Abstract
Despite the importance of functional outcome, only a few scoring systems exist to predict neurologic outcome in meningioma surgery. Therefore, our study aims to identify preoperative risk factors and develop the receiver operating characteristics (ROC) models estimating the risk of a new postoperative neurologic deficit and a decrease in Karnofsky performance status (KPS). A multicentric study was conducted in a cohort of 552 consecutive patients with skull base meningiomas who underwent surgical resection from 2014 to 2019. Data were gathered from clinical, surgical, and pathology records as well as radiological diagnostics. The preoperative predictive factors of functional outcome (neurologic deficit, decrease in KPS) were analyzed in univariate and multivariate stepwise selection analyses. Permanent neurologic deficits were present in 73 (13.2%) patients and a postoperative decrease in KPS in 84 (15.2%). Surgery-related mortality was 1.3%. A ROC model was developed to estimate the probability of a new neurologic deficit (area 0.74; SE 0.0284; 95% Wald confidence limits (0.69; 0.80)) based on meningioma location and diameter. Consequently, a ROC model was developed to predict the probability of a postoperative decrease in KPS (area 0.80; SE 0.0289; 95% Wald confidence limits (0.74; 0.85)) based on the patient’s age, meningioma location, diameter, presence of hyperostosis, and dural tail. To ensure an evidence-based therapeutic approach, treatment should be founded on known risk factors, scoring systems, and predictive models. We propose ROC models predicting the functional outcome of skull base meningioma resection based on the age of the patient, meningioma size, and location and the presence of hyperostosis and dural tail.
Similar content being viewed by others
Introduction
Meningiomas are the most frequent primary intracranial and central nervous system tumors [1]. Treatment modalities consist of observation, surgical resection, stereotactic radiosurgery (SRS), fractionated external beam radiotherapy (EBRT), and pharmacotherapy [2]. Shortly, the therapeutic approach will be refined by recent advances in molecular genetics [2]. In 2017, Sahm et al. introduced DNA methylation-based classification, which has high power to predict meningioma prognosis and recurrence [3]. Additionally, molecular markers as grading criteria for selected meningioma subtypes were introduced by the 2021 World Health Organization (WHO) classification [4].
Although recent advances in molecular genetics enable better patient stratification, surgical decision-making is based on preoperative predictive factors in a patient with newly diagnosed meningioma [3, 4]. For symptomatic or progressive meningiomas, the first-line treatment option in contemporary practice is a maximal safe resection [2]. In a recent series, the reported rates of neurologic morbidity and mortality are 3.9–13.7% and 0–5.4%, respectively [5,6,7]. Meling et al. documented a significantly higher risk of postoperative neurologic deterioration (21 vs. 13%) in skull base meningiomas (SBMs) compared to non-skull base meningiomas (nSBMs) [8]. This risk is especially apparent in SBMs because of their close relationship to critical neurovascular structures [9].
Despite the importance of the functional outcome, only several studies have focused on the prognostic factors in meningioma surgery [5, 7, 8, 10,11,12,13,14,15]. Moreover, only a few scoring systems exist to predict neurologic outcome [6, 16,17,18,19]. Our study aims to identify preoperative factors predicting the functional outcome of SBM resection. Thus, based on the risk factors identified, the ROC models estimating the risk of a new postoperative neurologic deficit and a decrease in KPS are developed and compared to the existing scoring systems in the literature review.
Material and methods
In this multicentric study 552 consecutive patients who underwent SBM resection from January 1, 2014 to December 31, 2019 were investigated. The data were collected retrospectively from January 1, 2014 to June 30, 2018 and prospectively from July 1, 2018 to December 31, 2019. Our analysis included data from six neurosurgical centers in the Czech Republic (Military University Hospital Prague, 260 patients; Pilsen University Hospital, 76 patients; Liberec Hospital, 69 patients; Ceske Budejovice Hospital, 63 patients; University Hospital Olomouc, 44 patients; and University Hospital Ostrava, 40 patients). Data were gathered from clinical, surgical, and pathology records as well as radiological diagnostic (magnetic resonance imaging [MRI] scans, computed tomography scans, digital subtraction angiography); subsequently, all data were anonymized. Radiological findings were evaluated by two independent senior radiologists (VS and JM). The degree of resection in the surgical records was estimated using the Simpson grading system. However, the extent of resection was consequently verified on early baseline postoperative MRI. Clinical and radiological controls were performed according to protocols of individual departments, but at least regularly once a year.
The following information was included in the database:
-
General characteristics: patient age, sex, date of birth, date of resection, and follow-up duration.
-
Preoperative status: symptoms (patient’s subjective perceptions suggesting bodily defect or malfunction), signs (objective indications of disease) and their duration (days, months etc.), preoperative Glasgow Coma Scale (GCS), [20] and the Karnofsky performance status (KPS) [21].
-
Radiological characteristics: meningioma diameter, dimensions (a, b, c), volume, location, shape, margins, tumor-brain interface, presence of arachnoid plane, arachnoid cistern of SBM origin, edema, enhancement, capsular enhancement, dural tail, vessel encasement/narrowing, cavernous sinus invasion, cysts, sunburst sign, bone invasion, and hyperostosis (Table 1).
-
Surgery: surgical approach, Simpson grade of resection, [22] complications, and surgical revisions.
-
Histopathological analysis: WHO grade. Histopathological diagnoses were performed using the 2007 and 2016 WHO classifications [23, 24].
-
Clinical outcome: evolution of preoperative symptoms and signs (improved, stable, worsened), new neurologic deficits (temporary or permanent, evaluated 1 year after surgical resection), KPS, and the Glasgow Outcome Scale (GOS) [25].
-
Radiological outcome: tumor progression date and recurrence date.
-
Further therapeutical management: SRS, EBRT, and surgical resection.
Outcome measures
We further defined functional outcome as favorable (absence of a new neurologic deficit, increased or unchanged KPS) or unfavorable (presence of a new neurologic deficit, decrease of KPS ≥10). Predictive factors of unfavorable clinical outcome were analyzed.
Literature review
To summarize known risk factors, surgical risk scales and grading systems for functional outcome in meningioma (or only SBM) surgery a PubMed search were performed for entries until July 3, 2022, using the following query guidelines: 1) (meningioma) AND (grading system) AND (outcome) with 237 results; 2) (meningioma) AND (surgical scale) with 418 results; and 3) (meningioma) AND (risk factors) AND ((functional outcome) OR (neurologic outcome) OR (clinical outcome)) with 330 results. Case reports, non-English studies, conference papers, and abstracts were not included. Exclusion criteria were selective anatomical location and histological meningioma variants, patient subgroup (e.g., elderly), and extracranial meningioma location. From a search of other relevant resources, the grading system CLASS algorithm was included (Lee et al.) [6]. The Milan Complexity Scale was included in the review because of its importance, although other brain tumors were included [18].
Statistical analysis
Baseline data are presented descriptively as means and standard deviations (SDs) for normal distributions, median, and interquartile range for non-normally distributed data and absolute and relative frequencies for qualitative variables as summary statistics. Inferential statistical analysis was done using logistic regression (univariate and multivariate stepwise selections). Group comparisons were performed employing Wilcoxon rank sum tests and the Kruskal–Wallis test for more than two groups. The relationship between numerical parameters was investigated by correlation analysis using the Spearman rank correlation coefficient and chi-square test for qualitative variables. All inferential statistics were presented with appropriate 95% confidence intervals and reported along with their p-values. SAS version 9.4 (SAS Institute Inc., Cary, NC, USA) software was used for all statistical analyses. For all hypotheses tested, a p-value < 0.05 indicated statistical significance. All tests were performed as two sided. No adjustment for multiple comparisons was made because there is no single primary hypothesis.
Ethics approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the Ethical Committee of University Hospital in Ostrava (reference number 530/2018) and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Results
From January 1, 2014 to December 31, 2019, 552 consecutive patients underwent surgical resection for SBMs. The cohort contained 423 women (76.6%) and 129 men (23.4%). The mean age of patients at surgery was 56.8 (range 20–85, median 58) years. The mean preoperative KPS was 90 (median 90). Objective neurological deficits were documented in 355 patients (64.3%). The average duration of clinical signs or symptoms was 56 months. Radiological characteristics are outlined in Table 2. Some 452 meningiomas (81.9%) were supratentorial and 100 (18.1%) infratentorial. The average diameter was 3.1 cm and the average volume was 22.7 cm3. The extent of resection followed Simpson grade (S) I in 87 (16.9%), SII in 321 (58.2%), SIII in 34 (6.2%), SIV in 109 (19.7%), and SV in 1 (0.2%) patient. Histological analysis revealed grade 1 meningiomas in 511 (92.6%) and grade 2 in 41 (7.4%) cases.
For statistical analysis, due to the limited number of patients with SBM in rare locations, these locations were considered together with meningiomas in adjacent locations: tuberculum sellae with sella turcica, posterior clinoid process with petrous, petroclival with clival, and jugular foramen with cerebellopontine angle meningiomas (Table 3).
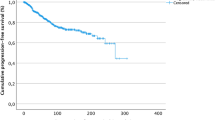
Clinical outcome
Overall survival (OS) at 1 and 2 years was 98.1% (average follow-up 27.7 months). The distribution of GOS in the cohort of our patients was as follows: 5 in 436 (79.0%), 4 in 85 (15.4%), 3 in 16 (2.9%), 2 in 5 (0.9%), and 1 in 10 (1.8%) patients. Surgery-related mortality was present in seven cases (1.3%) and not surgery-related in three cases (0.5%). The mean KPS at discharge was 89 (median 90). The KPS remained unchanged or increased in 468 (84.8%) patients and decreased in 84 (15.2%). The neurologic deficit, present initially in 355 patients, improved in 158 (44.5%), remained unchanged in 159 (44.8%), and worsened in 38 (10.7%). Temporary and permanent neurologic deficits were observed in 57 (10.3%) and 73 (13.2%) patients, respectively. The temporary neurologic deficits were CN palsy in 27 (4.9%, the most common oculomotor nerve palsy in 16 patients; 2.9%), motor deficit in 10 (1.8%), speech disorder in 9 (1.6%), cognitive decline in 4 (0.7%), somatosensory deficit in 2 (0.4%), cerebellar signs in 2 (0.4%), and higher cortical function deterioration in 2 patients (0.4%). Epileptic seizure was recorded in 7 patients (1.3%). The permanent neurologic deficits were CN palsy in 52 (9.4%; the most common oculomotor nerve palsy in 48 patients; 8.7%), motor deficit in 12 (2.2%), cognitive decline in 7 (1.3%), speech disorder in 4 (0.7%), higher cortical function deficit in 2 (0.4%), cerebellar signs in 2 (0.4%), and somatosensory deficit in 2 (0.4%). Secondary epilepsy was present in 3 patients (0.5%).
Predictive factors of clinical outcome
Predictive factors associated with a new neurologic deficit (temporary or permanent, evaluated at 1 year from surgical resection) and a decrease in KPS (at patient discharge) in univariate analysis are listed in Table 4.
The predictive factors of a new neurologic deficit (temporary or permanent, evaluated at 1 year from surgical resection) and a decrease in KPS (at patient discharge) selected by the multivariate stepwise selection model are presented in Table 5.
New neurological deficit
According to univariate analysis (done by the logistic regression univariate model), the risk factors associated with higher probability of a new neurologic deficit were the following: presence of major vessel contact, higher diameter, higher volume, supratentorial location, presence of cavernous sinus invasion, presence of vessel narrowing, and presence of edema. Considering the location and arachnoid cistern of origin, there were statistically significant differences in the risk of new neurologic deficit among the subgroups.
In multivariate analysis (done by the multivariate stepwise selection logistic regression model), higher diameter (p = 0.0043) and higher volume (p = 0.0406) were associated with higher probability of a new neurologic deficit. Considering the location (p < 0.0001), the lowest probability of a new neurologic deficit was in cerebellopontine angle and jugular foramen meningioma and the highest probability in petroclival and clival meningiomas (in the list of locations* with its values—the higher the value is, the higher is the risk of a new neurologic deficit).
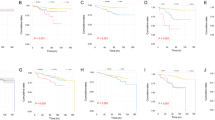
To build a ROC model, parameter volume was excluded because of non-significance (Wald criterion). Based on the results, a ROC model estimating the risk of a new neurologic deficit was compiled (area under the receiver operating characteristic curve (area) 0.74; SE 0.0284; 95% Wald confidence limits (0.69; 0.80); Somers’ D 0.49; gamma 0.49; tau-a 0.18; Fig. 1). These results were converted to a simple excel calculator attached (calculator 1—risk of a new neurologic deficit).
Risk score (below f (X)) = −2.1282 + 0.0289 × diameter (mm) + location ∗
*Location | |||
|---|---|---|---|
Cerebellopontine angle + jugular foramen | − 1.1002 | Middle cranial fossa | 0.2020 |
Sphenoid wing, lateral variant | − 0.9969 | Sphenoid wing, medial variant | 0.0000 |
Frontobasal | − 0.9789 | Cavernous sinus | 0.0571 |
Olfactory groove | − 0.7088 | Sphenoid wing, middle variant | 0.1872 |
Sella turcica + tuberculum sellae | − 0.4329 | Foramen magnum | 0.3805 |
Sphenoorbital | − 0.2768 | Petrous + posterior clinoid process | 1.7218 |
Planum sphenoidale | − 0.2290 | Petroclival + clival | 2.2125 |
The probability of a new neurologic deficit is then \(y=\frac{1}{1+{e}^{-f(X)}}\)
Postoperative decrease in KPS
According to univariate analysis (done by the logistic regression univariate model), factors associated with higher probability of a decrease in KPS at patient discharge were higher diameter, higher volume, presence of edema, infratentorial location, higher age, major artery contact, and lower GCS. Presence of hyperostosis and presence of capsular enhancement were associated with lower probability of a decrease in KPS. Considering the location and arachnoid cistern of origin, there were statistically significant differences in the risk of a decrease in KPS among the subgroups (see below).
Factors associated with higher probability of a decrease in KPS in multivariate analysis (done by the multivariate stepwise selection logistic regression model) were higher diameter (p < 0.0001), higher volume (p = 0.0909), higher patient age (p = 0.0213), and presence of dural tail (p = 0.0411). Conversely, presence of hyperostosis (p = 0.0367) was a protective factor. Concerning the location (p = 0.0008), the lowest probability of a decrease in KPS was in frontobasal meningiomas and the highest in petrous and posterior clinoid process meningiomas (in the list of locations** with its values—the higher the value is, the higher is risk of decrease in KPS).
To build a ROC model, the volume parameter was discarded because of non-significance (Wald criterion). Based on the statistical results, a ROC model estimating the risk of a postoperative decrease in KPS was established (area 0.80; SE 0.0289; 95% Wald confidence limits (0.74; 0.85); Somers’ D 0.59; gamma 0.59; tau-a 0.16; Fig. 2). These results were converted to a simple excel calculator attached (calculator 2—risk of a decrease in KPS).
Risks core (bellow f(X)) = − 6.2271 + 0.028 0 × age (years) + 0.0 514 × diameter (mm) + 0 .9781 x dural tail (0/1) − 1.3962 x hyperostosis(0/1) + location**
**Location | |||
|---|---|---|---|
Frontobasal | − 12.0078 | Planum sphenoidale | 0.4663 |
Sphenoid wing, lateral variant | − 1.1138 | Cavernous sinus | 0.9606 |
Olfactory groove | − 0.3455 | Sella turcica + tuberculum sellae | 1.7553 |
Middle cranial fossa | − 0.2336 | Sphenoorbital | 1.7941 |
Sphenoid wing, medial variant | 0 | Foramen magnum | 1.8534 |
Sphenoid wing, middle variant | 0.3612 | Petroclival + clival | 2.2055 |
Cerebellopontine angle + jugular foramen | 0.3976 | Petrous + posterior clinoid process | 3.0063 |
The probability of a decrease in KPS is then \(y=\frac{1}{1+{e}^{-f(X)}}\)
Based on the literature search, four articles and one chapter met the selection criteria for the scoring system predicting clinical outcome. Nine articles met the criteria for detecting general risk factors predicting the functional outcome in meningioma surgery. The selected references and their basic characteristics are summarized in Table 6.
Discussion
Surgical outcome is generally influenced by the patient’s comorbidities, age, presence of neurologic deficit, the size and location of the meningioma, and the experience, surgical strategy, and technique of the surgeon [9]. Individual predictive factors are the subject of several studies [5, 7, 8, 10,11,12,13,14,15]. and components of a few scoring systems [6, 16,17,18,19]. We analyzed the clinical outcome of SBM resection in 552 consecutive patients. KPS remained unchanged or increased in 84.8% and decreased in 15.2% of patients. Morbidity was 13.2% and surgery-related mortality was 1.3%. These results are consistent with the contemporary meningioma series with the reported rates of neurologic morbidity (3.9–13.7%) and mortality (0–5.4%) [5,6,7]. The preoperative risk factors were analyzed and ROC models estimating the risk of a new neurologic deficit and a decrease in KPS following SBM resection were developed.
In the following paragraphs, we review existing grading systems and compare them with the proposed ROC models. Finally, we provide a brief overview of the risk factors in meningioma surgery.
Grading systems predicting the functional outcome
The basic principle of medicine is that the benefits of treatment should far outweigh its risks [6]. To facilitate surgical decision-making, different grading systems are often applied in daily practice (e.g., Hunt-Hess classification, Spetzler-Martin classification, GCS) [19, 20, 27, 28]. The practical grading system should be simple, easy to recall, and provide a straightforward preoperative determination [16]. There are five grading systems predicting patient clinical outcomes following meningioma resection: the Levine-Sekhar grading system, the CLASS algorithm, the ABC Surgical Risk Scale, the Predictors of Severe Complications, and the Milan Complexity Scale [6, 16,17,18,19]. Selected grading systems with risk factors evaluated and relevant therapeutic recommendations are given in Table 6. Here, we summarize the predictive factors constituting individual scoring systems. Patient-related predictive factors are the patient’s age; [6, 17] comorbidities described by the ASA score; [6] KPS; [17] gravity of symptoms and signs; [6] and the presence of CN III, IV, or VI palsy [19]. Meningioma characteristics predicting the functional outcome are size, [6, 18] location, [6] multiple fossae or posterior fossa involvement, [18, 19] tumor position relative to the central cavity, [16] eloquent area involvement, [18] vessel encasement, [6, 19] CN group involvement, [16] contact with the brainstem, [16] and attachment size [16]. In some scales, previous progression, [6] surgical resection, [6, 16] or EBRT [16, 19] is taken into account. According to the total score achieved, grading scales stratify the patient on the risk of unfavorable clinical outcomes (decrease in KPS and GOS, neurologic deterioration, severe complications, etc.) and recommend therapeutic management.
Comparison of the ROC models estimating the functional outcome with grading systems
Compared to grading systems, predictive models ensure accurate outcome prediction and patient stratification. Instead of data categorization in the scoring systems, predictive models consider continuous variables (e.g., age, diameter) and their importance. Moreover, categorical data, such as meningioma location, could be more specific (exact location versus dichotomization SBM/nSBM). Although predictive models are often a complicated equation, they could be easily transformed into a surgeon-friendly Excel formula or a mobile phone application.
In this article we propose ROC models estimating the patient’s clinical outcome after SBM resection based on the following variables derived from multivariate stepwise selection analysis: patient age, meningioma size, location and presence of hyperostosis, and dural tail. A major advantage of our ROC models is that they are based on a multicentric study with a relatively large cohort (552 consecutive patients with SBM) compared to scoring systems with one exception based on single institutional retrospective studies with cohorts ranging from 132 to 979 patients [6, 16,17,18,19]. In addition, the models are designed for the most at-risk group of patients with surgically demanding SBM. Because the basic predictive variables (patient age, meningioma size, and location) in the studies mentioned are consistent, our models’ considerable convenience is that filling exact patient age, meningioma size, and anatomical location leads to more accurate patient stratification.
Higher age is a risk factor also included in the CLASS algorithm and in the risk of severe complication. While in our ROC model age is considered a continuous variable, in the scoring systems patients are categorized according to age into the risk groups ((≤ 60; 61–71; ≥ 71); (≤ 60; > 70)) [6, 17].
Similarly, the meningioma size included in our ROC models as continuous variable is relatively consistent risk factor considered in 4 out of 5 mentioned scoring system. In the Milan complexity scale, meningioma size ≥ 4.1 cm constitutes a risk factor [18]. Similarly, the ABC surgical risk scale defines three risk groups depending on the meningioma attachment size (< 2 cm; 2–4 cm; > 4 cm) [16]. In the Levine-Sekhar grading system, the risk factor is a presence of multiple fossa involvement [19]. Not quite in line with previous grading systems, the CLASS algorithm consider a higher diameter (≤ 2 cm; 2.1–4 cm; > 4 cm) not only a significant risk factors but also a benefit factor in favor of surgery. The authors’ explanation is the larger the tumor, the greater is the potential benefit for the patient following surgery [6].
The location of the meningioma is an important prognostic factor, but its definition varies significantly among the grading systems. In the CLASS algorithm, the locations are stratified as simple (convexity, lateral and middle sphenoid wing, posterior petrous), moderate (olfactory groove, planum sphenoidale, lateral and paramedian tentorial, parasagittal, intraventricular, cerebellopontine angle, falcine, posterior/lateral foramen magnum, para-sigmoid, and para-transverse sinus locations), and complex (clinoidal, cavernous sinus, tuberculum sellae, medial and incisural tentorial, ventral petrous, petroclival, and anterior/anterolateral foramen magnum) [6]. Adachi et al. in the ABC surgical risk scale define the risk groups by its relation to the central cavity as outside, partial involvement, and inside. The central cavity is the space encircled by the dural entry of CN II–XII [16]. The Milan complexity scale considers a risk factor the posterior fossa and eloquent area involvement [18]. Finally, our ROC models enabled accurate stratification of locations for surgical risk. Petroclival, clival, petrous, and the posterior clinoid process meningiomas were associated with unfavorable clinical outcomes, whereas frontobasal, cerebellopontine angle, and jugular foramen meningiomas with favorable clinical outcomes.
Another risk factors revealed by our ROC model was the presence of dural tail. Dural tail requires an extensive surgical resection with complicated dural repair and a higher risk of CSF leak and wound infection. The implication of dural tail is partly supported by a parameter attachment size from the ABC surgical risk scale, as it reflects both meningioma size and its dural tail [16].
The presence of hyperostosis was a positive prognostic factor in ROC model estimating the risk of a postoperative decrease in KPS. This parameter was statistically significant presumably because of the high prevalence of sphenoid wing and sphenoorbital meningiomas in our series (37.2%). These meningiomas represented 64.7% of tumors with hyperostosis. The presence of hyperostosis was a positive prognostic factor, as it was associated with a high rate of a preoperative neurologic deficit (69.8%) and thus a relatively low potential for clinical deterioration (decrease in KPS of 6.9%), even though another study described the association of hyperostosis with a higher risk of visual impairment [29].
Risk factors in meningioma surgery
Factors affecting the functional outcome of SBM resection could be divided into patient, tumor, and treatment related [9].
Patient-related factors
In line with previous studies, patient age is a well-known prognostic factor of the functional outcome in meningioma surgery [10, 14, 15]. Moreover, older age was associated with higher 30-day mortality, [7] risk of postoperative hematoma, [7] shorter OS, [30] and, in the present study, with a decrease in KPS. It is also a component of the CLASS algorithm by Lee et al. and of the predictors of severe complications by Bartek et al [6, 17].
In the literature, patient’s clinical condition (KPS, modified Rankin scale score, symptoms/signs, and comorbidities) is an important predictor of functional outcome. Bartek et al. documented an association of KPS < 70 with a higher risk of severe complications [17] and Lemée et al. of higher KPS with lower 30-day mortality and infection rate [7]. Similarly, Jenkins et al. reported that the rate of onset of focal neurological deficit or major adverse events was higher in patients with a higher modified Rankin scale score [5]. In contrast, preoperative KPS and neurologic deficit were not statistically significant predictive factors in our study. Inconsistent results were also reported for symptoms and signs. For instance, in the CLASS algorithm, more severe symptoms and signs favor surgery as they could be eventually alleviated [6]. In Meixensberger et al.’s study, CN palsy was associated with an unfavorable outcome, whereas intracranial hypertension, seizure, aphasia, or hemiparesis were associated with a favorable outcome [10]. In the Levine-Sekhar grading system, the CN III, IV, and VI palsies were negative predictive factors [19]. Comorbidities, frequently measured by the ASA score (not evaluated in the present study), are significant predictors of functional outcome in many studies [10, 12]. For instance, Lee et al. incorporated a higher ASA score as a negative predictor in the CLASS algorithm [6].
Patient sex is an inconsistent predictor of functional outcome. Lemée et al., for example, proved its association with neurologic outcome in recursive partitioning analysis, while Jenkins et al. did not [5, 7]. In our cohort, patient sex was not a significant predictor of clinical outcome in univariate or multivariate stepwise selection analysis. However, considering the OS female gender was associated with longer OS after meningioma surgery in French nationwide study [30].
Tumor-related factors
The most significant tumor-related risk factor is meningioma size. In the literature, meningioma size or even growth rate, described by several variables (e.g., diameter, dimensions, volume, surface, growth rate mm/year, or cm3/year), is considered an important predictor of functional outcome [11, 12]. Meningioma size, variably defined (multiple fossa involvement, [19] diameter, [6, 18] and attachment size [16]), is a component in 4 of 5 of the scoring systems described in this paper. Frequently, meningioma diameter (or attachment size) exceeding 2 or 4 cm is a significant predictor of unfavorable clinical outcomes [5, 6, 16, 18]. In our ROC models, larger meningioma diameter is associated with adverse clinical outcomes.
Another surgically relevant prognostic factor is meningioma location. For statistical analysis, meningioma location is frequently dichotomized (e.g., supra- versus infratentorial, [12] n-SBM versus SBM, [7, 8] and peripheral versus central [14]) the former being associated with a favorable outcome. In the different scoring systems of meningioma location complexity, [6] its relation to the central cavity [16] and multiple [19] or posterior fossa [18] involvement are considered. In contrast, our ROC models enabled accurate stratification of locations for surgical risk. Similarly, Scheitzach et al. reported significant differences in the improvement of the Medical Research Council Neurological Performance and KPS scores among the locations, with olfactory groove and lateral sphenoid wing meningiomas showing the best and foramen magnum meningiomas the worst functional outcomes [13]. According to multivariable analysis in French nationwide study by Champeaux-Depond et al., parasagittal and falx cerebri locations were associated with shorter OS [30].
Treatment-related factors
Previous surgical resection and irradiation are well-recognized risk factors associated with high morbidity and complication rates [6, 16, 19, 31, 32]. Considering reoperation for recurrent nSBM, patients with cognitive changes and meningiomas that overlap the middle third of the sagittal plane were at increased risk of complications [31]. In the reoperation of a recurrent SBM, posterior fossa location was significantly associated with complications [32]. In addition, according to multivariable analysis in French nationwide study, redo surgery and radiotherapy for recurrence were predictors of shorter OS [30].
Strengths and limitations
The main strengths of this study are its multicentric design and its relatively large cohort of patients. Moreover, all patients treated surgically for a meningioma within the study period were included, which avoids the problem of inclusion bias. Surgeries were performed in six neurosurgical departments within a geographically well-defined area with equal patient access to health care, thereby minimizing the risk of selection bias. A few Czech neurosurgical departments did not participate; therefore, the study does not meet the criterion of a national study. The major limitations are the retrospective nature of parts of the study, the relatively short postoperative follow-up, and the limited number of patients with SBM in rare locations (e.g., jugular foramen, tuberculum sellae, clivus).
Conclusion
An evidence-based therapeutic approach should be based on known risk factors, scoring systems, and predictive models. Predictive models allow rapid assessment of surgical risk, which could be compared to the natural history, SRS, EBRT, and combined approach, their efficacy, and complications. In addition to reviewing the basic literature, this article provides ROC models estimating the functional outcome of SBM resection based on patient age, meningioma size and location, and the presence of hyperostosis and dural tail. The next step is to validate the ROC models on a larger prospective patients’ cohort.
References
Ostrom QT, Gittleman H, Liao P, Rouse C, Chen Y, Dowling J, Wolinsky Y, Kruchko C, Barnholtz-Sloan J (2014) CBTRUS statistical report: primary brain and central nervous system tumors diagnosed in the United States in 2007-2011. Neuro-Oncology 16:iv1–iv63. https://doi.org/10.1093/neuonc/nou223
Goldbrunner R, Stavrinou P, Jenkinson MD, Sahm F, Mawrin C, Weber DC, Preusser M, Minniti G, Lund-Johansen M, Lefranc F, Houdart E, Sallabanda K, Le Rhun E, Nieuwenhuizen D, Tabatabai G, Soffietti R, Weller M (2021) EANO guideline on the diagnosis and management of meningiomas. Neuro-Oncol 23:1821–1834. https://doi.org/10.1093/neuonc/noab150
Sahm F, Schrimpf D, Stichel D, Jones DTW, Hielscher T, Schefzyk S, Okonechnikov K, Koelsche C, Reuss DE, Capper D, Sturm D, Wirsching H-G, Berghoff AS, Baumgarten P, Kratz A, Huang K, Wefers AK, Hovestadt V, Sill M et al (2017) DNA methylation-based classification and grading system for meningioma: a multicentre, retrospective analysis. Lancet Oncol 18:682–694. https://doi.org/10.1016/S1470-2045(17)30155-9
Louis DN, Perry A, Wesseling P, Brat DJ, Cree IA, Figarella-Branger D, Hawkins C, Ng HK, Pfister SM, Reifenberger G, Soffietti R, von Deimling A, Ellison DW (2021) The 2021 WHO Classification of Tumors of the Central Nervous System: a summary. Neuro-Oncology 23:1231–1251. https://doi.org/10.1093/neuonc/noab106
Jenkins FS, Vasella F, Padevit L, Mutschler V, Akeret K, Velz J, Regli L, Sarnthein J, Neidert MC (2021) Preoperative risk factors associated with new focal neurological deficit and other major adverse events in first-time intracranial meningioma neurosurgery. Acta Neurochir (Wien) 163:2871–2879. https://doi.org/10.1007/s00701-021-04897-x
Lee JH (2009) Meningiomas. Springer, London, London
Lemée J-M, Corniola MV, Da Broi M, Schaller K, Meling TR (2019) Early postoperative complications in meningioma: predictive factors and impact on outcome. World Neurosurg 128:e851–e858. https://doi.org/10.1016/j.wneu.2019.05.010
Meling TR, Da Broi M, Scheie D, Helseth E (2019) Meningiomas: skull base versus non-skull base. Neurosurg Rev 42:163–173. https://doi.org/10.1007/s10143-018-0976-7
Chen C-M, Huang AP-H, Kuo L-T, Tu Y-K (2011) Contemporary surgical outcome for skull base meningiomas. Neurosurg Rev 34:281–296. https://doi.org/10.1007/s10143-011-0321-x
Meixensberger J, Meister T, Janka M, Haubitz B, Bushe KA, Roosen K (1996) Factors influencing morbidity and mortality after cranial meningioma surgery — a multivariate analysis. In: Fahlbusch R, Bock WJ, Brock M, Buchfelder M, Klinger M (eds) Modern Neurosurgery of Meningiomas and Pituitary Adenomas. Springer Vienna, Vienna, pp 99–101
Miao Y, Lu X, Qiu Y, Jiang J, Lin Y (2010) A multivariate analysis of prognostic factors for health-related quality of life in patients with surgically managed meningioma. J Clin Neurosci 17:446–449. https://doi.org/10.1016/j.jocn.2009.07.111
Raman SG, Prakash P, Sumit J, Bikram SD, Prasanna K (2021) Clinical outcome and recurrence after meningioma surgery: an experience from a developing country, Nepal. World Neurosurg 148:e138–e144. https://doi.org/10.1016/j.wneu.2020.12.079
Scheitzach J, Schebesch K-M, Brawanski A, Proescholdt MA (2014) Skull base meningiomas: neurological outcome after microsurgical resection. J Neurooncol 116:381–386. https://doi.org/10.1007/s11060-013-1309-x
Splavski B, Hadzic E, Bagic I, Vrtaric V, Splavski B (2017) Simple tumor localization scale for estimating management outcome of intracranial meningioma. World Neurosurg 104:876–882. https://doi.org/10.1016/j.wneu.2017.05.039
Zeng L, Wang L, Ye F, Chen J, Lei T, Chen J (2015) Clinical characteristics of patients with asymptomatic intracranial meningiomas and results of their surgical management. Neurosurg Rev 38:481–488. https://doi.org/10.1007/s10143-015-0619-1
Adachi K, Kawase T, Yoshida K, Yazaki T, Onozuka S (2009) ABC Surgical Risk Scale for skull base meningioma: a new scoring system for predicting the extent of tumor removal and neurological outcome: Clinical article. JNS 111:1053–1061. https://doi.org/10.3171/2007.11.17446
Bartek J, Sjåvik K, Förander P, Solheim O, Gulati S, Weber C, Ingebrigtsen T, Jakola AS (2015) Predictors of severe complications in intracranial meningioma surgery: a population-based multicenter study. World Neurosurg 83:673–678. https://doi.org/10.1016/j.wneu.2015.01.022
Ferroli P, Broggi M, Schiavolin S, Acerbi F, Bettamio V, Caldiroli D, Cusin A, La Corte E, Leonardi M, Raggi A, Schiariti M, Visintini S, Franzini A, Broggi G (2015) Predicting functional impairment in brain tumor surgery: the Big Five and the Milan Complexity Scale. FOC 39:E14. https://doi.org/10.3171/2015.9.FOCUS15339
Levine ZT, Buchanan RI, Sekhar LN, Rosen CL, Wright DC (1999) Proposed grading system to predict the extent of resection and outcomes for cranial base meningiomas. Neurosurgery 45:221–229. https://doi.org/10.1097/00006123-199908000-00003
Teasdale G, Jennett B (1974) Assessment of coma and impaired consciousness. Lancet 304:81–84. https://doi.org/10.1016/S0140-6736(74)91639-0
Karnofsky DA, Abelmann WH, Craver LF, Burchenal JH (1948) The use of the nitrogen mustards in the palliative treatment of carcinoma. With particular reference to bronchogenic carcinoma. Cancer 1:634–656. https://doi.org/10.1002/1097-0142(194811)1:4<634::AID-CNCR2820010410>3.0.CO;2-L
Simpson D (1957) The recurrence of intracranial meningiomas after surgical treatment. J Neurol, Neurosurg Psychiatry 20:22–39. https://doi.org/10.1136/jnnp.20.1.22
Louis DN, Ohgaki H, Wiestler OD, Cavenee WK, Burger PC, Jouvet A, Scheithauer BW, Kleihues P (2007) The 2007 WHO Classification of Tumours of the Central Nervous System. Acta Neuropathol 114:97–109. https://doi.org/10.1007/s00401-007-0243-4
Louis DN, Perry A, Reifenberger G, von Deimling A, Figarella-Branger D, Cavenee WK, Ohgaki H, Wiestler OD, Kleihues P, Ellison DW (2016) The 2016 World Health Organization Classification of Tumors of the Central Nervous System: a summary. Acta Neuropathol 131:803–820. https://doi.org/10.1007/s00401-016-1545-1
Jennett B, Bond M (1975) Assessment of outcome after severe brain damage. Lancet 1:480–484. https://doi.org/10.1016/s0140-6736(75)92830-5
Landriel Ibañez FA, Hem S, Ajler P, Vecchi E, Ciraolo C, Baccanelli M, Tramontano R, Knezevich F, Carrizo A (2011) A new classification of complications in neurosurgery. World Neurosurg 75:709–715; discussion 604-611. https://doi.org/10.1016/j.wneu.2010.11.010
Hunt WE, Hess RM (1968) Surgical risk as related to time of intervention in the repair of intracranial aneurysms. J Neurosurg 28:14–20. https://doi.org/10.3171/jns.1968.28.1.0014
Spetzler RF, Martin NA (1986) A proposed grading system for arteriovenous malformations. J Neurosurg 65:476–483. https://doi.org/10.3171/jns.1986.65.4.0476
Zamanipoor Najafabadi AH, Genders SW, van Furth WR (2021) Visual outcomes endorse surgery of patients with spheno-orbital meningioma with minimal visual impairment or hyperostosis. Acta Neurochir 163:73–82. https://doi.org/10.1007/s00701-020-04554-9
Champeaux-Depond C, Weller J, Froelich S, Resche-Rigon M (2021) A nationwide population-based study on overall survival after meningioma surgery. Cancer Epidemiol 70:101875. https://doi.org/10.1016/j.canep.2020.101875
Magill ST, Dalle Ore CL, Diaz MA, Jalili DD, Raleigh DR, Aghi MK, Theodosopoulos PV, McDermott MW (2019) Surgical outcomes after reoperation for recurrent non–skull base meningiomas. J Neurosurg 131:1179–1187. https://doi.org/10.3171/2018.6.JNS18118
Magill ST, Lee DS, Yen AJ, Lucas C-HG, Raleigh DR, Aghi MK, Theodosopoulos PV, McDermott MW (2019) Surgical outcomes after reoperation for recurrent skull base meningiomas. J Neurosurg 130:876–883. https://doi.org/10.3171/2017.11.JNS172278
Funding
Supported by Ministry of Health of the Czech Republic, grant nr. 15 - NV19-04-00272. Supported by MO 1012 and Cooperation. Open access publishing supported by the National Technical Library in Prague.
Author information
Authors and Affiliations
Contributions
Michaela May: substantial contributions to the conception or design of the study, data acquisition, and drafting of the manuscript. Vojtech Sedlak and Jozef Malik: substantial contributions to the conception or design of the study and radiologic evaluation of the imaging studies; final approval of the version to be published. Ladislav Pecen: statistical analysis and interpretation of the results; final approval of the version to be published. Vladimir Priban, Pavel Buchvald, Jiri Fiedler, Miroslav Vaverka, Radim Lipina, and Stefan Reguli: substantial contributions to the conception or design of the study and the data acquisition; final approval of the version to be published. David Netuka: substantial contributions to the study design, revising the manuscript critically for important intellectual content, and final approval of the version to be published. Vladimir Benes: substantial contributions to the study design, revising the manuscript critically for important intellectual content, and final approval of the version to be published.
Corresponding author
Ethics declarations
Ethics approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the Ethical Committee of University Hospital in Ostrava (reference number 530/2018) and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Consent to participate
General informed consent to the use of the anonymized data for research purposes was obtained from all individual participants included in the study.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Key messages
What is already known on this topic:
If the principles of evidence-based medicine on meningioma surgery are to be applied, it is crucial to define the preoperative risk factors and build reliable models predicting the functional outcome. However, only a few scoring systems exist so far.
What this study adds:
In the present study, the ROC models estimating the functional outcome based on preoperative risk factors were built.
How this study might affect research, practice, or policy:
Future studies should refine the available models on larger prospective patient cohorts and identify reliable qualitative and quantitative risk factors.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
May, M., Sedlak, V., Pecen, L. et al. Role of risk factors, scoring systems, and prognostic models in predicting the functional outcome in meningioma surgery: multicentric study of 552 skull base meningiomas. Neurosurg Rev 46, 124 (2023). https://doi.org/10.1007/s10143-023-02004-5
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10143-023-02004-5