Abstract
Purpose
To identify risk factors for major postoperative complications in meningioma patients and to construct and validate a nomogram that identify patients at high risk of these complications.
Methods
The medical records of meningioma patients who underwent surgical resection in our hospital from January 2018 to December 2020 were collected. The patients were divided into a training set (815 cases from the main campus in 2018 and 2019) and a validation set (300 cases from two other campuses in 2020). Major postoperative complications were defined as any new neurological deficits and complications classified as Clavien-Dindo Grading (CDG) II or higher. Univariate and multivariate analyses were conducted using the training set to identify independent risk factors. A nomogram was constructed based on these results. And then validated the nomogram through bootstrap re-sampling in both the training and validation sets. The concordance index (C-index) and the area under the curve (AUC) were used to assess the discriminative ability of the nomogram. The Hosmer–Lemeshow test was performed to evaluate the goodness-of-fit. The optimal cutoff point for the nomogram was calculated using Youden’s index.
Results
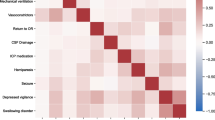
In the training set, 135 cases (16.56%) experienced major postoperative complications. The independent risk factors identified were male sex, recurrent tumors, American Society of Anesthesiologists (ASA) class III–IV, preoperative Karnofsky Performance Scale (KPS) score < 80, preoperative serum albumin < 35 g/L, tumor in the skull base or central sulcus area, subtotal tumor resection (STR), allogeneic blood transfusion, and larger tumor size. A nomogram was constructed based on these risk factors. It demonstrated good predictive performance, with a C-index of 0.919 for the training set and 0.872 for the validation set. The area under the curve (AUC) > 0.7 indicated satisfactory discriminative ability. The Hosmer–Lemeshow test showed no significant deviation from the predicted probabilities. And the cutoff for nomogram total points was about 200 (specificity 0.881 and sensitivity 0.834).
Conclusions
The constructed nomogram demonstrated robust predictive performance for major postoperative complications in meningioma patients. This model can be used by surgeons as a reference in clinical decision-making.



Similar content being viewed by others
Data availability
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Change history
27 December 2023
A Correction to this paper has been published: https://doi.org/10.1007/s10143-023-02253-4
References
Ostrom QT, Patil N, Cioffi G, Waite K, Kruchko C, Barnholtz-Sloan JS (2020) CBTRUS statistical report: primary brain and other central nervous system tumors diagnosed in the United States in 2013–2017. Neuro Oncol 22:iv1–iv96. https://doi.org/10.1093/neuonc/noaa200
Bateman BT, Pile-Spellman J, Gutin PH, Berman MF (2005) Meningioma resection in the elderly: nationwide inpatient sample, 1998–2002. Neurosurgery 57:866–872. https://doi.org/10.1227/01.neu.0000179923.66729.87. (discussion 866-872)
Goldbrunner R, Minniti G, Preusser M, Jenkinson MD, Sallabanda K, Houdart E, von Deimling A, Stavrinou P, Lefranc F, Lund-Johansen M, Moyal EC-J, Brandsma D, Henriksson R, Soffietti R, Weller M (2016) EANO guidelines for the diagnosis and treatment of meningiomas. Lancet Oncol 17:e383–e391. https://doi.org/10.1016/s1470-2045(16)30321-7
Lemee JM, Corniola MV, Da Broi M, Schaller K, Meling TR (2019) Early postoperative complications in meningioma: predictive factors and impact on outcome. World Neurosurg 128:e851–e858. https://doi.org/10.1016/j.wneu.2019.05.010
Isobe N, Ikawa F, Tominaga A, Kuroki K, Sadatomo T, Mizoue T, Hamasaki O, Matsushige T, Abiko M, Mitsuhara T, Kinoshita Y, Takeda M, Kurisu K (2018) Factors related to frailty associated with clinical deterioration after meningioma surgery in the elderly. World Neurosurg 119:e167–e173. https://doi.org/10.1016/j.wneu.2018.07.080
Jenkins FS, Vasella F, Padevit L, Mutschler V, Akeret K, Velz J, Regli L, Sarnthein J, Neidert MC (2021) Preoperative risk factors associated with new focal neurological deficit and other major adverse events in first-time intracranial meningioma neurosurgery. Acta Neurochir (Wien) 163:2871–2879. https://doi.org/10.1007/s00701-021-04897-x
Zeng L, Wang L, Ye F, Chen J, Lei T, Chen J (2015) Clinical characteristics of patients with asymptomatic intracranial meningiomas and results of their surgical management. Neurosurg Rev 38:481–488. https://doi.org/10.1007/s10143-015-0619-1. (discussion 488)
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240:205–213. https://doi.org/10.1097/01.sla.0000133083.54934.ae
Sarnthein J, Stieglitz L, Clavien PA, Regli L (2016) A patient registry to improve patient safety: recording general neurosurgery complications. Plos One 11:e0163154. https://doi.org/10.1371/journal.pone.0163154
Landriel Ibanez FA, Hem S, Ajler P, Vecchi E, Ciraolo C, Baccanelli M, Tramontano R, Knezevich F, Carrizo A (2011) A new classification of complications in neurosurgery. World Neurosurg 75:709–715. https://doi.org/10.1016/j.wneu.2010.11.010. (discussion 604-711)
Terrapon APR, Zattra CM, Voglis S, Velz J, Vasella F, Akeret K, Held U, Schiavolin S, Bozinov O, Ferroli P, Broggi M, Sarnthein J, Regli L, Neidert MC (2021) Adverse events in neurosurgery: the novel therapy-disability-neurology grade. Neurosurgery 89:236–245. https://doi.org/10.1093/neuros/nyab121
Li Y, Lu D, Feng D, Cheng H, Huang Q, Zhao H, Chen P, Qin H, Cai Q (2020) Management of incidental anterior skull base large and giant meningiomas in elderly patients. J Neurooncol 148:481–488. https://doi.org/10.1007/s11060-020-03484-x
Demonte F, Mcdermott MW, Almefty O (2011) Al-Mefty’s meningiomas. Thieme Medical, New York
Louis DN, Perry A, Reifenberger G, von Deimling A, Figarella-Branger D, Cavenee WK, Ohgaki H, Wiestler OD, Kleihues P, Ellison DW (2016) The 2016 World Health Organization Classification of Tumors of the Central Nervous System: a summary. Acta Neuropathol 131:803–820. https://doi.org/10.1007/s00401-016-1545-1
Caroli M, Locatelli M, Prada F, Beretta F, Martinelli-Boneschi F, Campanella R, Arienta C (2005) Surgery for intracranial meningiomas in the elderly: a clinical-radiological grading system as a predictor of outcome. J Neurosurg 102:290–294. https://doi.org/10.3171/jns.2005.102.2.0290
Sacko O, Sesay M, Roux FE, Riem T, Grenier B, Liguoro D, Loiseau H (2007) Intracranial meningioma surgery in the ninth decade of life. Neurosurgery 61:950–954. https://doi.org/10.1227/01.neu.0000303190.80049.7d. (discussion 955)
Wilson TA, Huang L, Ramanathan D, Lopez-Gonzalez M, Pillai P, De Los RK, Kumal M, Boling W (2020) Review of atypical and anaplastic meningiomas: classification, molecular biology, and management. Front Oncol 10:565582. https://doi.org/10.3389/fonc.2020.565582
Eksi MS, Canbolat C, Akbas A, Ozmen BB, Akpinar E, Usseli MI, Gungor A, Guduk M, Hacihanefioglu M, Ersen Danyeli A, Ozduman K, Pamir MN (2019) Elderly patients with intracranial meningioma: surgical considerations in 228 patients with a comprehensive analysis of the literature. World Neurosurg 132:e350–e365. https://doi.org/10.1016/j.wneu.2019.08.150
Chen ZY, Zheng CH, Tang L, Su XY, Lu GH, Zhang CY, Xiao SW, Tan YF (2015) Intracranial meningioma surgery in the elderly (over 65 years): prognostic factors and outcome. Acta Neurochir (Wien) 157:1549–1557. https://doi.org/10.1007/s00701-015-2502-9. (discussion 1557)
Gousias K, Schramm J, Simon M (2016) The Simpson grading revisited: aggressive surgery and its place in modern meningioma management. J Neurosurg 125:551–560. https://doi.org/10.3171/2015.9.JNS15754
Song X, Zeng C, Wang M, Wang W, Lin F, He Q, Cao Y, Wang S, Zhao J (2021) Clinical characteristics and risk factors of perioperative outcomes in elderly patients with intracranial tumors. Neurosurg Rev 44:389–400. https://doi.org/10.1007/s10143-019-01217-x
Zhao X, Zhao D, Wu Y, Gao W, Cui H, Wang Y, Nakaji P, Bao Y (2018) Meningioma in the elderly: characteristics, prognostic factors, and surgical strategy. J Clin Neurosci 56:143–149. https://doi.org/10.1016/j.jocn.2018.06.011
Yamamoto J, Takahashi M, Idei M, Nakano Y, Soejima Y, Akiba D, Kitagawa T, Ueta K, Miyaoka R, Nishizawa S (2017) Clinical features and surgical management of intracranial meningiomas in the elderly. Oncol Lett 14:909–917. https://doi.org/10.3892/ol.2017.6174
Kolakshyapati M, Ikawa F, Abiko M, Mitsuhara T, Kinoshita Y, Takeda M, Kurisu K, Alumni Association Group of the Department of Neurosurgery at Hiroshima U (2018) Multivariate risk factor analysis and literature review of postoperative deterioration in Karnofsky Performance Scale score in elderly patients with skull base meningioma. Neurosurg Focus 44:E14. https://doi.org/10.3171/2018.1.FOCUS17730
Rogers L, Barani I, Chamberlain M, Kaley TJ, McDermott M, Raizer J, Schiff D, Weber DC, Wen PY, Vogelbaum MA (2015) Meningiomas: knowledge base, treatment outcomes, and uncertainties. A RANO review. J Neurosurg 122:4–23. https://doi.org/10.3171/2014.7.JNS131644
Magill ST, Lee DS, Yen AJ, Lucas CG, Raleigh DR, Aghi MK, Theodosopoulos PV, McDermott MW (2018) Surgical outcomes after reoperation for recurrent skull base meningiomas. J Neurosurg 130:876–883. https://doi.org/10.3171/2017.11.JNS172278
Magill ST, Dalle Ore CL, Diaz MA, Jalili DD, Raleigh DR, Aghi MK, Theodosopoulos PV, McDermott MW (2018) Surgical outcomes after reoperation for recurrent non-skull base meningiomas. J Neurosurg: 1–9 https://doi.org/10.3171/2018.6.JNS18118
Meling TR, Da Broi M, Scheie D, Helseth E (2019) Skull base versus non-skull base meningioma surgery in the elderly. Neurosurg Rev 42:961–972. https://doi.org/10.1007/s10143-018-1005-6
Narayan V, Bir SC, Mohammed N, Savardekar AR, Patra DP, Nanda A (2018) Surgical management of giant intracranial meningioma: operative nuances, challenges, and outcome. World Neurosurg 110:e32–e41. https://doi.org/10.1016/j.wneu.2017.09.184
Jumah F, AbuRmilah A, Raju B, Jaber S, Adeeb N, Narayan V, Sun H, Cuellar H, Gupta G, Nanda A (2021) Does preoperative embolization improve outcomes of meningioma resection? Neurosurg Rev, A systematic review and meta-analysis. https://doi.org/10.1007/s10143-021-01519-z
Przybylowski CJ, Zhao X, Baranoski JF, Borba Moreira L, Gandhi S, Chapple KM, Almefty KK, Sanai N, Ducruet AF, Albuquerque FC, Little AS, Nakaji P (2020) Preoperative embolization versus no embolization for WHO grade I intracranial meningioma: a retrospective matched cohort study. J Neurosurg: 1–8 https://doi.org/10.3171/2020.1.JNS19788
Yoon N, Shah A, Couldwell WT, Kalani MYS, Park MS (2018) Preoperative embolization of skull base meningiomas: current indications, techniques, and pearls for complication avoidance. Neurosurg Focus 44:E5. https://doi.org/10.3171/2018.1.FOCUS17686
Dincer A, Jalal MI, Gupte TP, Vetsa S, Vasandani S, Yalcin K, Marianayagam N, Blondin N, Corbin Z, McGuone D, Fulbright RK, Erson-Omay Z, Günel M, Moliterno J (2023) The clinical and genomic features of seizures in meningiomas. Neurooncol Adv 5:i49–i57. https://doi.org/10.1093/noajnl/vdac110
Schwartz TH, McDermott MW (2020) The Simpson grade: abandon the scale but preserve the message. J Neurosurg: 1–8 https://doi.org/10.3171/2020.6.Jns201904
Cataldi S, Bruder N, Dufour H, Lefevre P, Grisoli F, Francois G (1997) Intraoperative autologous blood transfusion in intracranial surgery. Neurosurgery 40:765–771. https://doi.org/10.1097/00006123-199704000-00021. (discussion 771-762)
Patil H, Garg N, Navakar D, Banabokade L (2018) Clinical experience of autologous blood transfusion in neurosurgery: prospective study in Central India. World Neurosurg 115:e539–e543. https://doi.org/10.1016/j.wneu.2018.04.091
Cohen-Inbar O, Sviri GE, Soustiel JF, Zaaroor M (2011) The Geriatric Scoring System (GSS) in meningioma patients–validation. Acta Neurochir (Wien) 153:1501–1508. https://doi.org/10.1007/s00701-011-1034-1. (discussion 1508)
Adachi K, Kawase T, Yoshida K, Yazaki T, Onozuka S (2009) ABC Surgical Risk Scale for skull base meningioma: a new scoring system for predicting the extent of tumor removal and neurological outcome. Clinical article. J Neurosurg 111:1053–1061. https://doi.org/10.3171/2007.11.17446
Funding
This work was supported by the Natural Science Foundation of Tongji Hospital (No. 2020JZKT420).
Author information
Authors and Affiliations
Contributions
Zheng-Qian Guo conceived the project. Dan Cao collected the medical records from the database. Xiao-Yu Xia analyzed the data. Zheng-Qian Guo wrote the main manuscript text. Xu Chen, Yue He, and Bao-Feng Wang reviewed and edited the manuscript. Jian Chen and Dong-Sheng Guo supervised all the research work. All the authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethical approval
This study was approved by the ethics committee of Tongji Hospital, Tongji Medical College, Huazhong University of Science and Technology. The use of the clinical data was conducted in conformity with the institutional review boards.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Prof. Bao-Feng Wang, Prof. Dong-Sheng Guo and Prof. Jian Chen contributed equally to this paper.
The original online version of this article was revised: The authors regret that Figure 2 is missing in the published article.
The original article has been corrected.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Guo, ZQ., Xia, XY., Cao, D. et al. A nomogram for predicting the risk of major postoperative complications for patients with meningioma. Neurosurg Rev 46, 288 (2023). https://doi.org/10.1007/s10143-023-02198-8
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10143-023-02198-8