trauma quality improvement programs.
The WHO guidelines for trauma quality improvement programs recommend the establishment of death review panel committees in healthcare institutions for the classification of death preventability [6]. The death review panel committee presents, discusses, and reaches a consensus on the death preventability classification based on set criteria. The guidelines recommend that whatever classification system is used by the death review panel should be communicated clearly to the panelists. The committee chair leads the meetings and guides the decision process for determining the death classification as preventable, non-preventable, or potentially preventable. The definitions of death preventability classification by the WHO quality improvement programs are outlined below:
Preventable
-
Injuries and sequelae considered survivable.
-
Death could have been prevented if appropriate steps had been taken.
-
Frank deviations from the standard of care that, directly or indirectly, caused patient’s death.
-
Statistically, the probability of survival greater than 50%, or Injury Severity Score (ISS) below 20.1
Potentially preventable
-
Injuries and sequelae severe but survivable.
-
Death potentially could have been prevented if appropriate steps had been taken.
-
Evaluation and management generally appropriate.
-
Some deviations from the standard of care that may, directly or indirectly, have been implicated in the patient’s death.
-
Statistically, the probability of survival is 25–50% or ISS between 20 and 50.1
Non-preventable
-
Injuries and sequelae non-survivable even with optimal management.
-
Evaluation and management appropriate according to accepted standards.
-
If patient had comorbid factors, these were major contributors to death.
-
Statistically, the probability of survival less than 25% or ISS above 50.1.
As mentioned before, the literature substantiating the role of M&MC in reducing preventable deaths is very sparse [5]. The assumption is that acknowledging adverse events and medical errors will reduce adverse events and preventable deaths in the future [5, 9]. One notable study by Kashiwazaki et al. showed that M&MC significantly reduced preventable morbidity events among residents and experienced neurosurgeons [7]. In the same study, the residents’ educational effect was more distinct. There were no significant differences in mortality incidence. The decrease in the incidence of preventable morbidity was more pronounced in residents than in senior neurosurgeons [7]. This finding suggests that knowledge acquisition reduces avoidable morbidities.
The Western Australian Audit of Surgical Mortality (WAASM), established in 2002, conducted a 10-year review of surgical mortalities. They noted that the mortality rate in the initial years remained unchanged, but a progressive fall subsequently occurred [10]. This trend was observed in similar audits [5], with minimal initial change in mortality rate and a significant decrease as the audit-influenced practice. These audits suggest that sustained and routine M&MCs are needed for a long period before noticing a tangible effect on the mortality rate.
To our knowledge, no study has been conducted locally or regionally to assess the impact of routine surgical M&MC on reducing preventable death rates. Preventable hospital mortality is a critical public health concern. The present study sought to determine the impact of routine M&MC on reducing preventable death rates in the Department of Surgery. This followed the adoption of monthly and regular M&MC in the department in July 2016. A committee with a chair and a database manager was created for the first time. A Microsoft® Access database (Microsoft Corporation, One Microsoft Way, Redmond, WA, USA) was established to capture information on mortality and morbidity. This study represents be an audit of our quality assurance intervention, M&MC, and seeks to assess its impact on the department concerning the reduction of preventable death rates.
Methods
This study utilized a quantitative research methodology to assess the impact of routine M&MC on reducing preventable death rates. In this retrospective audit of the M&MC data, we collected all mortality data for the Department of Surgery from the date the database started, July 2016, to December 2019.
During data capture in our department, each surgical team classified their mortalities as preventable or non-preventable. In addition, at each monthly M&MC, the department reviewed all mortalities for learning points and approved the classification of deaths or amended them as appropriate based on the consensus reached. Mortalities of operatively and non-operatively managed surgical patients were all discussed. This is because the benefit of M&MC is equally important for both groups of patients. Cases were shared with members of the department on the day before the M&MC. The department adopted and adapted the criteria and definitions of preventability based on WHO guidelines for trauma quality improvement programs [6]. Mortality was defined as follows.
-
1.
Preventable if:
-
The pathology was deemed to be survivable.
-
Death could have been prevented if appropriate steps had been taken.
-
There were frank deviations from the standards of care that directly or indirectly caused the patient’s death.
-
-
2.
Non-preventable if:
-
The pathology and sequelae were deemed non-survivable even with optimal management.
-
The patient died in the face of appropriate evaluation and management according to accepted standards.
-
The patient had comorbid factors that were major contributors to death.
-
When the department members disagreed, they discussed their classification choices. If a consensus was reached, the death was classified appropriately, and if there were still disagreements, a classification with the majority of support was used. The department stores quality assurance data in an electronic registry.
We retrieved all documented mortalities from the departmental quality assurance electronic registry. Next, we determined the yearly cumulative preventable mortality rate as a percentage of all mortalities. Finally, we assessed the impact of routine M&MC on preventable yearly cumulative mortality rates. This was achieved by determining the proportion of surgical patients who died yearly from preventable causes for 4 years. Using the Pearson correlation statistic, we evaluated the correlation between the duration (years) of routine M&MC and the preventable yearly cumulative death rate. In this study, the preventable death rate refers to the preventable yearly cumulative death rate.
All mortalities were entered into the database from the date the database and routine M&MC started (July 2016) to 2019. Ethical approval was obtained.
Results
There were 4660 registered admissions between July 2016 and December 2019. The mean patient age was 56 years (standard deviation [SD] = 20.1). Of these, 267 deaths were recorded, resulting in a crude mortality rate of 6%. Of the 267 deaths, 41.9% (112/267) were cases of patients who had been operated on: 60% (161/267) were men, and 40% (106/267) were women. The mean age of the mortalities was comparable to that of all admissions (59 years; SD = 19.9). Overall, the department considered 23% (61/267) of deaths as preventable. Of the preventable death, 57.4% (35/61) were cases of patients who has been operated on. Table 1 presents the diagnoses and causes of preventable death. Table 2 shows the annual total and preventable deaths with corresponding overall and preventable death rates.
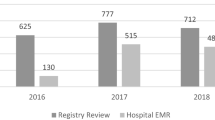
There was an observed progressive decrease in preventable death rates from the time routine M&MC started (July 2016) to December 2019, as shown in Fig. 1. We used Pearson correlation analysis to assess the strength of the correlation between the duration (years) over which routine M&MCs were conducted and the reduction in the preventable mortality rate. Table 3 shows the strong linear correlation (p = 0.009).
The leading diagnoses with preventable deaths were trauma 24.6% (15/61), with polytrauma (4/61), severe head injury (4/61), and burns (5/61).
A subanalysis of the causes of preventable death revealed that septic shock, the leading cause of preventable deaths, was the only one showing a statistically significant reduction over the 4 years. Other causes of death included hemorrhagic shock, multiorgan failure, respiratory failure, and cardiac arrest, as summarized in Table 4.
Discussion
This study aimed to assess the impact of routine M&MC on the preventable death rate over 4 years. Before the study period, M&MC was not routinely conducted in our department, and there was no electronic registry dedicated to surgical quality assurance.
We observed a statistically significant decrease in preventable death rates over 4 years. The preventable mortality rate decreased by approximately 50%, from 36.6% to 18.2% for all mortalities. We note that in the first year of 2016, data were collected only for the second half of the year, from July to December, and may not have been representative. However, the decreasing trend in preventable mortality rates was maintained over the subsequent 3 years. While we acknowledge that some confounders may underlie the findings of the reduction in preventable mortality rate, the results are compelling and suggest that routine M&MC played a significant role. The literature indicates that prospective and continuous data collection on avoidable deaths and identification of errors ultimately directs and informs practice toward improved outcomes [11, 12].
During the M&MC, the department endeavored to create a conducive learning environment and ensured that remedial action was clearly communicated. Residents and medical officers independently documented mortalities and presented them to the department. The input of surgeons was greater during discussions. Discussions of cases addressed principles rather than individuals. As a result, we believe that we foster a conducive learning environment and minimize the tendency to underreport mortality.
In this study, trauma was the leading cause of avoidable deaths. This finding is in keeping with previous studies conducted locally, showing trauma as the most common acute presentation and head injury as a significant public concern among young men in the country [13,14,15]. In total, 68.2% of road traffic collision deaths in our country are considered preventable [16]. Trauma is the leading cause of death both globally and among young people. However, its impact is disproportionately significant in low- and middle-income countries [16, 17], including locally. High rates of trauma-related preventable deaths indicate the need for a comprehensive trauma system [15, 16, 18]. Trauma kills by predictable mechanisms and time frames, and comprehensive trauma systems improve the outcomes of injured patients [19, 20].
Although the diagnoses were variable, the causes of preventable deaths were the same, with septic shock being the most common one. It was also noted that the reduction in the preventable death rates over the 4 years was attributable mainly to the reduction in the rate of septic shock as the cause. The authors believe that interventions implemented in response to the discussion might have had a role in this reduction. Some of the interventions were: implementing a formal handover checklist, especially for very sick patients, weekly presentations on select topics, and daily presentations of new mortalities at morning meetings.
Limitations
The authors acknowledge the limitations of this study. There is potential for under-reporting mortalities. However, the department holds daily morning meetings during which mortalities are reported by the on-call team, making it easy for the department to notice if a case is omitted at the monthly M&MC. There has been an increase in the number of subspecialty services in the private sector compared to the public sector. This has led to increasing subspecialty cases being transferred to the private sector under government cover. This may result in diverting mortalities to the private sector or reducing preventable deaths due to the specialized care provided in the private sector. The findings of this study provide a starting point for further investigation of the impact of M&MC on preventable death rates.
Conclusion
Our findings suggest that routine morbidity and mortality conferences have the desired effect of reducing preventable death rates. Further studies are required to investigate this observed effect.
References
Orlander JD, Barber TW, Fincke BG. The morbidity and mortality conference: the delicate nature of learning from error. Acad Med. 2002 Oct 1;77(10):1001–6.
Orlander JD, Fincke BG. Morbidity and mortality conference: a survey of academic internal medicine departments. J Gen Int Med. 2003 Aug;18:656–8. https://doi.org/10.1046/j.1525-1497.2003.20824.x.
Gore DC. National survey of surgical morbidity and mortality conferences. Am J Surg. 2006 May 1;191(5):708–14. https://doi.org/10.1016/j.amjsurg.2006.01.029.
Deis JN, Smith KM, Warren MD, et al. Transforming the morbidity and mortality conference into an instrument for systemwide improvement. 2008.
George J. Medical morbidity and mortality conferences: past, present and future. Postgrad Med J. 2017 Mar;93(1097):148–52.
World Health Organization. Guidelines for trauma quality improvement programmes. World Health Organization; 2009.
Kashiwazaki D, Saito H, Uchino H, Akioka N, Hori E, Shibata T, Tomita T, Akai T, Kuwayama N, Kuroda S. Morbidity and mortality conference can reduce avoidable morbidity in neurosurgery: its educational effect on residents and surgical safety outcomes. World Neurosurg. 2020 Jan 1;133:e348–55. https://doi.org/10.1016/j.wneu.2019.09.018.
Joseph CW, Garrubba ML, Melder AM. Informing best practice for conducting morbidity and mortality reviews: a literature review. Austral Health Rev. 2017 Apr 20;42(3):248–57. https://doi.org/10.1071/AH16193.
Epstein NE. Morbidity and mortality conferences: their educational role and why we should be there. Surg Neurol Int. 2012;3(Suppl 5):S377. https://doi.org/10.4103/2152-7806.103872.
Kiermeier A, Babidge WJ, McCulloch GA, Maddern GJ, Watters DA, Aitken RJ. National surgical mortality audit may be associated with reduced mortality after emergency admission. ANZ J Surg. 2017 Oct;87(10):830–6. https://doi.org/10.1111/ans.14170.
Healey MA, Shackford SR, Osler TM, Rogers FB, Burns E. Complications in surgical patients. Arch Surg. 2002 May 1;137(5):611–618. https://doi.org/10.1001/archsurg.137.5.611.
Rebasa P, Mora L, Luna A, Montmany S, Vallverdú H, Navarro S. Continuous monitoring of adverse events: influence on the quality of care and the incidence of errors in general surgery. World J Surg. 2009 Feb;33:191–8. https://doi.org/10.1007/s00268-008-9848-6.
Chandra A, Mullan P, Ho-Foster A, Langeveldt A, Caruso N, Motsumi J, Kestler A. Epidemiology of patients presenting to the emergency centre of Princess Marina Hospital in Gaborone, Botswana. Afr J Emerg Med. 2014 Sep 1;4(3):109–14. https://doi.org/10.1016/j.afjem.2013.12.004.
Cox M, Becker T, Motsumi M. Head trauma: A significant public health concern among young men in Botswana. Etiology referral patterns and opportunities for interventions. J Publ Health Afr. 2018 Oct 10;9(2). https://doi.org/10.4081/jphia.2018.798.
Cox M, Becker TD, Motsumi M. Head injury burden in a major referral hospital emergency centre in Botswana. Afr J Emerg Med. 2018 Sep 1;8(3):100–5. https://doi.org/10.1016/j.afjem.2018.02.003.
Motsumi MJ, Ayane G, Kwati M, Panzirah-Mabaka K, Walsh M. Preventable deaths following road traffic collisions in Botswana: a retrospective review. Injury. 2021 Sep 1;52(9):2665–71. https://doi.org/10.1016/j.injury.2021.04.020.
Organisation WH. Injuries and violence: the facts: World Health Organization. 2010.
Motsumi MJ, Mashalla Y, Sebego M, Ho-Foster A, Motshome P, Mokokwe L, Mmalane M, Montshiwa T. Developing a trauma registry in a middle-income country-Botswana. Afr J Emerg Med. 2020; 10(Suppl 1):S29–S37. https://doi.org/10.1016/j.afjem.2020.06.011.
Baert A. Imaging and intervention in abdominal trauma. Berlin: Springer; 2003.
Choi J, Carlos G, Nassar AK, Knowlton LM, Spain DA. The impact of trauma systems on patient outcomes. Curr Prob Surg. 2021 Jan;58(1):100849. https://doi.org/10.1016/j.cpsurg.2020.100849.
Funding
Open access funding provided by University of Botswana.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
M.J. Motsumi, N. Chinyepi, S. Rackara, R. Lwango, G. Kapinga, K. Ngwako, M. Sentsho, T. Leshomo, U. Chilisa, P. Motlaleselelo and E.K. Lekgowe declare that they have no competing interests.
Ethical standards
This study has been approved by the appropriate ethics committee and has therefore been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Motsumi, M.J., Chinyepi, N., Rackara, S. et al. Do regular morbidity and mortality conferences reduce preventable death rates? Our experience at Princess Marina Hospital. Eur Surg 56, 15–20 (2024). https://doi.org/10.1007/s10353-023-00810-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10353-023-00810-1