Abstract
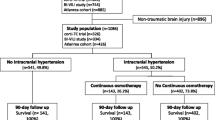
Osmotic therapy has been recognized as an important treatment option for patients with traumatic brain injury (TBI). Nevertheless, the effect of hypertonic saline (HTS) remains unknown, as findings are primarily based on a large database. This study aimed to elucidate the effect of HTS on the clinical outcomes of patients with TBI admitted to the intensive care unit (ICU). We retrospectively identified patients with moderate-to-severe TBI from two public databases: Medical Information Mart for Intensive Care (MIMIC)-IV and eICU Collaborative Research Database (eICU-CRD). A marginal structural Cox model (MSCM) was used, with time-dependent variates designed to reflect exposure over time during ICU stay. Trajectory modeling based on the intracranial pressure evolution pattern allowed for the identification of subgroups. Overall, 130 (6.65%) of 1955 eligible patients underwent HTS. MSCM indicated that the HTS significantly associated with higher infection complications (e.g., urinary tract infection (HR 1.88, 95% CI 1.26–2.81, p = 0.002)) and increased ICU LOS (HR 2.02, 95% CI 1.71–2.40, p < 0.001). A protective effect of HTS on GCS was found in subgroups with medium and low intracranial pressure. Our study revealed no significant difference in mortality between patients who underwent HTS and those who did not. Increased occurrence rates of infection and electrolyte imbalance are inevitable outcomes of continuous HTS infusion. Although the study suggests slight beneficial effects, including better neurological outcomes, these results warrant further validation.



Similar content being viewed by others
Data availability
Publicly available datasets were analyzed in this study. These data can be found in the physionet (https://physionet.org/content/mimiciv/1.0/; https://physionet.org/content/eicucrd/2.0/).
References
Myburgh JA, Cooper DJ, Finfer SR et al (2008) Epidemiology and 12-month outcomes from traumatic brain injury in australia and new zealand. J Trauma 64(4):854–862. https://doi.org/10.1097/TA.0b013e3180340e77
Dewan MC, Rattani A, Gupta S et al (2018) Estimating the global incidence of traumatic brain injury. J Neurosurg 130(4):1080–1097. https://doi.org/10.3171/2017.10.Jns17352
Rubiano AM, Carney N, Chesnut R, Puyana JC (2015) Global neurotrauma research challenges and opportunities. Nature 527(7578):S193–S197. https://doi.org/10.1038/nature16035
Global, regional, and national burden of neurological disorders, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol. 2019;18(5):459–480. https://doi.org/10.1016/s1474-4422(18)30499-x
Steyerberg EW, Wiegers E, Sewalt C et al (2019) Case-mix, care pathways, and outcomes in patients with traumatic brain injury in CENTER-TBI: a European prospective, multicentre, longitudinal, cohort study. Lancet Neurol 18(10):923–934. https://doi.org/10.1016/s1474-4422(19)30232-7
Diaz-Arrastia R, Kochanek PM, Bergold P et al (2014) Pharmacotherapy of traumatic brain injury: state of the science and the road forward: report of the Department of Defense Neurotrauma Pharmacology Workgroup. J Neurotrauma 31(2):135–158. https://doi.org/10.1089/neu.2013.3019
Juul N, Morris GF, Marshall SB, Marshall LF (2000) Intracranial hypertension and cerebral perfusion pressure: influence on neurological deterioration and outcome in severe head injury The Executive Committee of the International Selfotel Trial. J Neurosurg 92(1):1–6. https://doi.org/10.3171/jns.2000.92.1.0001
Ziai WC, Toung TJ, Bhardwaj A (2007) Hypertonic saline: first-line therapy for cerebral edema? J Neurol Sci 261(1–2):157–166. https://doi.org/10.1016/j.jns.2007.04.048
Kolmodin L, Sekhon MS, Henderson WR, Turgeon AF, Griesdale DE (2013) Hypernatremia in patients with severe traumatic brain injury: a systematic review. Ann Intensive Care 3(1):35. https://doi.org/10.1186/2110-5820-3-35
Vedantam A, Robertson CS, Gopinath SP (2017) Morbidity and mortality associated with hypernatremia in patients with severe traumatic brain injury. Neurosurg Focus 43(5):E2. https://doi.org/10.3171/2017.7.Focus17418
Kahle KT, Walcott BP, Simard JM (2013) Continuous hyperosmolar therapy for traumatic brain injury-associated cerebral edema: as good as it gets, or an iatrogenic secondary insult? J Clin Neurosci 20(1):30–31. https://doi.org/10.1016/j.jocn.2012.10.004
Griesdale DE, Sekhon MS, Henderson WR (2013) Hypernatremia and intracranial pressure: more questions than answers. Crit Care 17(1):401
Tan SK, Kolmodin L, Sekhon MS, et al. (2016) The effect of continuous hypertonic saline infusion and hypernatremia on mortality in patients with severe traumatic brain injury: a retrospective cohort study. Canadian journal of anaesthesia = Journal canadien d'anesthesie 63(6):664–73. Effet d'une perfusion saline hypertonique continue et de l'hypernatrémie sur la mortalité de patients souffrant d'un traumatisme cérébral grave: une étude de cohorte rétrospective. https://doi.org/10.1007/s12630-016-0633-y
Goldberger AL, Amaral LA, Glass L et al (2000) PhysioBank, PhysioToolkit, and PhysioNet: components of a new research resource for complex physiologic signals. Circulation 101(23):E215–E220. https://doi.org/10.1161/01.cir.101.23.e215
Pollard TJ, Johnson AEW, Raffa JD, Celi LA, Mark RG, Badawi O (2018) The Eicu Collaborative Research Database, a freely available multi-center database for critical care research. Sci Data 5:180178. https://doi.org/10.1038/sdata.2018.178
Benchimol EI, Smeeth L, Guttmann A et al (2015) The REporting of studies Conducted using Observational Routinely-collected health Data (RECORD) statement. PLoS Med 12(10):e1001885. https://doi.org/10.1371/journal.pmed.1001885
Cole SR, Hernán MA, Margolick JB, Cohen MH, Robins JM (2005) Marginal structural models for estimating the effect of highly active antiretroviral therapy initiation on CD4 cell count. Am J Epidemiol 162(5):471–478. https://doi.org/10.1093/aje/kwi216
Nagin DS, Odgers CL (2010) Group-based trajectory modeling in clinical research. Annu Rev Clin Psychol 6:109–138. https://doi.org/10.1146/annurev.clinpsy.121208.131413
Pedersen AB, Mikkelsen EM, Cronin-Fenton D et al (2017) Missing data and multiple imputation in clinical epidemiological research. Clin Epidemiol 9:157–166. https://doi.org/10.2147/clep.S129785
VanderWeele TJ, Ding P (2017) Sensitivity Analysis in Observational Research: Introducing the E-Value. Ann Intern Med 167(4):268–274. https://doi.org/10.7326/m16-2607
Haneuse S, VanderWeele TJ, Arterburn D (2019) Using the E-Value to Assess the Potential Effect of Unmeasured Confounding in Observational Studies. JAMA 321(6):602–603. https://doi.org/10.1001/jama.2018.21554
Riha HM, Erdman MJ, Vandigo JE et al (2017) Impact of Moderate Hyperchloremia on Clinical Outcomes in Intracerebral Hemorrhage Patients Treated With Continuous Infusion Hypertonic Saline: A Pilot Study. Crit Care Med 45(9):e947–e953. https://doi.org/10.1097/ccm.0000000000002522
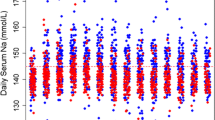
Harrois A, Anstey JR, van der Jagt M et al (2021) Variability in Serum Sodium Concentration and Prognostic Significance in Severe Traumatic Brain Injury: A Multicenter Observational Study. Neurocrit Care 34(3):899–907. https://doi.org/10.1007/s12028-020-01118-8
Maas AI, Steyerberg EW, Marmarou A et al (2010) IMPACT recommendations for improving the design and analysis of clinical trials in moderate to severe traumatic brain injury. Neurotherapeutics 7(1):127–134. https://doi.org/10.1016/j.nurt.2009.10.020
Zhang H, Liu J, Liu Y et al (2020) Hypertonic saline improves brain edema resulting from traumatic brain injury by suppressing the NF-Κb/IL-1β signaling pathway and AQP4. Exp Ther Med 20(5):71. https://doi.org/10.3892/etm.2020.9199
Roquilly A, Moyer JD, Huet O et al (2021) Effect of Continuous Infusion of Hypertonic Saline vs Standard Care on 6-Month Neurological Outcomes in Patients With Traumatic Brain Injury: The COBI Randomized Clinical Trial. JAMA 325(20):2056–2066. https://doi.org/10.1001/jama.2021.5561
Asehnoune K, Lasocki S, Seguin P et al (2017) Association between continuous hyperosmolar therapy and survival in patients with traumatic brain injury - a multicentre prospective cohort study and systematic review. Critical care (London, England) 21(1):328. https://doi.org/10.1186/s13054-017-1918-4
Chabok SY, Yazdanshenas H, Naeeni AF et al (2014) The impact of body mass index on treatment outcomes among traumatic brain injury patients in intensive care units. Eur J Trauma Emerg Surg 40(1):51–55. https://doi.org/10.1007/s00068-013-0314-2
Brown CV, Rhee P, Neville AL, Sangthong B, Salim A, Demetriades D (2006) Obesity and traumatic brain injury. J Trauma 61(3):572–576. https://doi.org/10.1097/01.ta.0000200842.19740.38
Coritsidis G, Diamond N, Rahman A et al (2015) Hypertonic saline infusion in traumatic brain injury increases the incidence of pulmonary infection. J Clin Neurosci 22(8):1332–1337. https://doi.org/10.1016/j.jocn.2015.02.025
Skrifvars MB, Bailey M, Moore E et al (2021) A Post Hoc Analysis of Osmotherapy Use in the Erythropoietin in Traumatic Brain Injury Study-Associations With Acute Kidney Injury and Mortality. Crit Care Med 49(4):e394–e403. https://doi.org/10.1097/ccm.0000000000004853
Simma B, Burger R, Falk M, Sacher P, Fanconi S (1998) A prospective, randomized, and controlled study of fluid management in children with severe head injury: lactated Ringer’s solution versus hypertonic saline. Crit Care Med 26(7):1265–1270. https://doi.org/10.1097/00003246-199807000-00032
Froelich M, Ni Q, Wess C, Ougorets I, Härtl R (2009) Continuous hypertonic saline therapy and the occurrence of complications in neurocritically ill patients. Crit Care Med 37(4):1433–1441. https://doi.org/10.1097/CCM.0b013e31819c1933
Bulger EM, Cuschieri J, Warner K, Maier RV (2007) Hypertonic resuscitation modulates the inflammatory response in patients with traumatic hemorrhagic shock. Ann Surg 245(4):635–641. https://doi.org/10.1097/01.sla.0000251367.44890.ae
Gabella BA, Hathaway JE, Hume B et al (2021) Multisite medical record review of emergency department visits for traumatic brain injury. Inj Prev 27(S1):i42–i48. https://doi.org/10.1136/injuryprev-2019-043510
Warwick J, Slavova S, Bush J, Costich J (2020) Validation of ICD-10-CM surveillance codes for traumatic brain injury inpatient hospitalizations. Brain Inj 34(13–14):1763–1770. https://doi.org/10.1080/02699052.2020.1849801
Acknowledgements
We would like to thank the Massachusetts Institute of Technology and the Beth Israel Deaconess Medical Center for the MIMIC project. We also would like to thank the Philips Eicu Research Institute and Philips Healthcare for their contribution to the Eicu-CRD project.
Funding
This study received the following funding: The San Hang Program of Naval Medical University and Clinical Research Program of Shanghai Municipal Health Commission (202340037).
Author information
Authors and Affiliations
Contributions
FY, LJC, and LB collected, analyzed and interpreted the data regarding the tracheostomy in trauma patients. CP designed the study, and was a major contributor in writing the manuscript. MC performed the statistical analysis. LP, LS, and ZJ participated in the revision of the draft. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethical approval and consent to participate
The MIMIC-IV and Eicu database were approved by the Massachusetts Institute of Technology (Cambridge, MA) and Beth Israel Deaconess Medical Center (Boston, MA), and consent was obtained for the original data collection.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Chi Peng, Lijie Chi, Mengjie Chen, and Liwei Peng contributed equally to this work and are co-first authors.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Peng, C., Chi, L., Chen, M. et al. Effect of continuous hypertonic saline infusion on clinical outcomes in patients with traumatic brain injury. Neurosurg Rev 47, 78 (2024). https://doi.org/10.1007/s10143-024-02316-0
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10143-024-02316-0