Abstract
Background
This study aimed to investigate barriers to sperm cryopreservation for patients with advanced germ cell tumors.
Methods
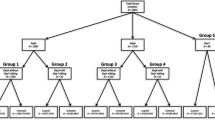
We reviewed data collected from patients who underwent chemotherapy for advanced germ cell tumors in our institutions from 1996 to 2016. We divided sperm cryopreservation procedures into three steps: offering information about sperm cryopreservation, patients’ decision making and sperm collection, and investigating the barriers in each step.
Results
Of the 91 patients, 43 (47%) successfully completed sperm cryopreservation. Thirty (33%) patients were not offered information about sperm cryopreservation from the doctors. Nine patients (9.9%) were offered but declined preservation. Nine patients (9.9%) were not able to provide sperm because of azoospermia (5) and anejaculation (4). Among 43 patients who successfully provided sperm, 10 (23%) had their cryopreserved sperm used for 21 cycles of in vitro fertilization. Ten pregnancies and 7 fatherhoods were achieved. Thirteen patients (30%) had their cryopreserved sperm discarded without use, whereas 20 (47%) continued preserving their sperm for a median 12.5 years.
Conclusions
Not only offering proper information about sperm cryopreservation, but also shared decision making prior to chemotherapy, and considering fertility preservation before orchiectomy are imperative. The rate of use of preserved sperm was relatively high, but decision making for sperm disposal should also be supported.



Similar content being viewed by others
References
Moody JA, Ahmed K, Yap T et al (2019) Fertility managment in testicular cancer: the need to establish a standardized and evidence-based patient-centric pathway. BJU Int 123:160–172
Lampe H, Horwich A, Norman A et al (1997) Fertility after chemotherapy for testicular germ cell cancers. J Clin Oncol 15:239–245
Lee SJ, Schover LR, Partridge AH et al (2006) American Society of Clinical Oncology recommendations on fertility preservation in cancer patients. J Clin Oncol 24:2917–2931
Japan Society of Clinical Oncology (2017) JSCO Clinical practice guidelines 2017 for fertility preservation in childhood, adolescent, and young adults cancer patients. Kanehara, Tokyo
Kawai K, Nishiyama H (2019) Preservation of fertility of adult male cancer patients treated with chemotherapy. Int J Clin Oncol 24:34–40
Ping P, Gu BH, Li P et al (2014) Fertility outcome of patients with testicular tumor: before and after treatment. Asian J Androl 16:107–111
Fraietta R, Spaine DM, Bertolla RP et al (2010) Individual and seminal characteristics of patients with testicular germ cell tumors. Fertil Steril 94:2107–2112
Schover LR, Brey K, Lichtin A et al (2002) Knowledge and experience regarding cancer, infertility, and sperm banking in younger male survivors. J Clin Oncol 20:1880–1889
Sonnenburg DW, Brames MJ, Case-Eads S et al (2015) Utilization of sperm banking and barriers to its use in testicular cancer patients. Support Care Cancer 23:2763–2768
World Health Organization (2010) WHO laboratory manual for the examination and processing of human semen, 5th edn. World Health Organization. https://apps.who.int/iris/handle/10665/44261
Kanda Y (2013) Investigation of the freely available easy-to-use software 'EZR' for medical statistics. Bone Marrow Transpl 48:452–458
Fine JP, Gray RJ (1999) A proportional hazards model for the subdistribution of a competing risk. J Am Stat Assoc 94:496–509
Negoro H, Matsui Y, Nakayama T et al (2018) Sperm cryopreservation: clinical and fertility outcomes in male oncological patients with germ cell tumors or hematological disorders. Reprod Med Biol 17:500–503
Schover LR, Brey K, Lichtin A et al (2002) Oncologists' attitudes and practices regarding banking sperm before cancer treatment. J Clin Oncol 20:1890–1897
Rabah DM, Wahdan IH, Merdawy A et al (2010) Oncologists' knowledge and practice towards sperm cryopreservation in Arabic communities. J Cancer Surviv 4:279–283
Magelssen H, Haugen TB, von During V et al (2005) Twenty years experience with semen cryopreservation in testicular cancer patients: who needs it? Eur Urol 48:779–785
Brydoy M, Fossa SD, Klepp O et al (2005) Paternity following treatment for testicular cancer. J Natl Cancer Inst 97:1580–1588
Stensheim H, Klungsoyr K, Skjaerven R et al (2013) Birth outcomes among offspring of adult cancer survivors: a population-based study. Int J Cancer 133:2696–2705
Signorello LB, Mulvihill JJ, Green DM et al (2012) Congenital anomalies in the children of cancer survivors: a report from the childhood cancer survivor study. J Clin Oncol 30:239–245
Paoli D, Pallotti F, Lenzi A et al (2018) Fatherhood and sperm DNA damage in testicular cancer patients. Front Endocrinol (Lausanne) 9:506
Stahl O, Boyd HA, Giwercman A et al (2011) Risk of birth abnormalities in the offspring of men with a history of cancer: a cohort study using Danish and Swedish national registries. J Natl Cancer Inst 103:398–406
Rives N, Perdrix A, Hennebicq S et al (2012) The semen quality of 1158 men with testicular cancer at the time of cryopreservation: results of the French National CECOS network. J Androl 33:1394–1401
Fossa SD, Aabyholm T, Vespestad S et al (1993) Semen quality after treatment for testicular cancer. Eur Urol 23:172–176
Hamano I, Hatakeyama S, Nakamura R et al (2018) Onco-testicular sperm extraction (Onco-TESE) from a single testis with metachronous bilateral testicular cancer: a case report. Basic Clin Androl 28:1
Ferrari S, Paffoni A, Filippi F et al (2016) Sperm cryopreservation and reproductive outcome in male cancer patients: a systematic review. Reprod Biomed Online 33:29–38
Ragni G, Somigliana E, Restelli L et al (2003) Sperm banking and rate of assisted reproduction treatment: insights from a 15-year cryopreservation program for male cancer patients. Cancer 97:1624–1629
Hamano I, Hatakeyama S, Ohyama C (2017) Fertility preservation of patients with testicular cancer. Reprod Med Biol 16:240–251
Namekawa T, Imamoto T, Kato M et al (2016) Testicular function among testicular cancer survivors treated with cisplatin-based chemotherapy. Reprod Med Biol 15:175–181
Eiser C, Arden-Close E, Morris K et al (2011) The legacy of sperm banking: how fertility monitoring and disposal of sperm are linked with views of cancer treatment. Hum Reprod 26:2791–2798
Pacey AA, Merrick H, Arden-Close E et al (2012) Monitoring fertility (semen analysis) by cancer survivors who banked sperm prior to cancer treatment. Hum Reprod 27:3132–3139
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
No author has any conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Ito, K., Ichioka, K., Dahal, S. et al. Barriers for sperm cryopreservation in advanced germ cell tumor patients: a 20-year experience. Int J Clin Oncol 25, 906–911 (2020). https://doi.org/10.1007/s10147-019-01607-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10147-019-01607-7