Abstract
Increased demand for in vitro fertilization (IVF) due to socio-demographic trends, and supply facilitated by new technologies, converged to transform the way a substantial proportion of humans reproduce. The purpose of this article is to describe the societal and demographic trends driving increased worldwide demand for IVF, as well as to provide an overview of emerging technologies that promise to greatly expand IVF utilization and lower its cost.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Since its clinical introduction in 1978, in vitro fertilization (IVF) has redefined the ability of the human species to procreate. Initially developed to aid the infertile couple, clinical indications for IVF have since rapidly expanded to include medical and genetic conditions, as well as fertility preservation. While IVF access and utilization vary widely globally, the practice now accounts for the conception of over 5% of all newborns in some European countries where IVF is more affordable and/or is covered by insurance [1]. The corresponding figure presently stands at 4.1% in Australia and New Zealand, 1.9% in the USA, and 1.7% in China and is rapidly rising in all regions of the world [2, 3]. Infertility, which affects approximately 10% of couples, remains the main driver of IVF utilization. These simple statistics suggest that IVF utilization may significantly grow in the coming decades if barriers to its utilization are lowered; this is without even considering an increasing number of indications for IVF beyond infertility.
Changing demographics and societal norms are driving increased IVF utilization. Improved access of women to educational and career opportunities, as well as effective contraception has contributed to progressively delayed childbearing and overall lower fertility rates worldwide. In many countries and in virtually all US states, fertility rates are now substantially below population replacement levels of 2100 births per 1000 women. In a growing number of metropolitan areas as well as in entire highly developed countries, the average age at first birth now exceeds 30 years, that is, well beyond peak fertility which occurs in the mid 20s. Inadvertently, a growing proportion of women is delaying childbearing to a point where age-related fertility decline contributes to the prevalence of infertility and to increased demand for fertility treatments including IVF and oocyte cryopreservation. These trends will likely accelerate due to the socio-economic impact of the COVID-19 pandemic, which has forestalled new family formation. Indeed, preliminary data from Chinese cities indicate that birth rates declined between 9 and 32.6% in the second half of 2020 compared with 2019, reflecting effects of the COVID-19 lockdowns [4]. Declining fertility rates in China have prompted its government to reverse a decades old one-child policy in favor of a two-child policy in 2016, and to a three-child policy in 2021.
The utilization of IVF is closely linked to its affordability and accessibility [5]. Indeed, a growing number of countries and US states are adopting various policies intended to reverse declining fertility rates. These policies range from legally mandated insurance coverage for fertility treatments to subsidies intended to ease the burdens of child-rearing. The concept that fertility is a basic human right is just starting to gain traction and is sure to accelerate wider adoption of such policies [6]. Another recent development is the growing number of prominent corporations opting to fund fertility benefits as a part of their social mission and as a means of attracting and retaining employees. Combined, the various policies that promote improved insurance coverage are bound to lower the cost of IVF to patients and increase its utilization.
The distribution of established fertility clinics thus closely corresponds to affluent metropolitan areas with the lowest fertility rates and the most advanced maternal ages at birth. Conversely, less densely populated and less affluent areas are characterized by relatively poor IVF access. Moreover, racial and ethnic disparities in the utilization of IVF, largely due to socio-economic factors, are inversely correlated with fertility rates [7]. An additional driver of IVF utilization is the growing societal acceptance of non-traditional families including single and same-sex parents. Finally, third-party IVF that includes the use of donor oocytes, sperm, or embryo and gestational carrier is rapidly growing, now accounting for over 20% of all birth conceived through IVF in the USA [8].
The IVF process is complex and stressful, it consists of multiple steps which can take up to several months to complete. The main reasons patient prematurely drop-out of IVF prior to achieving a pregnancy are the financial, physical, and psychological burdens of the treatment regimen [9]. Here, we describe promising future approaches and technological innovations which might improve IVF accessibility while reducing its costs and burden of care.
Medical Advancements
Controlled ovarian hyperstimulation (COH) is performed to increase the number of oocytes available for IVF. COH involves multiple injections of gonadotropins and serial visits to the fertility clinic for the conduct of transvaginal ultrasound evaluations and the measurement of circulating hormone levels. It follows that COH is complex, time sensitive, and intensive. Various strategies intent on reducing the number of injections by utilizing long-acting gonadotropins or oral medications are already available and are gaining increased acceptance in the field for the treatment of select patient populations [10, 11]. Similarly, an emerging strategy to measure salivary estradiol levels may help decrease the need for blood draws during COH [12]. Recent advancements in portable lower cost ultrasound devices may further simplify follicular and endometrial monitoring by way of convenient mobile facilities and potentially even self-operated endovaginal telemonitoring [13]. Combined, these approaches may greatly simplify COH by rendering it less invasive and by decreasing the time commitment required. Finally, interventions which may further decrease the treatment burden may include screening of patients for psychological issues as well as offering counseling and coping interventions such as e-therapy as an integral part of IVF [14, 15].
Technological Advancements
Perhaps the most promising technological development that might democratize IVF access in the near-term is the automation and miniaturization of the IVF laboratory. Building, staffing, and manually operating an IVF laboratory account for much of the high cost, maldistribution in access, and variability of outcomes. The basic steps in the IVF laboratory include:
-
1.
identification and separation of sperm and oocytes
-
2.
fertilization
-
3.
embryo culture
-
4.
embryo selection for transfer
-
5.
cryopreservation of surplus embryos and gametes
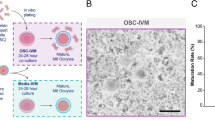
Great progress has already been made towards the automation of these individual steps by way of new technologies. Still, the IVF process in its entirety remains highly manual. The altogether novel IVF lab-on-a-chip concept has the potential to revolutionize IVF by enabling the automation of virtually all of the steps involved in a single system [16,17,18].
Microfluidics is defined as a multidisciplinary field of study and design whereby fluid behaviors are accurately controlled and manipulated with small scale geometric constraints that yields dominance of surface forces over volumetric counterparts. Past procedures in the IVF laboratory, though successful, apply a macroscale approaches to microscale cellular biological events [18]. Integration of microfluidics into the IVF laboratory may give rise to at least four foreseeable advantages: (1) precisely controlled fluidic gamete/embryo manipulations; (2) providing biomimetic environments for culture; (3) facilitating microscale genetic and molecular bioassays; and (4) enabling miniaturization and automation. The basic utility and advantages of individual microfluidic devices for gamete and preimplantation embryo isolation, manipulation, and assessment have been demonstrated [18]. Current efforts are focused on integrating extant individualized microfluidic procedural components into a future IVF lab-on-a-chip.
Microfluidic sperm-sorting devices [19,20,21] and automated sperm analyzers [22] are already being introduced into routine IVF practice. Indeed, microfluidics has been used for the isolation of sperm from semen and testicular biopsies [23,24,25,26,27,28,29]. These novel sperm-isolating microfluidics devices provide for the collection of highly motile sperm populations replete with enriched normal morphology, and most importantly, reduced DNA fragmentation relative to conventional methods of sperm isolation [19, 27, 30, 31].
Microfluidic in vitro insemination has been demonstrated [32], whereas conventional fertilization is suitable for the vast majority of IVF patients, microfluidic systems may further decrease the need for Intracytoplasmic Sperm Injection (ICSI). Such outcomes may even be possible in the setting of oligospermia, because even a low concentration of sperm may still be sufficient to achieve fertilization [32]. As ICSI has become a dominant method of insemination in human clinical IVF, the importance of precise microfluidic push/pull cumulus-oocyte-complex cumulus cell removal has been shown to yield good visualization of the oocyte cytoplasm/orientation [33]. The fertilization step by ICSI is perhaps the most technically difficult step to achieve on a commercial scale, but feasibility of one such system has been demonstrated [34]. Future automated ICSI will likely involve a combination of microfluidics, robotics, and refined optics [34, 35].
Embryo culture has already been fully automated with use of time-lapse incubators which allow continuous monitoring of embryo development. Data generated from time-lapse incubators can be analyzed with machine learning to aid in the selection of embryos with the highest pregnancy potential [36,37,38]. Additional information about embryo viability may be gleaned from other omics technologies which can either sample the embryo directly or indirectly via its culture media. The technologies in question include genomic, transcriptomic, proteomic, and metabolomic analyses [39]. Although the use of preimplantation genetic testing (PGT) of trophectoderm cells of blastocyst stage embryos is quite common in clinical practice, the utility of such testing for the ascertainment of aneuploidy remains controversial on both biological and technical grounds [40]. Microfluidics technology has been successfully used to culture mammalian preimplantation embryos from the zygote to the blastocyst stage both individually and in groups [41,42,43,44,45,46]. These experiments have proven informative to overcoming the hurdles of microenvironment manipulations in microfluidic devices involving microchannels [42], microfunnels [45], microwells [44], and microdroplets [46] that can induce shear stresses and osmotic shifts that can be detrimental to embryo development [45, 47]. The importance of individual embryo culture in microfluidic devices can be appreciated when one considers the desire to integrate real-time imaging and morphometrics [48], molecular [49], and/or metabolomic [50, 51] bioassays, biomechanics [52], and non-invasive PGT of cell-free DNA in spent media [53]. Noninvasive PGT, which utilizes cell-free DNA released into the spent embryo culture media, is likely to become the first omics technology used clinically in conjunction with a microfluidic system [53].
Finally, cryopreservation of sperm, oocytes, and embryos has become the standard of care. Vitrification has become the dominant method for oocyte and embryo cryopreservation. While semi-automated/automated systems for oocyte/embryo vitrification have been reported and are now in early stages of clinical adoption [54,55,56], these devices do not necessarily use or require microfluidics. If one looks to the future of a microfluidic automated lab-on-a-chip, the question arises of whether or not microfluidics is useful and/or beneficial in the vitrification process? Microfluidics can be used to precisely control cryoprotectant exposures (gradual versus step-wise exposure) to oocytes/zygotes/embryos and thus reduce osmotic strain, reduce sub-lethal membrane damage, and improve subsequent development [57,58,59,60]. Future potential benefits of integrating microfluidics with vitrification and automation have been carefully enumerated in recent reviews [59, 61, 62]. Integrated microfluidics for vitrification with automation is promising. Such a system/device will reduce reagent consumption, decrease labor intensity, facilitate ease of use, offer medium to high throughput, and may foster point-of-care cryopreservation and/or promote in-office cryopreservation procedures that require less in the way of technical/personnel expertise and sophisticated laboratory/equipment needs.
Figure 1 illustrates the future IVF lab-on-a-chip concept, including all of the laboratory steps performed during IVF while integrating emerging non-invasive techniques of embryo assessment. Adoption of automated IVF systems offers multiple potential advantages: standardization of workflows, reduction in errors, reduction in cost, reduction in contamination, and the potential for incremental system improvement via machine learning. Additionally, miniaturization and automation of the IVF laboratory can greatly improve accessibility to IVF treatment for underserved communities, especially those who are economically disadvantaged and who reside in rural areas. Regulatory approval will doubtlessly be required if automated systems are to be adequately validated to produce clinical outcomes superior to those attained with the current manual process in the IVF laboratory. Furthermore, automation will likely significantly decrease the staffing requirements and alter the type of skills required to operate fertility centers. It is likely that the technical aspects of IVF will be gradually assumed by machines. This may well increase the emphasis placed on human interactions which supports the medical and psychological needs of patients during their fertility journey.
Scientific Advancements
Fertility preservation research has steadily increased our understanding of the mechanisms that govern folliculogenesis [63]. The development of in vitro culture systems for follicles provided insights into the relationship between oocytes and their surrounding somatic cells, as well as the requisite hormones and growth factors. Multi-step culture systems have advanced to a point where primordial follicles residing in ovarian cortical tissue can undergo activation, growth, and in vitro maturation (IVM) to yield metaphase II (MII) oocytes [64]. These advancements are expanding fertility preservation via ovarian tissue cryopreservation and subsequent chance at parenthood via IVF to pre-pubertal girls and young women at-risk to develop primary ovarian insufficiency (POI) due to gonadotoxic chemotherapy for cancer or due to other serious diseases. Intriguing extensions of this technology may enable the isolation of oocytes from patients who have already developed POI or have entered natural menopause so long as some dormant follicles remain within their ovarian cortex. Another avenue of research is to develop an artificial ovary as has been achieved in a murine model using 3D printed scaffolds for tissue engineering [65, 66]. Microfluidic culture systems may also be utilized to support follicle development while mimicking the natural menstrual cycle [67].
In Vitro Gametogenesis (IVG)
Perhaps the most revolutionary concept in modern reproductive science is that of in vitro gametogenesis (IVG). IVG comprises various approaches, including organ culture systems, embryonic stem cells (ESC), induced pluripotent stem cells (iPSC), and spermatogonial stem cells (SSCs). Several of these approaches led to the creation of functional gametes in rodent models [68]. Japanese scientists, who have been at the forefront of IVG research, have recently succeeded in extending these techniques to the generation of human oogonia from iPSCs [69]. Yet, another approach to IVG involves reconstruction of functional oocytes by nuclear transfer of the first polar body genome from an MII oocyte into an enucleated donor MII cytoplasm [70]. This latter technique may well increase the number of oocytes available for the treatment of infertility of women with few or poor-quality autologous oocytes.
The existence of human oogonial stem cells (OSCs) capable of giving rise to new oocytes has been an area of some controversy for nearly a decade. Reports to the effect that cells isolated from human ovarian tissue using fluorescence-activated cell sorting and an antibody against the DDX4 protein constituted OSCs challenged the long-standing dogma that the ovarian reserve is finite [71, 72]. Multiple follow up studies by several groups were unable to confirm the presence of OSCs in the human ovary. Recently, single-cell analysis of the human ovarian cortex failed to identify OSCs [73]. Instead, cells captured by the DDX4-directed antibody proved to be perivascular cellular elements [73].
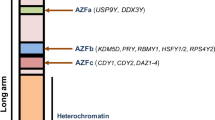
SSCs constitute the progenitor cells in the process of spermatogenesis. As such, these cells are the focus of in vitro spermatogenesis (IVS) and in vivo restoration of male fertility. While IVS has been achieved in rodent models, it has proven far more difficult to realize in primate counterparts [74]. One recent approach to IVS involved the culture of SSCs with immortalized Sertoli cells. Meiosis and the production of spermatid-like cells followed, albeit in the face of improper activation of cognate meiotic checkpoints [75]. In yet another approach, sperm nuclear transfer allowed production of androgenetic haploid embryonic stem cells which were able to “fertilize” oocytes and support early embryonic development, diploid blastocysts, and ESC generation [76]. Once fully realized, IVS is destined to offer genetic parenthood via IVF to infertile men diagnosed with azoospermia and pre-pubertal boys undergoing gonadotoxic treatments.
Reproductive Genetics
The convergence of IVF with reproductive genetics has been at the forefront of the field for the past few decades. The development of next generation sequencing has expedited the adoption of PGT of embryos with an eye toward detecting the presence of chromosomal abnormalities. Moreover, increased use of carrier screening of infertile couples has increased the use of PGT for monogenic diseases. As cost of carrier screening decreases and the number of detected mutations expands, a substantial new population of patients identified as carriers may pursue IVF with PGT to build their families. Indeed, population genomic screening of young adults may offer significant healthcare savings through the prevention of rare disorders and cancers [77]. Future applications of PGT may expand to multifactorial diseases and whole-exome screening, though current attempts at introduction of embryo selection based on polygenic scores into clinical practice seem premature and fraught with ethical challenges [78]. Recent improvements in micromanipulation techniques and the development of CRISPR-Cas9 gene editing tools [79] raise the prospect of germline genome modification (GGM) for severe monogenic disorders. Indeed, GGM has already been achieved in human embryos [80]. Mitochondrial replacement therapy (MRT) for the prevention of heritable mitochondrial DNA diseases is even further developed than GGM, with clinical trials already underway in the UK [81].
Conclusion
The growing utilization of IVF will transform the way a substantial proportion of the human species procreates. It is likely that in the near future, as many as 10% of all children will be conceived through IVF in many parts of the world. Given the rapid scientific and technological evolution of IVG and of reproductive genetics, it is imperative that both the public and regulatory bodies be engaged in establishing a framework for the ethical evaluation of emerging technologies [82,83,84]. Such public engagement is critical. The absence of such may well result in reactionary bans against clinical research as has been the case for GGM and MRT in the USA [85]. Moreover, the introduction of innovative technologies into clinical practice must be rooted in science and supported by well-designed clinical trials [86]. Premature commercialization of costly and unproven “add-ons” to IVF has been an ongoing issue in the field, ranging from procedures to medicines to laboratory techniques [87, 88]. Collectively, routine application and marketing of unproven IVF add-ons may erode the public trust in the reproductive medicine field. Thus, it is imperative for the field to prioritize requiring confirmation of safety and efficacy of technologies before allowing them to be offered routinely to IVF patients. Reproductive medicine, and especially IVF, is rapidly transforming human reproduction and is thus bound to remain of fundamental importance to both science and society.
Data availability
Not applicable.
Code Availability
Not applicable.
Abbreviations
- COH:
-
Controlled ovarian hyperstimulation
- ESC:
-
Embryonic stem cells
- GSC:
-
Germline stem cells
- GGM:
-
Germline genome modification
- iPSC:
-
Induced pluripotent stem cells
- ICSI:
-
Intracytoplasmic sperm injection
- IVF:
-
In vitro fertilization
- IVG:
-
In vitro gametogenesis
- IVM:
-
In vitro maturation
- IVS:
-
In vitro spermatogenesis
- MII:
-
Metaphase II
- MRT:
-
Mitochondrial replacement therapy
- OSC:
-
Oogonial stem cells
- PGT:
-
Preimplantation genetic testing
- POI:
-
Primary ovarian insufficiency
- SSC:
-
Spermatogonial stem cells
References
European IVF-monitoring consortium (EIM)‡ for the European society of human reproduction and embryology (ESHRE), Wyns C, Bergh C, et al. ART in Europe, 2016: results generated from European registries by ESHRE. Hum Reprod Open. 2020;2020(3):hoaa032. https://doi.org/10.1093/hropen/hoaa032
De Geyter C, Wyns C, Calhaz-Jorge C, et al. 20 years of the European IVF-monitoring consortium registry: what have we learned? A comparison with registries from two other regions. Hum Reprod. 2020;35(12):2832–49. https://doi.org/10.1093/humrep/deaa250.
Bai F, Wang DY, Fan YJ, et al. Assisted reproductive technology service availability, efficacy and safety in mainland China: 2016. Hum Reprod. 2020;35(2):446–52. https://doi.org/10.1093/humrep/dez245.
Instead of a desperately needed baby boom, China gets a COVID-19 baby bust - SupChina. https://supchina.com/2021/02/09/instead-of-a-desperately-needed-baby-boom-china-gets-a-covid-19-baby-bust/. Accessed Apr 2, 2021.
Chambers GM, Adamson GD, Eijkemans MJC. Acceptable cost for the patient and society. Fertil Steril. 2013;100(2):319–27. https://doi.org/10.1016/j.fertnstert.2013.06.017.
Kawwass JF, Penzias AS, Adashi EY. Fertility-a human right worthy of mandated insurance coverage: the evolution, limitations, and future of access to care. Fertil Steril. 2021;115(1):29–42. https://doi.org/10.1016/j.fertnstert.2020.09.155.
Shapiro AJ, Darmon SK, Barad DH, Albertini DF, Gleicher N, Kushnir VA. Effect of race and ethnicity on utilization and outcomes of assisted reproductive technology in the USA. Reprod Biol Endocrinol. 2017;15(1):44. https://doi.org/10.1186/s12958-017-0262-5.
Kushnir VA, Darmon SK, Shapiro AJ, Albertini DF, Barad DH, Gleicher N. Utilization of third-party in vitro fertilization in the United States. Am J Obstet Gynecol. 2017;216(3):266.e1-266.e10. https://doi.org/10.1016/j.ajog.2016.11.1022.
Verberg MFG, Eijkemans MJC, Heijnen EMEW, et al. Why do couples drop-out from IVF treatment? A prospective cohort study Hum Reprod. 2008;23(9):2050–5. https://doi.org/10.1093/humrep/den219.
Pouwer AW, Farquhar C, Kremer JAM. Long-acting FSH versus daily FSH for women undergoing assisted reproduction. Cochrane Database Syst Rev. 2015;(7):CD009577. https://doi.org/10.1002/14651858.CD009577.pub3
Datta AK, Maheshwari A, Felix N, Campbell S, Nargund G. Mild versus conventional ovarian stimulation for IVF in poor responders: a systematic review and meta-analysis. Reprod Biomed Online. 2020;41(2):225–38. https://doi.org/10.1016/j.rbmo.2020.03.005.
Sakkas D, Howles CM, Atkinson L, et al. A multi-centre international study of salivary hormone oestradiol and progesterone measurements in ART monitoring. Reprod Biomed Online. 2020. https://doi.org/10.1016/j.rbmo.2020.10.012.
Gerris J, Delvigne A, Dhont N, et al. Self-operated endovaginal telemonitoring versus traditional monitoring of ovarian stimulation in assisted reproduction: an RCT. Hum Reprod. 2014;29(9):1941–8. https://doi.org/10.1093/humrep/deu168.
Rich CW, Domar AD. Addressing the emotional barriers to access to reproductive care. Fertil Steril. 2016;105(5):1124–7. https://doi.org/10.1016/j.fertnstert.2016.02.017.
van Dongen AJCM, Nelen WLDM, IntHout J, Kremer JAM, Verhaak CM. e-therapy to reduce emotional distress in women undergoing assisted reproductive technology (ART): a feasibility randomized controlled trial. Hum Reprod. 2016;31(5):1046–57. https://doi.org/10.1093/humrep/dew040.
Weng L. IVF-on-a-chip: recent advances in microfluidics technology for in vitro fertilization. SLAS Technol. 2019;24(4):373–85. https://doi.org/10.1177/2472630319851765.
Swain JE, Lai D, Takayama S, Smith GD. Thinking big by thinking small: application of microfluidic technology to improve ART. Lab Chip. 2013;13(7):1213–24. https://doi.org/10.1039/c3lc41290c.
Smith GD, Takayama S. Application of microfluidic technologies to human assisted reproduction. Mol Hum Reprod. 2017;23(4):257–68. https://doi.org/10.1093/molehr/gaw076.
Quinn MM, Jalalian L, Ribeiro S, et al. Microfluidic sorting selects sperm for clinical use with reduced DNA damage compared to density gradient centrifugation with swim-up in split semen samples. Hum Reprod. 2018;33(8):1388–93. https://doi.org/10.1093/humrep/dey239.
Parrella A, Keating D, Cheung S, et al. A treatment approach for couples with disrupted sperm DNA integrity and recurrent ART failure. J Assist Reprod Genet. 2019;36(10):2057–66. https://doi.org/10.1007/s10815-019-01543-5.
Marzano G, Chiriacò MS, Primiceri E, et al. Sperm selection in assisted reproduction: a review of established methods and cutting-edge possibilities. Biotechnol Adv. 2020;40:107498. https://doi.org/10.1016/j.biotechadv.2019.107498.
Lammers J, Chtourou S, Reignier A, Loubersac S, Barrière P, Fréour T. Comparison of two automated sperm analyzers using 2 different detection methods versus manual semen assessment. J Gynecol Obstet Hum Reprod. 2021;50(8):102084. https://doi.org/10.1016/j.jogoh.2021.102084.
Cho BS, Schuster TG, Zhu X, Chang D, Smith GD, Takayama S. Passively driven integrated microfluidic system for separation of motile sperm. Anal Chem. 2003;75(7):1671–5. https://doi.org/10.1021/ac020579e.
Schuster TG, Cho B, Keller LM, Takayama S, Smith GD. Isolation of motile spermatozoa from semen samples using microfluidics. Reprod Biomed Online. 2003;7(1):75–81. https://doi.org/10.1016/s1472-6483(10)61732-4.
Nosrati R, Vollmer M, Eamer L, et al. Rapid selection of sperm with high DNA integrity. Lab Chip. 2014;14(6):1142–50. https://doi.org/10.1039/c3lc51254a.
Wu J-K, Chen P-C, Lin Y-N, Wang C-W, Pan L-C, Tseng F-G. High-throughput flowing upstream sperm sorting in a retarding flow field for human semen analysis. Analyst. 2017;142(6):938–44. https://doi.org/10.1039/c6an02420c.
Nagata MPB, Endo K, Ogata K, et al. Live births from artificial insemination of microfluidic-sorted bovine spermatozoa characterized by trajectories correlated with fertility. Proc Natl Acad Sci USA. 2018;115(14):E3087–96. https://doi.org/10.1073/pnas.1717974115.
Mangum CL, Patel DP, Jafek AR, et al. Towards a better testicular sperm extraction: novel sperm sorting technologies for non-motile sperm extracted by microdissection TESE. Transl Androl Urol. 2020;9(Suppl 2):S206–14. https://doi.org/10.21037/tau.2019.08.36.
Samuel R, Feng H, Jafek A, Despain D, Jenkins T, Gale B. Microfluidic-based sperm sorting & analysis for treatment of male infertility. Transl Androl Urol. 2018;7(Suppl 3):S336–47. https://doi.org/10.21037/tau.2018.05.08.
Schulte RT, Chung YK, Ohl DA, Takayama S, Smith GD. Microfluidic sperm sorting device provides a novel method for selecting motile sperm with higher DNA integrity. Fertil Steril. 2007;88:S76. https://doi.org/10.1016/j.fertnstert.2007.07.254.
Shirota K, Yotsumoto F, Itoh H, et al. Separation efficiency of a microfluidic sperm sorter to minimize sperm DNA damage. Fertil Steril. 2016;105(2):315-21.e1. https://doi.org/10.1016/j.fertnstert.2015.10.023.
Suh RS, Zhu X, Phadke N, Ohl DA, Takayama S, Smith GD. IVF within microfluidic channels requires lower total numbers and lower concentrations of sperm. Hum Reprod. 2006;21(2):477–83. https://doi.org/10.1093/humrep/dei323.
Zeringue HC, Beebe DJ. Microfluidic removal of cumulus cells from Mammalian zygotes. Methods Mol Biol. 2004;254:365–74. https://doi.org/10.1385/1-59259-741-6:365.
Lu Z, Zhang X, Leung C, Esfandiari N, Casper RF, Sun Y. Robotic ICSI (intracytoplasmic sperm injection). IEEE Trans Biomed Eng. 2011;58(7):2102–8. https://doi.org/10.1109/TBME.2011.2146781.
Mor A, Zhang M, Esencan E, et al. A step towards the automation of intracytoplasmic sperm injection: real time confirmation of mouse and human oocyte penetration and viability by electrical resistance measurement. Fertil Steril. 2020;113(1):234–6. https://doi.org/10.1016/j.fertnstert.2019.09.023.
Tran D, Cooke S, Illingworth PJ, Gardner DK. Deep learning as a predictive tool for fetal heart pregnancy following time-lapse incubation and blastocyst transfer. Hum Reprod. 2019;34(6):1011–8. https://doi.org/10.1093/humrep/dez064.
Fishel S, Campbell A, Montgomery S, et al. Time-lapse imaging algorithms rank human preimplantation embryos according to the probability of live birth. Reprod Biomed Online. 2018;37(3):304–13. https://doi.org/10.1016/j.rbmo.2018.05.016.
Khosravi P, Kazemi E, Zhan Q, et al. Deep learning enables robust assessment and selection of human blastocysts after in vitro fertilization. npj Digital Med. 2019;2(1):21. https://doi.org/10.1038/s41746-019-0096-y
Horcajadas JA, Gosálvez J, eds. Reproductomics: the -omics revolution and its impact on human reproductive medicine.
Practice committees of the American society for reproductive medicine and the society for assisted reproductive technology. Electronic address: ASRM@asrm.org, practice committees of the American society for reproductive medicine and the society for assisted reproductive technology. The use of preimplantation genetic testing for aneuploidy (PGT-A): a committee opinion. Fertil Steril. 2018;109(3):429–436. https://doi.org/10.1016/j.fertnstert.2018.01.002
Raty S, Walters EM, Davis J, et al. Embryonic development in the mouse is enhanced via microchannel culture. Lab Chip. 2004;4(3):186–90. https://doi.org/10.1039/b316437c.
Walters EM, Clark SG, Beebe DJ, Wheeler MB. Mammalian embryo culture in a microfluidic device. Methods Mol Biol. 2004;254:375–82. https://doi.org/10.1385/1-59259-741-6:375.
Han C, Zhang Q, Ma R, et al. Integration of single oocyte trapping, in vitro fertilization and embryo culture in a microwell-structured microfluidic device. Lab Chip. 2010;10(21):2848–54. https://doi.org/10.1039/c005296e.
Krisher RL, Wheeler MB. Towards the use of microfluidics for individual embryo culture. Reprod Fertil Dev. 2010;22(1):32–9. https://doi.org/10.1071/RD09219.
Heo YS, Cabrera LM, Bormann CL, Shah CT, Takayama S, Smith GD. Dynamic microfunnel culture enhances mouse embryo development and pregnancy rates. Hum Reprod. 2010;25(3):613–22. https://doi.org/10.1093/humrep/dep449.
Esteves TC, van Rossem F, Nordhoff V, Schlatt S, Boiani M, Le Gac S. A microfluidic system supports single mouse embryo culture leading to full-term development. RSC Adv. 2013;3(48):26451. https://doi.org/10.1039/c3ra44453h.
Heo YS, Cabrera LM, Song JW, et al. Characterization and resolution of evaporation-mediated osmolality shifts that constrain microfluidic cell culture in poly(dimethylsiloxane) devices. Anal Chem. 2007;79(3):1126–34. https://doi.org/10.1021/ac061990v.
Gardner DK, Balaban B. Assessment of human embryo development using morphological criteria in an era of time-lapse, algorithms and “OMICS”: is looking good still important? Mol Hum Reprod. 2016;22(10):704–18. https://doi.org/10.1093/molehr/gaw057.
Rosàs-Canyelles E, Modzelewski AJ, Geldert A, He L, Herr AE. Assessing heterogeneity among single embryos and single blastomeres using open microfluidic design. Sci Adv. 2020;6(17):eaay1751. https://doi.org/10.1126/sciadv.aay1751.
Urbanski JP, Johnson MT, Craig DD, Potter DL, Gardner DK, Thorsen T. Noninvasive metabolic profiling using microfluidics for analysis of single preimplantation embryos. Anal Chem. 2008;80(17):6500–7. https://doi.org/10.1021/ac8010473.
Heo YS, Cabrera LM, Bormann CL, Smith GD, Takayama S. Real time culture and analysis of embryo metabolism using a microfluidic device with deformation based actuation. Lab Chip. 2012;12(12):2240–6. https://doi.org/10.1039/c2lc21050a.
Yanez LZ, Camarillo DB. Microfluidic analysis of oocyte and embryo biomechanical properties to improve outcomes in assisted reproductive technologies. Mol Hum Reprod. 2017;23(4):235–47. https://doi.org/10.1093/molehr/gaw071.
Huang L, Bogale B, Tang Y, Lu S, Xie XS, Racowsky C. Noninvasive preimplantation genetic testing for aneuploidy in spent medium may be more reliable than trophectoderm biopsy. Proc Natl Acad Sci USA. 2019;116(28):14105–12. https://doi.org/10.1073/pnas.1907472116.
Roy TK, Brandi S, Tappe NM, et al. Embryo vitrification using a novel semi-automated closed system yields in vitro outcomes equivalent to the manual Cryotop method. Hum Reprod. 2014;29(11):2431–8. https://doi.org/10.1093/humrep/deu214.
Arav A, Natan Y, Kalo D, et al. A new, simple, automatic vitrification device: preliminary results with murine and bovine oocytes and embryos. J Assist Reprod Genet. 2018;35(7):1161–8. https://doi.org/10.1007/s10815-018-1210-9.
Canto MD, Moutier C, Brambillasca F, et al. Automated vitrification for embryo cryopreservation: preliminary comparative results and first live birth in Europe. Fertil Steril. 2019;112(3):e116–7. https://doi.org/10.1016/j.fertnstert.2019.07.425.
Heo YS, Lee H-J, Hassell BA, et al. Controlled loading of cryoprotectants (CPAs) to oocyte with linear and complex CPA profiles on a microfluidic platform. Lab Chip. 2011;11(20):3530–7. https://doi.org/10.1039/c1lc20377k.
Pyne DG, Liu J, Abdelgawad M, Sun Y. Digital microfluidic processing of mammalian embryos for vitrification. PLoS One. 2014;9(9):e108128. https://doi.org/10.1371/journal.pone.0108128.
Lai D, Ding J, Smith GW, Smith GD, Takayama S. Slow and steady cell shrinkage reduces osmotic stress in bovine and murine oocyte and zygote vitrification. Hum Reprod. 2015;30(1):37–45. https://doi.org/10.1093/humrep/deu284.
Guo Y, Yang Y, Yi X, Zhou X. Microfluidic method reduces osmotic stress injury to oocytes during cryoprotectant addition and removal processes in porcine oocytes. Cryobiology. 2019;90:63–70. https://doi.org/10.1016/j.cryobiol.2019.08.005.
Zhao G, Fu J. Microfluidics for cryopreservation. Biotechnol Adv. 2017;35(2):323–36. https://doi.org/10.1016/j.biotechadv.2017.01.006.
Smith GD, Takayama S. Cryopreservation and microfluidics: a focus on the oocyte. Reprod Fertil Dev. 2018;31(1):93–104. https://doi.org/10.1071/RD18326.
Yang Q, Zhu L, Jin L. Human follicle in vitro culture including activation, growth, and maturation: a review of research progress. Front Endocrinol (Lausanne). 2020;11:548. https://doi.org/10.3389/fendo.2020.00548.
McLaughlin M, Albertini DF, Wallace WHB, Anderson RA, Telfer EE. Metaphase II oocytes from human unilaminar follicles grown in a multi-step culture system. Mol Hum Reprod. 2018;24(3):135–42. https://doi.org/10.1093/molehr/gay002.
Laronda MM, Rutz AL, Xiao S, et al. A bioprosthetic ovary created using 3D printed microporous scaffolds restores ovarian function in sterilized mice. Nat Commun. 2017;8:15261. https://doi.org/10.1038/ncomms15261.
Salama M, Woodruff TK. From bench to bedside: current developments and future possibilities of artificial human ovary to restore fertility. Acta Obstet Gynecol Scand. 2019;98(5):659–64. https://doi.org/10.1111/aogs.13552.
Xiao S, Coppeta JR, Rogers HB, et al. A microfluidic culture model of the human reproductive tract and 28-day menstrual cycle. Nat Commun. 2017;8:14584. https://doi.org/10.1038/ncomms14584.
Nagamatsu G, Hayashi K. Stem cells, in vitro gametogenesis and male fertility. Reproduction. 2017;154(6):F79–91. https://doi.org/10.1530/REP-17-0510.
Yamashiro C, Sasaki K, Yabuta Y, et al. Generation of human oogonia from induced pluripotent stem cells in vitro. Science. 2018;362(6412):356–60. https://doi.org/10.1126/science.aat1674.
Ma H, O’Neil RC, Marti Gutierrez N, et al. Functional human oocytes generated by transfer of polar body genomes. Cell Stem Cell. 2017;20(1):112–9. https://doi.org/10.1016/j.stem.2016.10.001.
White YAR, Woods DC, Takai Y, Ishihara O, Seki H, Tilly JL. Oocyte formation by mitotically active germ cells purified from ovaries of reproductive-age women. Nat Med. 2012;18(3):413–21. https://doi.org/10.1038/nm.2669.
Woods DC, Tilly JL. Isolation, characterization and propagation of mitotically active germ cells from adult mouse and human ovaries. Nat Protoc. 2013;8(5):966–88. https://doi.org/10.1038/nprot.2013.047.
Wagner M, Yoshihara M, Douagi I, et al. Single-cell analysis of human ovarian cortex identifies distinct cell populations but no oogonial stem cells. Nat Commun. 2020;11(1):1147. https://doi.org/10.1038/s41467-020-14936-3.
Ibtisham F, Honaramooz A. Spermatogonial stem cells for in vitro spermatogenesis and in vivo restoration of fertility. Cells. 2020;9(3). https://doi.org/10.3390/cells9030745
Lei Q, Lai X, Eliveld J, Chuva de Sousa Lopes SM, van Pelt AMM, Hamer G. In vitro meiosis of male germline stem cells. Stem Cell Rep. 2020;15(5):1140–1153. https://doi.org/10.1016/j.stemcr.2020.10.006
Zhang XM, Wu K, Zheng Y, et al. In vitro expansion of human sperm through nuclear transfer. Cell Res. 2020;30(4):356–9. https://doi.org/10.1038/s41422-019-0265-1.
Zhang L, Bao Y, Riaz M, et al. Population genomic screening of all young adults in a health-care system: a cost-effectiveness analysis. Genet Med. 2019;21(9):1958–68. https://doi.org/10.1038/s41436-019-0457-6.
Turley P, Meyer MN, Wang N, et al. Problems with using polygenic scores to select embryos. N Engl J Med. 2021;385(1):78–86. https://doi.org/10.1056/NEJMsr2105065.
Jinek M, Chylinski K, Fonfara I, Hauer M, Doudna JA, Charpentier E. A programmable dual-RNA-guided DNA endonuclease in adaptive bacterial immunity. Science. 2012;337(6096):816–21. https://doi.org/10.1126/science.1225829.
Ma H, Marti-Gutierrez N, Park S-W, et al. Correction of a pathogenic gene mutation in human embryos. Nature. 2017;548(7668):413–9. https://doi.org/10.1038/nature23305.
Kang E, Wu J, Gutierrez NM, et al. Mitochondrial replacement in human oocytes carrying pathogenic mitochondrial DNA mutations. Nature. 2016;540(7632):270–5. https://doi.org/10.1038/nature20592.
Adashi EY, Cohen IG, Hanna JH, Surani AM, Hayashi K. Stem cell-derived human gametes: the public engagement imperative. Trends Mol Med. 2019;25(3):165–7. https://doi.org/10.1016/j.molmed.2019.01.005.
Adashi E, Cohen IG. Heritable genome editing-edited eggs and sperm to the rescue? JAMA. 2019;322(18):1754–5. https://doi.org/10.1001/jama.2019.17538.
Cohen IG, Daley GQ, Adashi EY. Disruptive reproductive technologies. Sci Transl Med. 2017;9(372). https://doi.org/10.1126/scitranslmed.aag2959
Cohen GI, Adashi EY. The FDA is prohibited from going germline. Science. August 2016.
Mastenbroek S, de Wert G, Adashi EY. The imperative of responsible innovation in reproductive medicine. N Engl J Med. 2021;385(22):2096–100. https://doi.org/10.1056/NEJMsb2101718.
Harper J, Jackson E, Sermon K, et al. Adjuncts in the IVF laboratory: where is the evidence for “add-on” interventions? Hum Reprod. 2017;32(3):485–91. https://doi.org/10.1093/humrep/dex004.
Special collection - in vitro fertilisation – effectiveness of add-ons | Cochrane Library. https://www.cochranelibrary.com/collections/doi/SC000046/full. Published July 15, 2021. Accessed Dec 6, 2021.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics Approval
Not applicable.
Consent to Participate
Not applicable.
Consent for Publication
The authors consent.
Conflict of Interest
Dr. Kushnir is an inventor on patents related to clinical use of recombinant anti-müllerian hormone and a consultant for medical insurance companies. Professor Smith is an inventor and jointly holds patents with the University of Michigan related to microfluidics and gamete isolation, in vitro fertilization, embryo culture and cryopreservation. Dr. Smith served as consultant for Overture Life.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kushnir, V.A., Smith, G.D. & Adashi, E.Y. The Future of IVF: The New Normal in Human Reproduction. Reprod. Sci. 29, 849–856 (2022). https://doi.org/10.1007/s43032-021-00829-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43032-021-00829-3